Introduction to Gastric Bypass Surgery
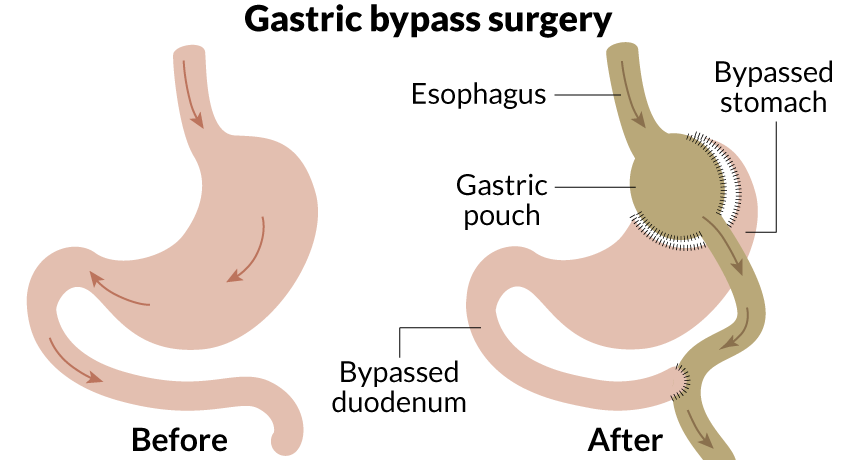
Gastric Bypass Surgery, medically known as Roux-en-Y Gastric Bypass (RYGB), is one of the most effective and commonly performed bariatric (weight-loss) procedures worldwide. It is designed to help individuals suffering from severe obesity and related metabolic disorders when other non-surgical treatments-such as diet, exercise, and medication-have failed. The surgery works through two primary mechanisms: restriction and malabsorption. First, the stomach is divided into a small upper pouch, drastically reducing food intake capacity. Second, part of the small intestine is rerouted (bypassed), which limits the absorption of calories and nutrients. This dual action leads to substantial and sustainable weight loss, typically resulting in the loss of 60-80% of excess body weight within the first 12 to 18 months after surgery.
Beyond weight reduction, gastric bypass surgery has a profound impact on metabolic health. It can induce remission of Type 2 diabetes, reduce blood pressure, improve cholesterol levels, alleviate obstructive sleep apnea, and decrease the risk of heart disease and stroke. The procedure is generally performed using laparoscopic (keyhole) techniques, which involve several small incisions instead of one large one, allowing faster recovery and fewer complications.
Gastric bypass is not merely a cosmetic intervention-it is a life-saving, metabolic operation. It redefines the body's digestive physiology and often transforms patients' physical, emotional, and psychological well-being. However, it requires a lifelong commitment to dietary discipline, regular medical follow-up, and nutritional supplementation to ensure long-term success and prevent deficiencies.
Causes and Risks Leading to Gastric Bypass Surgery
The main causes and risk factors leading to gastric bypass surgery are severe obesity (high body mass index, BMI) and its related health complications-especially after non-surgical weight loss approaches have failed. The procedure is designed to help with significant, sustained weight loss and to reduce the risk of life-threatening obesity-related conditions.
A. Causes / Indications for Surgery
Gastric Bypass is primarily indicated for patients with morbid obesity, typically defined as a Body Mass Index (BMI) of 40 or higher, or BMI of 35 or higher accompanied by serious obesity-related health problems. These health problems may include:
-
Type 2 Diabetes Mellitus - Uncontrolled blood sugar due to insulin resistance.
-
Hypertension (High Blood Pressure) - Persistent elevation of blood pressure linked to obesity.
-
Dyslipidemia - High cholesterol and triglyceride levels.
-
Sleep Apnea - Recurrent pauses in breathing during sleep caused by airway obstruction.
-
Severe Gastroesophageal Reflux Disease (GERD) - Chronic acid reflux damaging the esophagus.
-
Osteoarthritis and Joint Pain - Caused by excess weight burdening joints.
-
Polycystic Ovary Syndrome (PCOS) - In women, leading to infertility and hormonal imbalance.
In short, gastric bypass is recommended when lifestyle modification and pharmacotherapy fail and when obesity poses a significant threat to health and life expectancy.
B. Risk Factors for Obesity Requiring Surgery
Obesity is a multifactorial disease influenced by genetic, environmental, hormonal, and behavioral factors. Some key risks include:
-
Genetics: Family history of obesity or metabolic disorders increases susceptibility.
-
Dietary Habits: High consumption of calorie-dense, processed foods and sugary beverages.
-
Sedentary Lifestyle: Lack of physical activity slows metabolism.
-
Hormonal Imbalances: Conditions like hypothyroidism, Cushing's syndrome, or leptin resistance.
-
Psychological Stress & Depression: Emotional eating and poor sleep can trigger weight gain.
-
Medications: Certain drugs such as antidepressants, corticosteroids, and antipsychotics.
-
Socioeconomic Factors: Limited access to healthy food, education, and healthcare.
These factors, when combined, can result in obesity that becomes resistant to conservative interventions-necessitating surgical management through gastric bypass.
Symptoms and Signs Leading to Gastric Bypass Consideration
Patients who are candidates for gastric bypass usually experience multiple physical, metabolic, and psychological symptoms due to obesity. These symptoms significantly impair quality of life and overall health.
A. Physical Symptoms
-
Shortness of Breath: Even with minimal exertion, caused by excess body mass.
-
Chronic Fatigue: Reduced energy due to metabolic inefficiency.
-
Joint and Back Pain: Overload on bones and ligaments.
-
Snoring and Sleep Disturbance: Obstructive sleep apnea leads to poor sleep quality.
-
Recurrent Skin Infections: Especially in skin folds due to moisture and friction.
B. Metabolic and Internal Symptoms
-
Uncontrolled Diabetes: Persistent high blood sugar despite medication.
-
High Blood Pressure: Frequently associated with obesity-induced vascular changes.
-
GERD and Digestive Discomfort: Due to abdominal pressure and reflux.
-
Irregular Menstrual Cycles and Infertility: Common in women with PCOS and obesity.
C. Psychological Symptoms
-
Low Self-Esteem and Depression: Due to social stigma and self-image issues.
-
Social Withdrawal and Anxiety: Fear of judgment, leading to isolation.
-
Emotional Eating: Using food as a coping mechanism for stress or sadness.
These symptoms, collectively, can be debilitating and create a cycle of physical limitation, emotional stress, and worsening obesity, making surgical intervention a necessary step toward recovery.
Diagnosis and Preoperative Evaluation for Gastric Bypass Surgery
Before undergoing gastric bypass, patients must go through a comprehensive evaluation to confirm eligibility, optimize health, and minimize surgical risk.
A. Diagnostic Tests and Assessment
-
BMI and Obesity Classification: Determines surgical candidacy (usually BMI ≥35 with comorbidities).
-
Laboratory Tests: Includes blood sugar, HbA1c, liver and kidney function, cholesterol profile, and complete blood count.
-
Endoscopy: Checks for ulcers, gastritis, or hernias.
-
Ultrasound or CT Scan: Evaluates abdominal organs and fat distribution.
-
Sleep Study: Detects sleep apnea requiring management before surgery.
-
Cardiac Evaluation: ECG, echocardiogram, and stress test for cardiac risk assessment.
B. Psychological and Nutritional Evaluation
-
Mental Health Assessment: Ensures emotional readiness and the absence of eating disorders or uncontrolled depression.
-
Dietitian Consultation: Reviews current eating habits and prepares the patient for post-surgery dietary changes.
-
Lifestyle Commitment Discussion: Clarifies the lifelong requirement for exercise, follow-up visits, and supplementation.
Only patients who demonstrate physical and psychological readiness, understanding, and commitment to the post-surgical lifestyle are approved for gastric bypass.
Treatment Options and The Gastric Bypass Procedure
The main treatment option for significant, medically-complicated obesity is gastric bypass surgery, most commonly the Roux-en-Y gastric bypass. This is a minimally invasive procedure performed laparoscopically in most cases. The goal is to reduce stomach size and reroute the digestive tract to induce safe, effective, and long-lasting weight loss.
A. Surgical Procedure Explained
Roux-en-Y Gastric Bypass involves the following steps:
-
Creation of a Small Pouch: The stomach is divided into a small upper pouch (approximately 30 ml) and a larger lower section, which is bypassed.
-
Intestinal Rerouting: A segment of the small intestine (jejunum) is connected directly to the new pouch, allowing food to bypass part of the digestive tract.
-
Dual Mechanism: This combination reduces stomach capacity (restrictive) and nutrient absorption (malabsorptive).
The surgery is performed laparoscopically, meaning smaller incisions, less pain, faster healing, and minimal scarring. Hospital stay averages 1-3 days, and patients can return to work within 2-3 weeks.
B. Expected Outcomes
-
Average weight loss of 60-80% of excess body weight within 1-2 years.
-
Resolution or improvement of diabetes, hypertension, and sleep apnea.
-
Long-term reduction in cardiovascular risk.
-
Enhanced mobility, mental health, and fertility.
C. Other Surgical Alternatives
-
Sleeve Gastrectomy: Removes 80% of the stomach but keeps the intestine intact.
-
Adjustable Gastric Banding: Uses a silicone band to restrict stomach size.
-
Biliopancreatic Diversion: A more complex version for extremely high BMI cases.
Gastric bypass remains the gold standard due to its balance between safety, effectiveness, and long-term metabolic benefits.
Prevention and Postoperative Management
Prevention and postoperative management after gastric bypass surgery are critical to maximize weight loss, avoid complications like dumping syndrome, and ensure long-term health. Careful adherence to dietary, lifestyle, medication, and follow-up protocols is essential.
A. Prevention Before Surgery
-
Adopt Healthy Eating Habits Early: Emphasize portion control, high protein, and low fat.
-
Regular Physical Activity: Improves heart health and surgical outcomes.
-
Control of Existing Diseases: Proper diabetes and blood pressure management reduces complications.
B. Post-Surgical Management
-
Diet Progression:
-
Week 1-2: Liquids only (broths, protein shakes).
-
Week 3-4: Pureed and soft foods.
-
After 4 weeks: Gradual reintroduction of solid foods in small portions.
-
-
Vitamin and Mineral Supplements: Lifelong use of B12, calcium, vitamin D, and iron.
-
Regular Follow-ups: Every 3-6 months for the first year, then annually.
-
Behavioral Therapy: Helps prevent emotional eating and weight regain.
Proper postoperative care ensures successful recovery, sustained weight loss, and long-term health improvement.
Complications of Gastric Bypass Surgery
Complications after gastric bypass surgery are generally divided into early (within 30 days) and late (after one month), encompassing both surgical and long-term metabolic/nutritional risks. While most complications are manageable, some require urgent recognition and intervention to avoid severe outcomes.
A. Early Complications (within 30 days)
-
Bleeding or Infection: Managed with antibiotics and supportive care.
-
Anastomotic Leak: Leakage from intestinal joins, requiring immediate medical attention.
-
Blood Clots: Prevented with early ambulation and blood thinners.
-
Anesthesia Reactions: Rare but possible.
B. Long-Term Complications
-
Nutritional Deficiencies: Iron, B12, folate, calcium, and vitamin D shortages can lead to anemia and osteoporosis.
-
Dumping Syndrome: Rapid gastric emptying after high-sugar foods causing nausea, sweating, and palpitations.
-
Gallstones: Due to rapid weight loss.
-
Stomal Stenosis: Narrowing of the new stomach outlet causing vomiting.
-
Weight Regain: If dietary and lifestyle guidelines are not followed.
Despite these, the overall success rate exceeds 95%, and serious complications are rare with proper follow-up.
Living with Gastric Bypass Surgery
Life after gastric bypass represents a new beginning, both physically and emotionally. Patients experience profound improvements in their health, energy, and confidence-but only when they fully embrace lifelong changes.
A. Diet and Nutrition
-
Eat small, frequent meals with high protein and low fat/sugar.
-
Avoid carbonated drinks, alcohol, and fried foods.
-
Stay hydrated but avoid drinking during meals.
-
Take daily prescribed vitamins and supplements.
B. Lifestyle and Physical Activity
-
Engage in 30-60 minutes of daily exercise, including walking, cycling, or swimming.
-
Attend support groups or counseling to stay motivated.
-
Get regular sleep and stress management through yoga or mindfulness.
C. Emotional and Social Wellbeing
Many patients feel empowered by their transformation-regaining confidence, improving relationships, and leading more active lives. However, body image changes, loose skin, or psychological adjustments may require counseling or reconstructive surgery later.
With consistent self-care and medical follow-up, gastric bypass patients typically enjoy a longer, healthier, and more fulfilling life, free from many obesity-related diseases.
Top 10 Frequently Asked Questions about Gastric Bypass Surgery
1. What is Gastric Bypass Surgery?
Gastric Bypass Surgery (also called Roux-en-Y Gastric
Bypass) is a weight-loss surgery (bariatric surgery) that
helps patients with severe obesity lose weight and improve health.
The surgeon creates a small pouch from the stomach and connects it
directly to the small intestine, bypassing a large portion of the
stomach and upper intestine. This reduces food intake and nutrient absorption, leading
to significant and sustained weight loss.
2. Who is a good candidate for Gastric Bypass Surgery?
You may be eligible for gastric bypass if you:
-
Have a Body Mass Index (BMI) of 40 or higher, or
-
Have a BMI of 35-39.9 with obesity-related health issues like:
-
Type 2 diabetes
-
High blood pressure
-
Sleep apnea
-
Heart disease or joint problems
-
-
Have not achieved weight loss through diet, exercise, or medications
Candidates must also be physically and mentally prepared to adopt lifelong lifestyle changes.
3. How is Gastric Bypass Surgery performed?
The surgery is typically done laparoscopically (minimally invasive), under general anesthesia:
-
The surgeon creates a small stomach pouch (about the size of an egg).
-
The small intestine is divided and attached to the pouch.
-
Food then bypasses most of the stomach and the first part of the intestine.
This limits food intake and reduces calorie absorption, promoting steady weight loss.
The procedure takes around 2-3 hours, and most patients stay in the hospital for 2-3 days.
4. What are the benefits of Gastric Bypass Surgery?
Key benefits include:
-
Rapid and long-term weight loss (60-80% of excess body weight)
-
Improvement or resolution of obesity-related conditions:
-
Type 2 diabetes
-
High blood pressure
-
Sleep apnea
-
High cholesterol
-
-
Enhanced mobility and energy levels
-
Improved self-esteem and quality of life
It's one of the most effective and time-tested bariatric procedures.
5. What are the possible risks or complications?
As with any major surgery, there are potential risks, such as:
-
Infection or bleeding
-
Blood clots
-
Anastomotic leak (leakage where the stomach and intestine are connected)
-
Nutrient deficiencies (iron, calcium, vitamin B12)
-
Dumping syndrome (rapid stomach emptying causing nausea, sweating, or diarrhea)
-
Bowel obstruction or ulcers (rare)
Working with an experienced bariatric team greatly minimizes these risks.
6. What is the recovery process like after Gastric Bypass Surgery?
Recovery time varies by patient:
-
Hospital stay: 2-3 days
-
Return to work: 2-4 weeks (for light work)
-
Full recovery: About 6-8 weeks
Post-surgery, patients follow a liquid diet initially, then progress to soft and solid foods under medical supervision. Regular follow-ups with the bariatric team ensure proper healing and nutrition.
7. How much weight can I expect to lose after Gastric Bypass?
Most patients lose:
-
60-80% of excess body weight within 12-18 months after surgery.
Weight loss is fastest in the first 6 months, then gradually slows.
Long-term success depends on maintaining a healthy diet, regular exercise, and follow-up care.
8. Will I need to take vitamins or supplements after surgery?
Yes. Since gastric bypass reduces nutrient absorption, lifelong supplementation is required to prevent deficiencies. Common supplements include:
-
Multivitamin with minerals
-
Vitamin B12
-
Iron and calcium with Vitamin D
-
Folate (Folic acid)
Your doctor or nutritionist will provide a personalized supplementation plan.
9. Can Gastric Bypass Surgery cure diabetes or other obesity-related diseases?
In many cases, yes - gastric bypass can significantly improve or
even resolve obesity-related conditions.
Studies show:
-
80-90% of Type 2 diabetes patients see remission or improvement.
-
High blood pressure, sleep apnea, and cholesterol levels also improve dramatically.
This makes gastric bypass not just a weight-loss tool but a metabolic surgery that improves overall health.
10. What lifestyle changes are needed after Gastric Bypass Surgery?
Long-term success depends on committed lifestyle changes, including:
-
Eating small, nutrient-rich meals
-
Avoiding high-sugar and fatty foods
-
Regular physical activity
-
Staying hydrated (but avoiding drinks during meals)
-
Attending regular follow-ups with your bariatric team
Following these habits ensures lasting weight loss and better overall health.


