Introduction to Glaucoma Implant Surgery
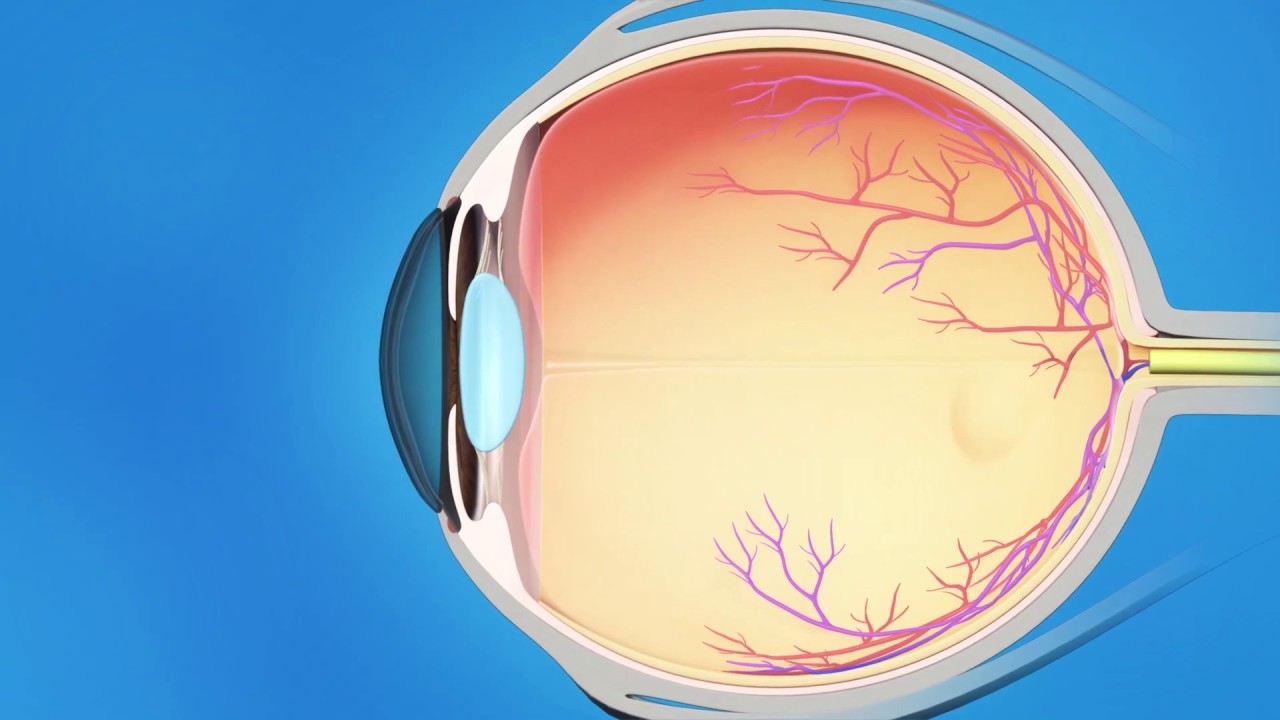
Glaucoma Implant Surgery, also known as aqueous shunt surgery or tube shunt implantation, is a highly advanced ophthalmic procedure performed to control intraocular pressure (IOP) in patients with severe or treatment-resistant glaucoma. Glaucoma is a chronic, progressive eye condition that damages the optic nerve, often due to fluid buildup within the eye. This fluid, known as aqueous humor, normally drains through a natural channel system, but in glaucoma, these pathways become blocked or inefficient, causing increased pressure that can lead to irreversible vision loss if untreated.
During glaucoma implant surgery, the surgeon places a tiny drainage device (implant) into the eye to help drain excess fluid and reduce pressure. The implant typically consists of a small flexible tube connected to a plate that sits on the white part of the eye (sclera). The tube directs fluid away from the anterior chamber to a small reservoir formed under the conjunctiva (the outer membrane covering the eye). The fluid is then absorbed gradually by surrounding tissues, lowering the pressure inside the eye.
This surgery is particularly useful for patients who have failed conventional therapies — such as medications, laser treatments, or earlier filtering surgeries (like trabeculectomy). It is often performed in complex cases, including neovascular, uveitic, congenital, or traumatic glaucoma, where scarring or other issues make traditional drainage procedures less effective.
Glaucoma implant surgery represents a critical advancement in eye care, combining precision, durability, and long-term pressure control to preserve remaining vision and prevent blindness in advanced cases of glaucoma.
Causes and Risk Factors Leading to Glaucoma Implant Surgery
The main reason patients require glaucoma implant surgery is uncontrolled intraocular pressure (IOP) that continues to damage the optic nerve despite all other treatments. Several causes and risk factors can contribute to this scenario:
A. Causes Requiring Surgery
-
Refractory Glaucoma: When medications and laser therapies fail to adequately lower IOP.
-
Scarring from Previous Surgeries: After trabeculectomy or other eye operations, scar tissue can block fluid drainage.
-
Secondary Glaucoma: Caused by eye trauma, inflammation (uveitis), or conditions like neovascular glaucoma (due to diabetic retinopathy).
-
Congenital or Developmental Glaucoma: Present from birth, where natural drainage pathways are malformed.
-
Post-surgical or Post-inflammatory Glaucoma: Increased pressure following cataract or retinal surgery.
B. Risk Factors for Glaucoma Progression
-
Family History of Glaucoma: Strong genetic predisposition.
-
Diabetes and Hypertension: These conditions can damage blood vessels supplying the optic nerve.
-
Severe Myopia (Nearsightedness): Associated with structural changes in the optic nerve.
-
Prolonged Steroid Use: Topical or systemic steroids can increase IOP.
-
Age and Ethnicity: People over 60 and those of African or Asian descent are at higher risk.
When these risk factors combine and pressure remains high despite optimal therapy, glaucoma implant surgery becomes the most reliable way to preserve sight.
Symptoms and Signs Indicating the Need for Glaucoma Implant Surgery
In the early stages, glaucoma is often called the “silent thief of sight” because it develops gradually and painlessly. However, as the disease progresses, symptoms become more apparent and may signal the need for surgical intervention.
A. Common Symptoms
-
Loss of Peripheral Vision: Patients may notice narrowing of their visual field, often described as “tunnel vision.”
-
Blurred or Hazy Vision: Especially in bright light or after prolonged screen use.
-
Eye Pain and Headaches: Particularly in advanced or acute cases with very high pressure.
-
Halos Around Lights: Rings or glares seen around lights at night.
-
Sudden Redness or Nausea: Signs of acute pressure spikes, requiring urgent care.
B. Clinical Signs Observed by Ophthalmologists
-
Elevated Intraocular Pressure (IOP): Measured using tonometry.
-
Optic Nerve Damage: Visible as increased “cupping” on the optic disc during examination.
-
Thinning of Retinal Nerve Fiber Layer: Detected using OCT (Optical Coherence Tomography).
-
Visual Field Loss: Confirmed by perimetry testing.
When these findings persist or worsen despite maximum tolerated therapy, glaucoma implant surgery becomes the best option to protect remaining vision.
Diagnosis and Preoperative Evaluation for Glaucoma Implant Surgery
Before performing implant surgery, ophthalmologists perform a comprehensive evaluation to assess the type, severity, and progression of glaucoma, as well as the overall health of the eye.
A. Diagnostic Tests
-
Tonometry: Measures intraocular pressure accurately.
-
Ophthalmoscopy: Allows direct visualization of the optic nerve head for signs of damage.
-
Gonioscopy: Evaluates the drainage angle of the eye to determine open- or closed-angle glaucoma.
-
Optical Coherence Tomography (OCT): Measures retinal nerve fiber thickness and optic nerve health.
-
Visual Field Test: Maps areas of vision loss and monitors progression.
-
Slit Lamp Examination: Assesses the anterior chamber and lens for abnormalities.
-
Ultrasound Biomicroscopy (UBM): Provides detailed imaging for eyes with prior surgeries or structural anomalies.
B. Preoperative Preparation
-
Systemic Evaluation: Checking for hypertension, diabetes, and clotting disorders.
-
Medication Adjustment: Some glaucoma medications are discontinued before surgery.
-
Patient Counseling: Explaining procedure details, risks, and the fact that surgery prevents further loss but cannot restore lost vision.
This careful diagnostic process ensures the right surgical plan and optimal postoperative outcomes.
Treatment Procedure: The Glaucoma Implant Surgery
The surgery is usually performed under local anesthesia with sedation, though general anesthesia may be used for children or anxious adults. The procedure typically lasts 45-90 minutes and follows these key steps:
A. Surgical Technique
-
Preparation: The surgeon makes a small incision in the conjunctiva (the clear membrane covering the white part of the eye).
-
Implant Placement: A small drainage plate is positioned on the sclera (usually under the upper eyelid) and sutured securely.
-
Tube Insertion: A flexible silicone tube is connected to the plate and inserted into the anterior chamber (front part of the eye) to divert fluid.
-
Fluid Regulation:
-
Valved implants (e.g., Ahmed valve) automatically control fluid flow.
-
Non-valved implants (e.g., Baerveldt) use a temporary ligature to prevent early over-drainage.
-
-
Closure: The tube is covered with donor tissue or scleral patch graft, and the conjunctiva is sutured closed.
B. Postoperative Care
Patients are usually discharged the same day or after an overnight stay. They are prescribed antibiotic and anti-inflammatory drops to prevent infection and control inflammation. Follow-up visits are scheduled frequently to monitor pressure levels and wound healing.
C. Expected Outcomes
-
Reduction in IOP to a safe range (typically 30-50% lower).
-
Stabilization of optic nerve damage and preservation of remaining vision.
-
Reduced dependence on multiple glaucoma medications.
Glaucoma implant surgery has a high success rate in maintaining target pressure, especially in complex or refractory cases.
Prevention and Long-Term Management
While surgery effectively controls pressure, glaucoma remains a lifelong condition that requires ongoing care and vigilance.
A. Post-Surgical Management
-
Regular Check-ups: Frequent visits in the first few months to monitor IOP, implant function, and healing.
-
Medication Adjustment: Some patients may still need eye drops or systemic medications.
-
Lifestyle Modifications: Maintaining a healthy weight, managing diabetes and blood pressure, and avoiding smoking.
-
Protecting the Eye: Avoid rubbing the eyes, heavy lifting, or contact sports during recovery.
B. Preventing Disease Progression
-
Early detection of pressure rise or scarring around the implant capsule through routine imaging and pressure checks.
-
Managing systemic conditions that exacerbate glaucoma (like diabetes and hypertension).
-
Following a nutrient-rich diet high in antioxidants, vitamins A, C, and E to support ocular health.
Proper long-term management is crucial to sustain pressure control and prevent further optic nerve damage.
Complications of Glaucoma Implant Surgery
Although glaucoma implant surgery is generally safe, complications can occur, especially in complex eyes or those with previous surgeries.
A. Early Complications
-
Hypotony: Excessive lowering of eye pressure causing blurred vision or fluid accumulation.
-
Shallow or Flat Anterior Chamber: May require temporary reforming with special injections.
-
Infection (Endophthalmitis): Rare but serious; requires immediate treatment.
-
Bleeding or Inflammation: Controlled with medications.
B. Late Complications
-
Tube Erosion or Exposure: Requires surgical repair to prevent infection.
-
Encapsulation of the Drainage Plate: Leads to increased IOP; may need revision.
-
Corneal Decompensation: Long-term contact of the tube with the cornea can cause cell loss.
-
Persistent Need for Medications: Some patients may still require eye drops.
-
Implant Failure or Migration: In rare cases, the device may need repositioning or replacement.
With modern implants and meticulous technique, complication rates are low, and most issues can be corrected promptly with appropriate care.
Living with Glaucoma After Implant Surgery
After glaucoma implant surgery, patients can expect significant improvements in pressure control and long-term vision stability. However, success depends on strict adherence to follow-up and lifestyle care.
A. Recovery and Daily Life
Most patients resume normal activities within a week, but strenuous activity, swimming, and eye makeup should be avoided for several weeks. It is essential to use all prescribed medications regularly and attend all follow-up visits.
B. Psychological and Lifestyle Adjustments
Living with glaucoma can be emotionally challenging. Patients benefit from counseling and support groups to manage anxiety about vision loss. Incorporating eye-friendly habits—like reducing screen time, managing stress, and protecting the eyes from UV rays—further supports ocular health.
C. Long-Term Outlook
The implant does not cure glaucoma or restore lost vision but effectively slows or halts disease progression. With successful surgery, most patients maintain stable vision for many years, often regaining confidence and independence in daily life.
Top 10 Frequently Asked Questions about Glaucoma Implant Surgery
1. What is Glaucoma Implant Surgery?
Glaucoma Implant Surgery, also known as aqueous shunt or
drainage device surgery, is a procedure performed to reduce
intraocular pressure (IOP) in patients whose glaucoma cannot be controlled
with medications or laser treatments.
During the procedure, a small drainage device (implant or tube) is
placed in the eye to help excess fluid (aqueous humor) drain out, thereby
preventing further optic nerve damage and preserving vision.
2. Why is Glaucoma Implant Surgery needed?
This surgery is recommended when:
-
Eye drops or oral medications fail to control intraocular pressure.
-
Laser treatments (like trabeculoplasty) are ineffective.
-
The patient has advanced or complex glaucoma (such as neovascular or congenital glaucoma).
-
Previous glaucoma surgeries (like trabeculectomy) have not been successful.
The goal is to protect remaining vision by maintaining safe pressure inside the eye.
3. How does a Glaucoma Implant work?
A glaucoma implant acts as a tiny drainage system. It consists of:
-
A small silicone tube placed inside the eye to drain excess fluid.
-
A plate or reservoir placed on the white part of the eye (sclera), where fluid collects and is gradually absorbed by surrounding tissues.
This controlled drainage helps lower eye pressure and prevents further optic nerve damage that leads to vision loss.
4. What types of Glaucoma Implants are available?
Commonly used glaucoma implants include:
-
Ahmed Glaucoma Valve - has a one-way valve to regulate fluid flow.
-
Baerveldt Glaucoma Implant - non-valved device for greater long-term pressure reduction.
-
Molteno Implant - one of the earliest and most reliable designs.
-
Express Shunt or Paul Implant - smaller implants for specific cases.
Your ophthalmologist will choose the best type based on your glaucoma severity, eye structure, and previous surgeries.
5. How is Glaucoma Implant Surgery performed?
The surgery is typically done under local or general anesthesia and
takes about 45-60 minutes.
Steps include:
-
The surgeon makes a small incision in the white part of the eye (sclera).
-
The implant plate is secured to the sclera, and the tube is inserted into the front chamber of the eye.
-
The tube is covered with a thin tissue graft to protect it.
-
The incision is closed with fine sutures.
The procedure is painless, and patients can usually go home the same day.
6. What are the benefits of Glaucoma Implant Surgery?
The main advantages include:
-
Effective long-term control of intraocular pressure
-
Reduced dependence on glaucoma medications
-
Preservation of existing vision
-
Useful for complex or refractory glaucoma cases
-
Safe for patients with previous failed surgeries
This surgery does not restore lost vision but helps prevent further vision loss.
7. What are the possible risks or complications?
Like any eye surgery, potential risks include:
-
Eye redness or discomfort (temporary)
-
Infection or inflammation
-
Tube blockage or excessive drainage
-
Double vision or drooping eyelid (rare)
-
Low eye pressure (hypotony)
-
Corneal damage or erosion (long-term risk)
Most complications can be managed effectively with medication or minor corrective procedures.
8. What is recovery like after Glaucoma Implant Surgery?
Recovery is usually smooth:
-
Mild discomfort or irritation is common for a few days.
-
Vision may be blurry initially but improves gradually.
-
Eye drops will be prescribed to prevent infection and control inflammation.
-
Follow-up visits are required frequently for the first few months.
-
Avoid rubbing the eye, swimming, or strenuous activities during recovery.
Most patients return to normal routines within 2-4 weeks.
9. How successful is Glaucoma Implant Surgery?
Success rates are generally 80-90% in lowering intraocular pressure and
controlling glaucoma.
Many patients experience:
-
Significant pressure reduction
-
Fewer medications needed
-
Stable long-term eye health
However, success depends on individual eye condition, adherence to postoperative care, and regular monitoring.
10. Will I still need glaucoma medication after surgery?
Some patients can completely stop using eye drops, while others may
still need reduced medication to maintain target pressure.
The need for medication varies depending on:
-
The type of implant used
-
Healing response
-
Long-term eye pressure control
Your ophthalmologist will monitor your pressure and adjust treatment accordingly.


