Introduction to Gastric Lap Band Surgery
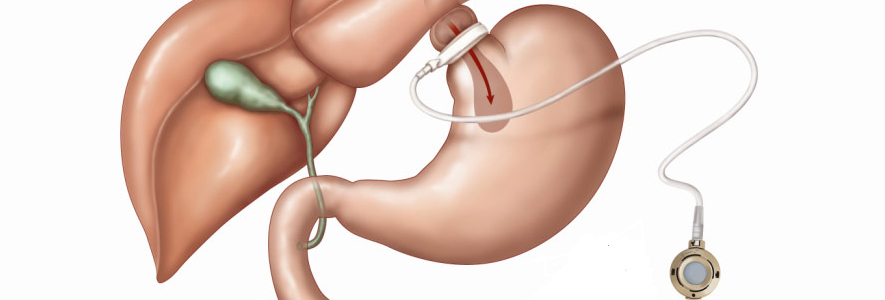
Gastric Lap Band Surgery, medically known as Laparoscopic Adjustable Gastric Banding (LAGB), is a minimally invasive bariatric procedure designed to help individuals achieve significant weight loss by restricting food intake. During this procedure, a surgeon places an adjustable silicone band around the upper portion of the stomach, creating a small pouch that holds only a limited amount of food. The goal is to make patients feel full sooner, eat less, and lose weight gradually and safely over time. Unlike gastric bypass or sleeve gastrectomy, the Lap Band does not require cutting, stapling, or rerouting of the stomach or intestines. This makes it one of the least invasive and fully reversible surgical weight-loss options available.
The Lap Band system also includes an access port placed under the skin of the abdomen, allowing saline adjustments through a small injection. These adjustments tighten or loosen the band, customizing the level of restriction according to the patient's needs and progress. The procedure is typically performed laparoscopically—using small incisions and a camera—leading to minimal scarring, less pain, and faster recovery.
Gastric Lap Band Surgery became popular in the early 2000s for its lower surgical risk profile and reversibility. However, long-term studies show that while effective for many, it requires strict adherence to dietary and lifestyle changes, regular follow-ups, and sometimes additional interventions for best results. Today, it remains a valuable treatment option for patients seeking a restrictive-only bariatric solution who are committed to lifelong follow-up and self-care.
Causes and Risk Factors Leading to Gastric Lap Band Surgery
The main causes and risk factors leading to gastric lap band surgery (LAP-Band) are obesity that has not responded to other weight loss methods and the presence of obesity-related medical conditions. This procedure is chosen for those seeking a less invasive, reversible solution with fewer short-term risks compared to other bariatric surgeries, but who are still in need of effective, long-term weight reduction and improvement of health.
A. Causes / Indications for the Surgery
Gastric Lap Band surgery is performed to treat morbid obesity, a chronic disease where excess body fat negatively affects health, mobility, and lifespan. Candidates typically have:
-
A Body Mass Index (BMI) of 40 or greater, indicating severe obesity.
-
A BMI of 35 or greater with serious health conditions such as type 2 diabetes, hypertension, sleep apnea, or severe joint disease.
-
Repeated failure of non-surgical weight loss programs, including supervised diet, exercise, and pharmacologic therapy.
Obesity often arises from a complex interplay of genetic, metabolic, behavioral, and environmental factors. Genetics may influence appetite regulation and metabolism, while modern sedentary lifestyles and calorie-dense diets contribute to excessive calorie intake. Psychological stress, hormonal imbalances, and poor sleep also play significant roles in weight gain.
For many individuals, obesity becomes resistant to conservative treatment methods, making bariatric surgery the most effective and durable intervention for achieving meaningful, long-term weight reduction. The Lap Band, in particular, is chosen for its safety, adjustability, and reversibility compared to more complex surgeries.
B. Risk Factors and Considerations
Despite being minimally invasive, gastric band surgery carries potential medical and surgical risks that must be carefully evaluated before proceeding.
-
Surgical Risks: Bleeding, infection, or reaction to anesthesia during the operation.
-
Long-Term Risks: Band slippage, erosion, or device malfunction requiring adjustment or removal.
-
Patient-Related Factors: Smoking, poor dietary compliance, or failure to attend follow-up visits can reduce effectiveness and increase complication risk.
-
Pre-existing Conditions: Heart disease, liver disease, or respiratory problems can elevate operative risk.
Proper pre-operative evaluation and patient education help minimize these risks. Patients must understand that the Lap Band is not a quick fix but a lifetime commitment to new eating and lifestyle habits.
Symptoms and Signs Leading to Gastric Lap Band Surgery
Patients who seek gastric band surgery often struggle with persistent and progressive obesity and its associated complications. These symptoms are not of the band itself but of the disease (obesity) that necessitates surgical intervention.
A. Physical Symptoms
-
Chronic Fatigue and Breathlessness: Simple tasks like walking or climbing stairs become exhausting.
-
Joint Pain and Arthritis: Extra body weight stresses the knees, hips, and lower back.
-
Snoring and Sleep Apnea: Interrupted breathing during sleep causes poor rest and daytime drowsiness.
-
Skin Issues: Rashes or infections in skin folds from trapped moisture and friction.
B. Metabolic and Systemic Symptoms
-
Type 2 Diabetes: Persistent high blood sugar despite medication or diet control.
-
Hypertension and Cardiovascular Disease: Elevated blood pressure and cholesterol levels.
-
Gastroesophageal Reflux Disease (GERD): Acid reflux and heartburn caused by abdominal pressure.
-
Infertility or Hormonal Imbalance: Common in women with obesity-related polycystic ovarian syndrome (PCOS).
C. Psychological and Social Signs
-
Depression and Anxiety: Resulting from low self-esteem and body image concerns.
-
Social Withdrawal: Avoidance of activities or events due to embarrassment or mobility limits.
-
Eating Disorders or Emotional Eating: Using food for comfort or stress relief.
Such symptoms significantly reduce quality of life and often prompt patients to consider surgical solutions like the Lap Band, which offers controlled, gradual weight loss and improved health outcomes.
Diagnosis and Preoperative Evaluation for Gastric Lap Band Surgery
Before gastric band surgery, a thorough diagnostic evaluation ensures that the patient is an appropriate candidate. The assessment focuses on medical readiness, psychological stability, and lifestyle commitment.
A. Clinical Assessment
-
BMI Calculation: Confirms obesity classification and eligibility for surgery.
-
Medical History and Physical Exam: Reviews previous weight-loss attempts, family history, and coexisting illnesses such as diabetes or hypertension.
-
Blood Tests: Evaluate blood sugar, lipid profile, thyroid function, liver and kidney health, and nutritional markers (iron, B12, vitamin D, folate).
-
Imaging Studies: Abdominal ultrasound to check for gallstones or liver disease, chest X-ray, and ECG for heart evaluation.
-
Sleep Studies: Conducted if sleep apnea is suspected.
B. Nutritional and Psychological Evaluation
-
A dietitian assesses eating habits and educates patients on post-surgical diet stages (liquid → soft → solid).
-
A psychologist evaluates readiness for long-term behavioral change and screens for depression or eating disorders.
C. Patient Preparation
-
Patients follow a pre-operative low-calorie diet to reduce liver size and surgical difficulty.
-
Smoking cessation and medication adjustments are required weeks before surgery.
A multidisciplinary team approach ensures optimal outcomes, minimizing risk and maximizing long-term success.
Treatment Procedure: The Gastric Lap Band Surgery
Gastric Lap Band Surgery is performed under general anesthesia using laparoscopic (keyhole) techniques, typically lasting 30-60 minutes.
A. Surgical Process
-
Accessing the Abdomen: Small incisions (usually 4-6) are made to insert instruments and a laparoscope (camera).
-
Placement of the Band: The surgeon wraps an adjustable silicone band around the upper stomach to form a small pouch (approximately 30 ml).
-
Attachment of Access Port: A tube connects the band to an access port fixed under the skin. Saline solution can be injected or withdrawn to tighten or loosen the band.
-
Closure and Recovery: Incisions are closed with sutures or surgical glue, and patients are monitored for a few hours.
B. Mechanism of Action
-
The small pouch created by the band limits the amount of food that can be eaten at once.
-
The narrow opening slows the passage of food, promoting early satiety and reduced calorie intake.
-
The band's adjustability allows customized weight loss and gradual adaptation to lifestyle changes.
C. Postoperative Care
Patients are typically discharged within 24-48 hours. A liquid diet is followed for 2 weeks, transitioning to soft and then solid foods. Regular follow-ups are essential to adjust the band for optimal restriction and comfort.
Prevention and Postoperative Management
Effective management after Lap Band surgery is crucial for long-term success and complication prevention.
A. Postoperative Lifestyle Adjustments
-
Dietary Guidelines: Eat small meals, chew thoroughly, avoid high-calorie liquids and carbonated drinks.
-
Exercise Routine: Start with light walking, progressing to 30-60 minutes of moderate activity daily.
-
Hydration: Drink water between meals, not during them.
-
Avoid Smoking and Alcohol: Both can irritate the stomach and hinder healing.
B. Medical Follow-Up
-
Band adjustments are performed at regular intervals to regulate food restriction.
-
Nutritional supplements such as multivitamins, calcium, and B12 may be recommended.
-
Routine blood tests monitor nutritional and metabolic health.
C. Preventing Failure or Complications
Long-term success depends on patient motivation, discipline, and consistent medical supervision. Skipping follow-ups, overeating, or ignoring symptoms like vomiting or reflux can lead to band slippage or poor results.
Complications of Gastric Lap Band Surgery
Although considered one of the safest bariatric procedures, Lap Band surgery is not without potential complications.
A. Early Complications
-
Bleeding and Infection: Typically managed with antibiotics or minor procedures.
-
Postoperative Pain and Swelling: Temporary and resolves within days.
-
Nausea or Vomiting: Common if eating too quickly or in large amounts.
B. Late Complications
-
Band Slippage or Prolapse: The stomach moves above the band, causing obstruction and vomiting.
-
Band Erosion: The band wears through the stomach wall over time, requiring removal.
-
Port Problems: Disconnection or flipping of the port, hindering adjustments.
-
Esophageal Dilation: Caused by chronic overeating or tight restriction.
-
Insufficient Weight Loss or Regain: Often due to poor dietary compliance or lack of band adjustments.
Proper monitoring and prompt medical attention can correct most complications without long-term consequences.
Living with Gastric Lap Band Surgery
Life after gastric banding requires a new relationship with food, body, and lifestyle. Patients who follow their care team's guidance often experience improved health, energy, and self-confidence.
A. Diet and Nutrition
-
Focus on high-protein, low-fat meals in small portions.
-
Avoid sugary, fried, and processed foods.
-
Eat slowly and stop eating when full.
B. Exercise and Physical Health
Consistent physical activity is vital to maintain weight loss, improve cardiovascular health, and prevent muscle loss. Activities like swimming, brisk walking, and yoga are encouraged.
C. Emotional Wellbeing
Weight loss can improve mood, self-esteem, and social confidence, but some patients may struggle with body image or emotional eating. Ongoing psychological support and participation in bariatric support groups can help sustain motivation and prevent relapse.
D. Long-Term Outlook
When followed correctly, Gastric Lap Band Surgery leads to sustained weight loss, improved quality of life, and remission of obesity-related diseases. However, it demands lifelong commitment, self-discipline, and regular follow-up visits to ensure optimal outcomes.
Top 10 Frequently Asked Questions about Gastric Lap Band Surgery
1. What is Gastric Lap Band Surgery?
Gastric Lap Band Surgery, also known as Laparoscopic Adjustable
Gastric Banding (LAGB), is a minimally invasive weight-loss
procedure where a silicone band is placed around the upper
part of the stomach to create a small pouch.
This limits the amount of food you can eat and helps you feel full
sooner, promoting gradual and controlled weight loss. The band's tightness
can be adjusted by adding or removing saline through a small port placed under the skin.
2. Who is a good candidate for Gastric Lap Band Surgery?
You may be a suitable candidate if you:
-
Have a Body Mass Index (BMI) of 40 or more, or
-
Have a BMI between 35 and 39.9 with obesity-related health problems such as:
-
Type 2 diabetes
-
High blood pressure
-
Sleep apnea
-
Heart disease or joint pain
-
-
Have not achieved long-term weight loss with diet, exercise, or medication.
Candidates must also be committed to lifestyle changes and regular medical follow-ups.
3. How does the Gastric Lap Band work?
The adjustable silicone band divides the stomach into two parts:
-
A small upper pouch, which holds a limited amount of food.
-
A larger lower portion, where food passes more slowly.
Because of the smaller pouch, you feel satiated after eating small portions, reducing overall calorie intake. The band can be tightened or loosened through saline injections to adjust the rate of weight loss or manage side effects.
4. How is the Gastric Lap Band procedure performed?
The surgery is done laparoscopically (through small incisions) under
general anesthesia.
Here's how it works:
-
Several small cuts are made in the abdomen.
-
The surgeon places the adjustable silicone band around the upper stomach.
-
The band is connected to a port under the skin for future adjustments.
The procedure usually takes 30-60 minutes, and most patients go home the same day or after one night in the hospital.
5. What are the benefits of Gastric Lap Band Surgery?
The major advantages include:
-
Minimally invasive and reversible procedure
-
No stomach cutting or intestinal rerouting
-
Adjustable according to your needs
-
Shorter recovery time (1-2 weeks)
-
Lower risk of nutritional deficiencies compared to gastric bypass
-
Sustained weight loss when combined with healthy habits
It's a safe and flexible option for long-term obesity management.
6. What are the possible risks or complications?
While Gastric Lap Band Surgery is safe, potential complications can include:
-
Band slippage or erosion
-
Infection or port leakage
-
Difficulty swallowing or nausea
-
Esophageal dilation (rare)
-
Insufficient weight loss if lifestyle changes are not followed
Most issues can be corrected with band adjustments or minor procedures.
7. How much weight can I expect to lose after Gastric Lap Band Surgery?
Weight loss varies by individual but is typically 40-60% of excess body
weight within 12-24 months after surgery.
For example, if you are 100 pounds overweight, you can expect to lose around
40-60 pounds.
Success depends on following your diet, exercise, and regular follow-up
schedule with your bariatric surgeon.
8. What is recovery like after the procedure?
Recovery from gastric band surgery is relatively quick:
-
Hospital stay: Same day or overnight
-
Return to work: Within 1-2 weeks
-
Full recovery: About 4-6 weeks
Post-surgery, you'll follow a liquid diet for the first two weeks, then transition to soft foods, and gradually to solid foods as healing progresses.
Regular follow-ups are important to adjust the band for optimal results.
9. Will I need to make lifestyle or diet changes after surgery?
Yes — success depends largely on long-term lifestyle changes, including:
-
Eating small, frequent meals and chewing food thoroughly
-
Avoiding high-calorie, sugary, or carbonated foods
-
Staying hydrated but avoiding drinking during meals
-
Regular exercise (at least 30 minutes most days)
-
Attending scheduled band adjustment appointments
These changes ensure steady, healthy weight loss and prevent complications.
10. Can the Gastric Lap Band be removed or adjusted later?
Yes. One of the main advantages of the Lap Band is that it is completely adjustable and reversible.
-
The band's tightness can be modified by adding or removing saline via the access port.
-
If necessary, the band can be safely removed without permanent changes to the stomach or intestines.
This flexibility makes it an excellent option for patients seeking a less invasive and adjustable weight-loss procedure.


