Introduction to Gamma Knife Radiosurgery
Gamma Knife Radiosurgery (GKR) is a groundbreaking, minimally invasive procedure designed to treat brain disorders without the need for traditional open surgery. Despite the term "knife," this technique involves no surgical incision. Instead, it uses highly focused gamma radiation beams to target abnormal tissue, such as brain tumors, arteriovenous malformations (AVMs), and certain functional disorders like trigeminal neuralgia.
Developed in the mid-20th century and continually refined through modern technology, the Gamma Knife has revolutionized the way neurosurgeons manage brain conditions that once required complex, high-risk open surgeries. The precision of this system - capable of targeting lesions smaller than a few millimeters - ensures that only the diseased tissue receives high-dose radiation while surrounding healthy brain tissue is preserved.
The procedure is performed under local anesthesia or mild sedation, typically on an outpatient basis, meaning patients can often return home the same day. It is especially valuable for treating deep-seated or surgically inaccessible brain lesions, offering an exceptional level of safety and accuracy.
In contemporary neuro-oncology, the Gamma Knife has become an essential treatment option - combining the accuracy of microsurgery, the effectiveness of radiation therapy, and the comfort of a non-invasive technique.
Causes and Risk Factors of Conditions Treated with Gamma Knife
The Gamma Knife itself is not a cause or disease; it is a treatment modality used to address a range of neurological and vascular disorders. Understanding the causes and risk factors of these underlying conditions helps explain why Gamma Knife treatment becomes necessary.
A. Common Conditions Treated by Gamma Knife
-
Brain Tumors
Both benign (non-cancerous) and malignant (cancerous) tumors can be effectively treated. Examples include:-
Meningiomas (tumors of the brain lining)
-
Acoustic neuromas (affecting hearing and balance)
-
Metastatic brain tumors (secondary cancer spread)
-
Pituitary adenomas (hormone-producing tumors)
-
-
Arteriovenous Malformations (AVMs)
These are tangled masses of blood vessels in the brain that disrupt normal circulation and can lead to hemorrhage. Gamma Knife therapy helps close off these vessels gradually, reducing the risk of bleeding. -
Functional Neurological Disorders
Certain disorders related to nerve function, such as trigeminal neuralgia (severe facial pain) and Parkinson's tremors, can be treated by targeting specific brain regions responsible for abnormal activity. -
Recurrent Lesions or Post-Surgical Residue
In cases where tumors recur after surgery or radiotherapy, Gamma Knife serves as a precise, repeatable, and minimally invasive alternative.
B. Risk Factors for Developing These Conditions
-
Genetic predispositions: Certain hereditary syndromes increase the risk of brain tumor formation.
-
Radiation exposure: Prior exposure to high-dose radiation can predispose individuals to secondary tumors.
-
Age: Older adults have higher risks for meningiomas, metastases, and vascular malformations.
-
Environmental factors: Long-term exposure to chemicals, smoking, and stress may play indirect roles.
-
Other medical conditions: Chronic hypertension, autoimmune disorders, or infections can contribute to vascular or neoplastic changes in the brain.
Understanding these risks allows for early diagnosis and timely intervention - where Gamma Knife may serve as a curative or palliative measure.
Symptoms and Signs of Conditions Requiring Gamma Knife Treatment
The symptoms prompting consideration for Gamma Knife vary depending on the underlying disease but generally relate to pressure effects on brain structures or abnormal neural function.
A. Common Neurological Symptoms
-
Persistent Headaches: Often described as localized, worsening over time, or unresponsive to medication.
-
Seizures: New-onset seizures in adults often point toward an underlying lesion such as a tumor or AVM.
-
Vision Problems: Blurred vision, double vision, or partial loss of sight may indicate pressure on optic nerves.
-
Hearing Loss or Tinnitus: Common in acoustic neuroma cases.
-
Facial Pain or Numbness: A hallmark of trigeminal neuralgia or skull-base lesions.
-
Weakness or Coordination Issues: Result from pressure on motor or balance centers.
-
Cognitive and Personality Changes: Common in frontal or temporal lobe lesions.
B. Symptoms of Vascular Lesions (AVMs)
-
Sudden severe headache ("thunderclap headache")
-
Nausea and vomiting
-
Neurological deficits due to minor hemorrhage or chronic ischemia
C. Functional Disorders
-
Electric shock-like pain along the face (trigeminal neuralgia)
-
Tremors or stiffness in Parkinson's disease
Recognizing these warning signs and seeking early evaluation ensures safer and more successful outcomes through radiosurgical intervention.
Diagnosis and Evaluation Before Gamma Knife Treatment
Accurate diagnosis and treatment planning are the foundation of successful Gamma Knife radiosurgery. The process involves advanced imaging, interdisciplinary consultation, and individualized treatment mapping.
A. Diagnostic Procedures
-
Magnetic Resonance Imaging (MRI): The gold standard for identifying tumors, vascular anomalies, and nerve compression.
-
Computed Tomography (CT) Scan: Provides detailed bone and vascular structure imaging.
-
Angiography: Used to visualize abnormal blood vessels in AVMs.
-
Positron Emission Tomography (PET): Helps assess tumor metabolism and growth activity.
-
Functional MRI (fMRI): Maps brain activity and helps surgeons avoid critical areas during treatment.
B. Clinical Evaluation
-
Neurological Examination: Tests coordination, strength, reflexes, and sensory response.
-
Endocrine Assessment: For pituitary tumors, hormone levels are measured to assess functional impact.
-
Multidisciplinary Discussion: Neurosurgeons, radiation oncologists, and physicists collaboratively design a personalized treatment plan.
The data from these assessments guide precise targeting and dose calibration during Gamma Knife therapy.
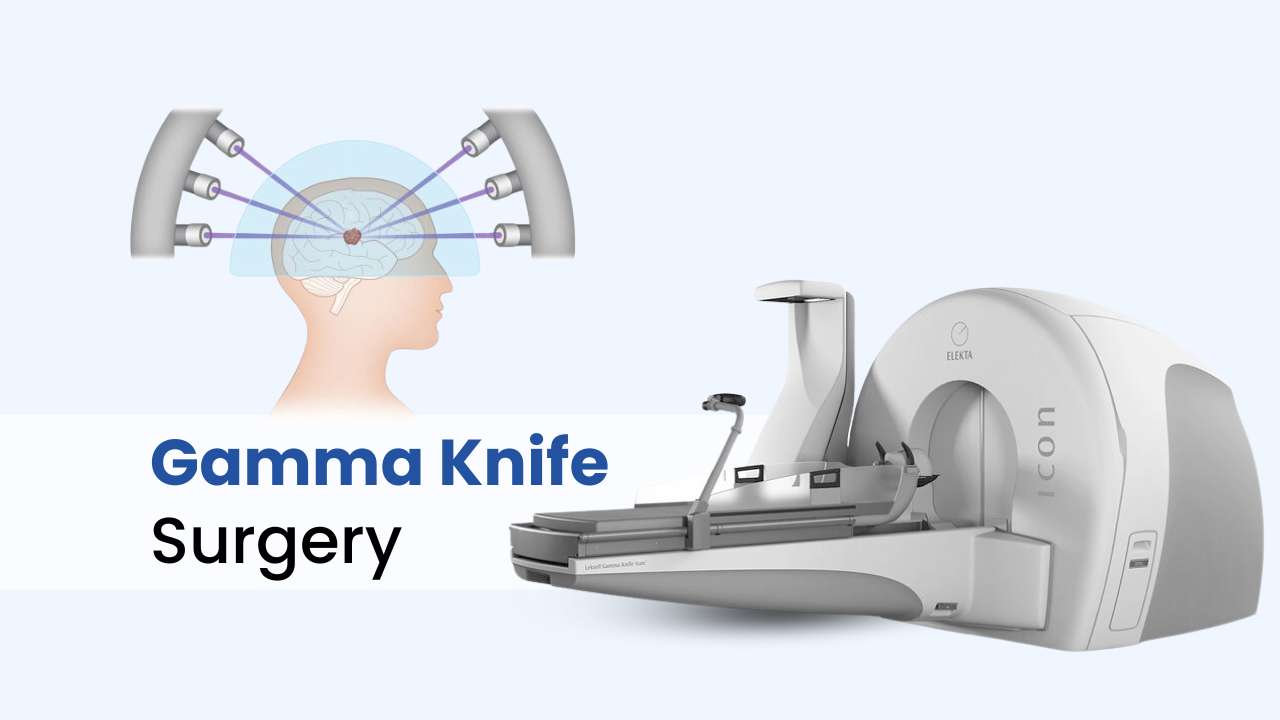
Treatment Options: The Gamma Knife Procedure
The Gamma Knife procedure is a highly precise form of stereotactic radiosurgery-using focused beams of gamma radiation to treat brain tumors, vascular malformations, and certain other brain conditions without an incision. It's preferred for patients with lesions in sensitive or hard-to-reach brain areas, offering an alternative to open surgery with less risk and minimal recovery time.
A. Preparation and Planning
-
The patient's head is immobilized using a stereotactic frame (or mask in newer systems) to ensure sub-millimeter accuracy.
-
High-resolution scans are performed to map the lesion and nearby vital structures.
-
The medical team uses specialized software to calculate radiation dosage and beam trajectory - ensuring maximum focus on the lesion while preserving normal brain tissue.
B. The Procedure Step-by-Step
-
Positioning: The patient lies on a treatment couch that slides into the Gamma Knife unit.
-
Radiation Delivery: Around 192 precisely focused cobalt-60 gamma beams converge at the target point, delivering an intense dose to the abnormal tissue.
-
Duration: The procedure lasts from 30 minutes to 2 hours, depending on target size and complexity.
-
Monitoring: Throughout the process, patients remain conscious and communicate with the medical team via intercom.
-
Post-Procedure: The stereotactic frame is removed, and most patients can return home the same day.
C. Advantages of Gamma Knife
-
No incision, no bleeding, no anesthesia risks
-
Outpatient procedure with minimal recovery time
-
High success rates for small to medium-sized brain lesions
-
Lower risk of infection or neurological deficit compared to open surgery
Prevention and Management After Gamma Knife Radiosurgery
Prevention and management after Gamma Knife radiosurgery focus on minimizing acute and delayed side effects, monitoring for complications, and supporting patient recovery through education, follow-up, and symptom management.
A. Preventive Strategies
Although one cannot always prevent brain tumors or AVMs, risk reduction involves:
-
Controlling blood pressure and cardiovascular health.
-
Avoiding unnecessary radiation exposure.
-
Maintaining a healthy lifestyle with adequate sleep, nutrition, and exercise.
-
Regular medical checkups for individuals with genetic or familial predispositions.
B. Post-Treatment Management
-
Observation and Rest: Mild headache or fatigue may occur for 24-48 hours; rest is recommended.
-
Medication: Steroids may be prescribed to prevent brain swelling, and anticonvulsants for seizure prevention.
-
Follow-Up Imaging: MRI scans at 3, 6, and 12 months assess lesion shrinkage or obliteration.
-
Symptom Monitoring: Report new neurological changes immediately to your doctor.
Long-term management includes lifestyle adaptation, routine evaluations, and, in some cases, ongoing medication.
Complications of Gamma Knife Treatment
While the Gamma Knife is highly precise and safe, no medical procedure is entirely free of risk.
A. Short-Term Complications
-
Headache and Scalp Soreness: Usually mild and temporary.
-
Swelling or Redness: Around the stereotactic frame points.
-
Fatigue or Nausea: Due to brief radiation exposure.
B. Delayed Complications
-
Radiation Edema: Temporary swelling around treated tissue that can cause mild symptoms, managed with steroids.
-
Radiation Necrosis: Rare tissue death that may appear months later, often treated conservatively.
-
Neurological Symptoms: Rarely, transient weakness or numbness due to localized inflammation.
-
Incomplete Treatment Response: Some tumors or AVMs may require repeat radiosurgery or adjunct therapy.
With modern imaging and dose planning, the rate of serious complications remains below 2-3%, making Gamma Knife one of the safest neurosurgical options available.
Living with the Condition After Gamma Knife Radiosurgery
Recovery from Gamma Knife radiosurgery is generally rapid, and most patients resume their regular routines within a few days. However, maintaining a long-term care plan ensures lasting health and stability.
A. Immediate Recovery
-
Resume light activities within 24 hours.
-
Avoid strenuous exercise for 3-5 days.
-
Maintain hydration and balanced nutrition.
-
Follow prescribed medications exactly as instructed.
B. Long-Term Living and Lifestyle
-
Regular neurological checkups every 6-12 months.
-
Continued MRI surveillance for at least 2-3 years post-procedure.
-
Adopt a neuroprotective lifestyle - healthy diet, stress control, avoiding tobacco and excessive alcohol.
-
Engage in light aerobic exercise and cognitive activities to promote brain health.
C. Emotional and Psychological Health
Undergoing brain treatment can be emotionally challenging. Counseling, support groups, or therapy can help patients adapt and cope with post-treatment anxiety or fear of recurrence.
In most cases, Gamma Knife patients experience remarkable quality-of-life improvement, reduced symptoms, and excellent long-term control of their condition.
Top 10 Frequently Asked Questions about Gamma Knife Surgery
1. What is Gamma Knife Surgery?
Gamma Knife Surgery is a non-invasive radiosurgical
procedure used to treat brain disorders such as tumors, arteriovenous
malformations (AVMs), and functional conditions like trigeminal neuralgia. Despite its
name, it's not an actual knife or surgical incision.
The procedure uses highly focused beams of gamma radiation to precisely
target abnormal tissue in the brain while sparing the surrounding healthy tissue.
2. What conditions can be treated with Gamma Knife?
Gamma Knife radiosurgery is used to treat a variety of brain conditions, including:
-
Brain tumors (benign and malignant)
-
Metastatic brain tumors (cancer spread from other organs)
-
Arteriovenous malformations (AVMs)
-
Trigeminal neuralgia (chronic facial pain)
-
Acoustic neuroma (vestibular schwannoma)
-
Meningioma
-
Pituitary adenoma
-
Certain forms of epilepsy and Parkinson's disease
It is particularly beneficial when traditional surgery is risky or not possible.
3. How does Gamma Knife Surgery work?
Gamma Knife uses focused gamma radiation from multiple angles to deliver
a high dose to a specific brain target. Each individual beam is weak
and harmless as it passes through healthy tissue, but they converge precisely at the
target area to destroy or shrink abnormal cells.
This allows the treatment to be painless, bloodless, and extremely
accurate - typically within 0.3 mm precision.
4. How is Gamma Knife Surgery performed?
Here's what to expect during the procedure:
-
The patient's head is fitted with a lightweight stereotactic frame (for accuracy).
-
MRI or CT scans are taken to pinpoint the exact target area in the brain.
-
A computer plan is created to focus radiation precisely on the target.
-
The patient lies on the treatment couch, and the Gamma Knife machine delivers radiation beams for 30 minutes to 2 hours.
-
The patient can usually go home the same day.
The entire process is painless, and no surgical incision or anesthesia (beyond local numbing) is required.
5. Is Gamma Knife Surgery painful?
No. Gamma Knife surgery is completely painless.
You may feel slight pressure when the head frame is attached, but the procedure itself
causes no discomfort. Most patients remain awake and
relaxed throughout treatment.
6. What are the advantages of Gamma Knife Surgery?
Key benefits include:
-
Non-invasive and bloodless (no incision or stitches)
-
No need for general anesthesia
-
Minimal side effects and short recovery time
-
High precision targeting minimizes damage to healthy tissue
-
Outpatient procedure - patients usually go home the same day
-
Excellent long-term control rates for many brain disorders
It's often a safer alternative to traditional open brain surgery.
7. What are the possible side effects or risks?
While Gamma Knife is very safe, some patients may experience:
-
Mild headache or nausea (temporary)
-
Scalp tenderness or swelling at frame sites
-
Fatigue for a few days after treatment
-
Delayed effects such as swelling in the treated area (edema)
-
Rare complications like radiation necrosis or hair loss in localized areas
Your medical team will discuss all potential risks and provide medications if needed.
8. How long does recovery take after Gamma Knife Surgery?
Recovery is typically quick:
-
Return home: The same day
-
Resume normal activities: Within 24-48 hours
-
Follow-up MRI or CT scan: Usually within 6-12 weeks to monitor treatment response
Since there's no incision or anesthesia recovery, most patients can return to work or normal life within a day or two.
9. How successful is Gamma Knife Surgery?
Gamma Knife has an exceptional success rate, depending on the condition treated:
-
Benign tumors: 90-95% tumor control rate
-
Metastatic tumors: 85-90% shrinkage or control
-
Trigeminal neuralgia: 70-90% long-term pain relief
-
AVMs: 80-90% eventual closure rate (within 2-3 years)
It's one of the most effective and precise radiosurgery techniques available worldwide.
10. Who is a suitable candidate for Gamma Knife Surgery?
You may be a good candidate if you:
-
Have a small to medium-sized brain tumor or lesion
-
Cannot undergo open surgery due to health risks
-
Need a precise, non-invasive treatment for a brain condition
-
Are looking for a short recovery, outpatient procedure
Your neurosurgeon or radiation oncologist will review imaging results and medical history to determine suitability.


