Introduction to Glaucoma (Trabeculectomy)
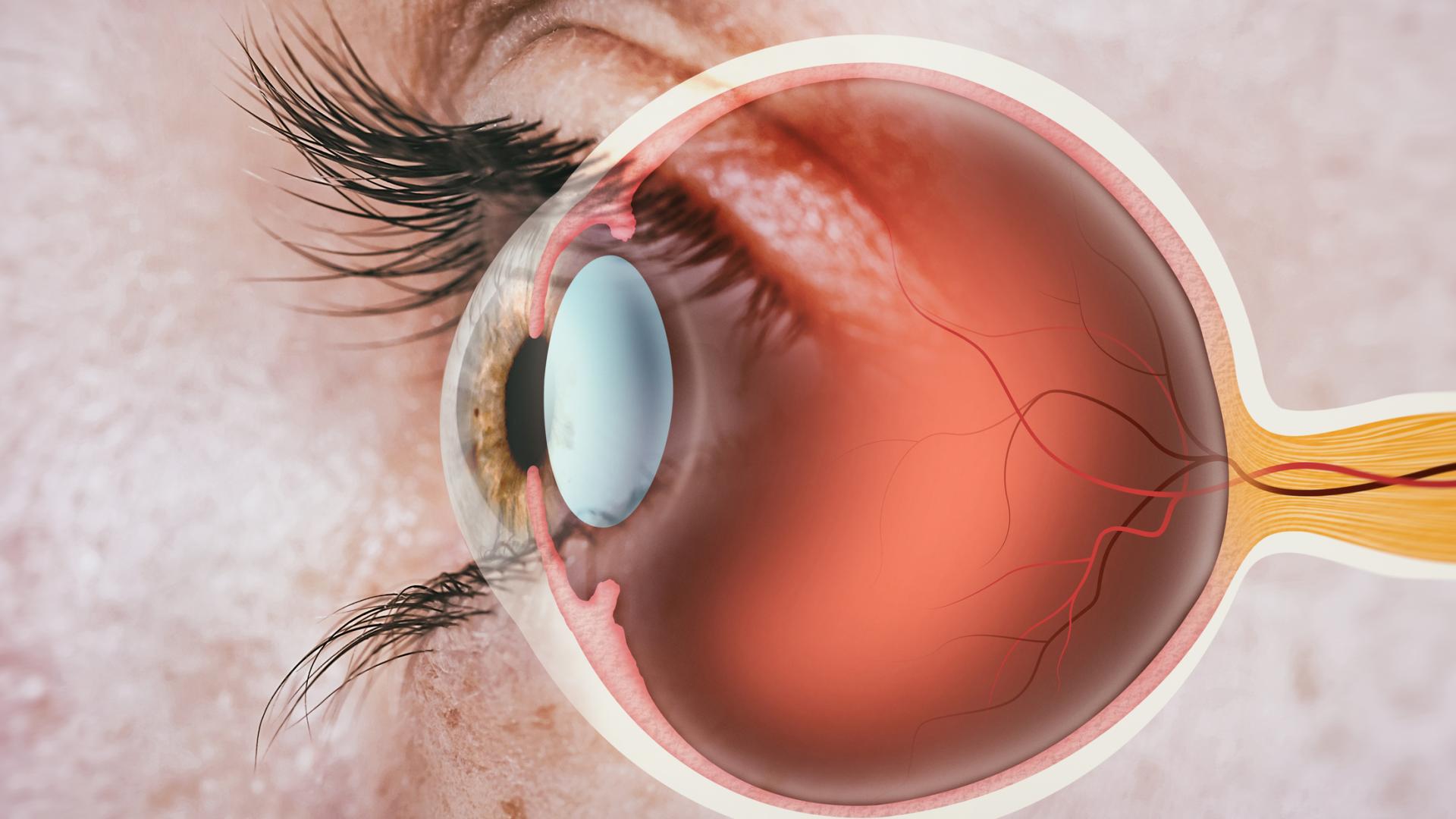
Glaucoma (Trabeculectomy) is a surgical procedure designed to treat advanced or uncontrolled glaucoma by creating a new drainage channel to relieve intraocular pressure (IOP) - the fluid pressure inside the eye. Glaucoma itself is a chronic, progressive eye disease that damages the optic nerve, leading to gradual vision loss and, if untreated, blindness. The primary cause of this damage is the buildup of aqueous humor, the fluid responsible for nourishing eye tissues. Normally, this fluid drains through a delicate structure called the trabecular meshwork, but in glaucoma, this drainage system becomes blocked or inefficient.
Trabeculectomy helps bypass this blockage by forming a controlled fistula (a tiny new drainage pathway) under the conjunctiva, the thin membrane covering the eye. The fluid then collects in a small filtering area called a bleb, located beneath the upper eyelid, where it is slowly absorbed by the body's natural tissues. This procedure effectively lowers eye pressure, preventing further optic nerve damage.
Trabeculectomy is considered the gold standard surgical treatment for glaucoma that doesn't respond adequately to medications or laser therapy. It has been performed successfully for decades and remains one of the most reliable ways to control intraocular pressure in patients with open-angle, closed-angle, or secondary glaucoma. Although it does not reverse vision already lost, it is crucial in halting or slowing the disease's progression, preserving remaining sight, and improving the patient's quality of life.
Causes and Risk Factors Leading to Trabeculectomy
The need for trabeculectomy arises when glaucoma progresses despite other treatment options. Glaucoma itself can result from a wide range of causes - both primary and secondary - that disrupt the balance between fluid production and drainage inside the eye.
A. Primary Causes
-
Primary Open-Angle Glaucoma (POAG): The most common form, in which drainage channels gradually clog without pain or early symptoms, leading to chronic pressure elevation.
-
Angle-Closure Glaucoma: Occurs when the iris bulges and blocks the drainage angle suddenly, causing rapid pressure buildup that can cause severe pain, redness, and vision loss.
-
Normal-Tension Glaucoma: Optic nerve damage occurs even at normal IOP levels, often due to poor blood flow to the nerve.
B. Secondary Causes
-
Neovascular Glaucoma: Caused by new abnormal blood vessels, often secondary to diabetes or retinal vein occlusion.
-
Uveitic Glaucoma: Linked to chronic eye inflammation (uveitis).
-
Traumatic or Post-Surgical Glaucoma: Results from eye injury or complications from other surgeries.
-
Congenital Glaucoma: Present from birth due to abnormal eye development.
C. Risk Factors
Certain risk factors increase the likelihood of developing glaucoma and may lead to surgical intervention:
-
Advanced Age (Above 60 years)
-
Family History of Glaucoma
-
High Myopia (Nearsightedness)
-
Prolonged Steroid Use
-
Ethnicity: African, Hispanic, and Asian populations have higher prevalence.
-
Systemic Conditions: Diabetes, hypertension, or cardiovascular disease can exacerbate the disease.
When these factors coexist and intraocular pressure remains uncontrolled despite maximum medical therapy, trabeculectomy becomes the recommended treatment to preserve remaining vision.
Symptoms and Signs of Glaucoma Requiring Trabeculectomy
Glaucoma is often called the "silent thief of sight" because it progresses slowly and painlessly until significant vision loss occurs. Recognizing symptoms early can make a life-changing difference, but many patients only seek medical attention in the advanced stages when surgery becomes necessary.
A. Symptoms
-
Gradual Peripheral Vision Loss: Difficulty seeing objects to the side or corners of your visual field, often noticed during driving or walking.
-
Blurred or Hazy Vision: Especially under dim lighting conditions.
-
Halos Around Lights: Circular rings or glare seen during nighttime.
-
Eye Pain or Redness: Common in angle-closure glaucoma or during acute pressure spikes.
-
Headache and Nausea: Can occur during severe pressure elevation.
-
Sudden Vision Loss: A medical emergency in acute angle-closure glaucoma.
B. Clinical Signs Observed by Ophthalmologists
-
Elevated Intraocular Pressure (IOP): Persistent despite medications.
-
Optic Nerve Cupping: Progressive deepening and widening of the optic cup on examination.
-
Thinning of Retinal Nerve Fiber Layer: Confirmed by optical coherence tomography (OCT).
-
Progressive Visual Field Loss: Demonstrated by perimetry tests.
If these symptoms and signs worsen despite treatment, trabeculectomy is performed to create a permanent pressure-regulating system, helping preserve the remaining vision.
Diagnosis and Preoperative Evaluation for Trabeculectomy
A thorough diagnostic work-up is crucial before deciding on trabeculectomy. The surgeon must assess the type of glaucoma, its severity, and whether the patient's ocular anatomy can support the procedure.
A. Diagnostic Tests
-
Tonometry: Measures intraocular pressure accurately.
-
Gonioscopy: Examines the drainage angle to classify glaucoma (open-angle or closed-angle).
-
Ophthalmoscopy: Evaluates optic nerve health and degree of cupping.
-
Optical Coherence Tomography (OCT): Measures thickness of the retinal nerve fiber layer.
-
Visual Field Testing: Maps vision loss and tracks progression.
-
Anterior Segment Imaging: Provides a detailed view of the front eye structures.
-
Systemic Evaluation: Includes blood sugar, blood pressure, and general medical clearance.
B. Preoperative Preparation
Before surgery, the ophthalmologist:
-
Adjusts medications (some glaucoma drops are stopped).
-
Treats any eye infections or inflammation.
-
Explains the procedure, outcomes, and recovery expectations.
-
Assesses patient compliance for postoperative visits.
The goal is to ensure the patient is medically and mentally prepared for the surgery and postoperative recovery process.
Treatment Procedure: Trabeculectomy Surgery
Trabeculectomy is typically performed under local anesthesia with sedation, though general anesthesia may be used in certain patients. The surgery lasts around 45 to 90 minutes, and the patient usually goes home the same day.
A. Surgical Steps
-
Creating the Access Flap: The surgeon makes a small incision in the conjunctiva (the transparent outer layer of the eye) to expose the sclera.
-
Forming a Scleral Flap: A partial-thickness flap is made to create a new drainage route.
-
Opening a Drainage Channel: A tiny piece of tissue is removed beneath the flap, connecting the anterior chamber to the subconjunctival space.
-
Regulating Flow: A portion of the iris (iridectomy) is often removed to prevent blockage of the new channel.
-
Closure: The flap and conjunctiva are sutured carefully, allowing fluid to drain slowly and form a filtering bleb under the eyelid.
B. Postoperative Care
After surgery, the patient uses antibiotic and anti-inflammatory eye drops for several weeks. The surgeon monitors the bleb formation and may adjust sutures or apply antifibrotic agents (like mitomycin-C) to prevent scarring, which could close the drainage site.
C. Outcome and Success Rate
Trabeculectomy successfully lowers IOP in 70-90% of patients during the first year. Long-term success depends on ongoing care, healing response, and adherence to follow-up visits.
Prevention and Management After Trabeculectomy
Even after successful surgery, glaucoma management is lifelong. The key goals are to prevent infection, ensure proper healing, and maintain optimal pressure control.
A. Early Postoperative Management
-
Frequent Follow-ups: Weekly visits initially, then monthly for the first 3-6 months.
-
Eye Protection: Wearing an eye shield at night and avoiding rubbing or pressure.
-
Medication Compliance: Using prescribed drops exactly as directed.
-
Activity Restrictions: Avoid heavy lifting, bending, or strenuous exercise for at least 4-6 weeks.
B. Long-Term Management
-
Continued monitoring for pressure fluctuations and bleb health.
-
Managing systemic risk factors like diabetes, blood pressure, and cholesterol.
-
Avoiding dehydration, stress, or excessive caffeine, which can transiently raise eye pressure.
C. Preventing Recurrence or Failure
If scar tissue forms and blocks the drainage pathway, additional procedures (bleb needling or revision) may be required. Early intervention prevents long-term failure and maintains stable pressure.
Complications of Trabeculectomy
Although trabeculectomy is generally safe and effective, it carries certain risks and complications, as with any surgery.
A. Early Complications
-
Hypotony (Low Eye Pressure): Can cause blurred vision or choroidal detachment.
-
Bleeding: Minor bleeding may occur but is usually self-limited.
-
Infection (Endophthalmitis): Rare but serious, requiring urgent care.
-
Shallow or Flat Anterior Chamber: Occurs if fluid drains too rapidly.
B. Late Complications
-
Bleb Failure or Scarring: Leads to re-elevation of IOP.
-
Bleb Leaks: Increases infection risk.
-
Cataract Formation: Common in the years following surgery.
-
Corneal Decompensation: Due to long-term fluid flow changes.
-
Over-Drainage: Causes hypotony maculopathy and visual distortion.
Proper surgical technique, postoperative care, and prompt response to complications significantly improve long-term outcomes.
Living with Glaucoma After Trabeculectomy
Life after trabeculectomy can be extremely positive, especially for those who have struggled with uncontrolled glaucoma for years. The majority of patients experience stabilized vision, reduced dependence on eye drops, and improved confidence in managing their eye health.
A. Recovery and Adjustment
-
Short-Term Recovery: Most patients resume daily activities within 2-3 weeks, with full recovery in 6-8 weeks.
-
Long-Term Vision Stability: The main benefit is preventing further loss, not regaining lost vision.
-
Lifestyle Adaptations: Wearing sunglasses outdoors, eating a nutrient-rich diet, managing stress, and maintaining good hydration.
B. Psychological and Emotional Health
Chronic eye disease can cause anxiety or fear of blindness. Support groups, counselling, and education about the condition can help patients stay optimistic and compliant with their care plan.
C. Ongoing Monitoring
Regular follow-up visits remain essential for life. Even after successful surgery, glaucoma may slowly progress if neglected. Continuous collaboration between the patient and ophthalmologist ensures long-term success and quality of life.
Top 10 Frequently Asked Questions about Glaucoma (Trabeculectomy)
1. What is Glaucoma Trabeculectomy?
Trabeculectomy is a surgical procedure used to treat
glaucoma, a condition that damages the optic nerve due to high
intraocular pressure (IOP).
In this surgery, a small drainage channel is created in the white part
of the eye (sclera) to allow excess fluid (aqueous humor) to drain out,
lowering eye pressure.
The drained fluid forms a tiny reservoir (bleb) under the eyelid where
it is absorbed naturally by surrounding tissues.
2. Why is Trabeculectomy performed?
Trabeculectomy is recommended when:
-
Eye pressure remains uncontrolled despite medications or laser treatments.
-
Progressive optic nerve damage threatens vision.
-
The patient has advanced glaucoma (open-angle or closed-angle).
-
Other surgical or laser options (like glaucoma stents) are not suitable.
The main goal is to preserve remaining vision by preventing further optic nerve damage - not to restore vision already lost.
3. How does Trabeculectomy lower eye pressure?
In a trabeculectomy, the surgeon creates a small opening in the sclera,
forming a new drainage pathway for fluid to exit the eye.
This reduces the buildup of fluid and lowers intraocular pressure (IOP).
The fluid collects under the upper eyelid in a bleb, where it is safely
absorbed into the bloodstream over time.
4. How is Glaucoma Trabeculectomy performed?
The surgery is usually performed under local or general anesthesia and takes about 45-60 minutes:
-
A small incision is made in the upper part of the sclera.
-
A flap is created to regulate fluid drainage.
-
A tiny channel is made for fluid to flow out.
-
The flap and conjunctiva are closed with fine stitches.
Sometimes, antifibrotic medications (like Mitomycin-C) are used during surgery to prevent scarring that might block drainage.
5. What are the benefits of Trabeculectomy?
Key benefits include:
-
Significant reduction in eye pressure (IOP)
-
Long-term control of glaucoma without heavy reliance on medications
-
Preservation of existing vision
-
Effective for advanced or resistant glaucoma cases
For many patients, trabeculectomy can delay or prevent vision loss caused by uncontrolled glaucoma.
6. What are the possible risks or complications?
Although trabeculectomy is generally safe, potential complications include:
-
Infection (endophthalmitis)
-
Bleeding inside the eye
-
Excessive drainage leading to low eye pressure (hypotony)
-
Scarring of the drainage site (causing failure)
-
Blurred vision or discomfort in the early healing stage
-
Cataract formation (over time)
Most side effects are temporary or manageable with proper medical care and close follow-up.
7. What is recovery like after Trabeculectomy?
Recovery usually takes 4-6 weeks:
-
Mild irritation, redness, or blurred vision may occur initially.
-
You'll need to use antibiotic and anti-inflammatory eye drops for several weeks.
-
Avoid rubbing your eye, strenuous activity, or swimming until cleared by your doctor.
-
Regular postoperative check-ups are essential to monitor pressure and healing.
Most patients return to normal activities within 2-4 weeks.
8. How successful is Glaucoma Trabeculectomy?
Trabeculectomy has a success rate of 70-90% in effectively lowering
intraocular pressure and controlling glaucoma progression.
Success depends on:
-
The type and severity of glaucoma
-
The patient's healing response
-
Adherence to postoperative care
Even if some pressure returns over time, the procedure can still reduce the need for medications.
9. Will I still need to use glaucoma eye drops after surgery?
Possibly, but less frequently.
Some patients achieve adequate eye pressure control without medications, while others
may still require reduced dosages or fewer medications.
Your ophthalmologist will assess your intraocular pressure during follow-ups and decide
if drops are still needed.
10. How long do the results of Trabeculectomy last?
In most cases, the results of trabeculectomy can last many years, though
sometimes the drainage site (bleb) can scar over time, reducing effectiveness.
To maintain long-term success:
-
Attend regular eye exams.
-
Use prescribed medications as directed.
-
Protect your eyes from infection and injury.
If scarring occurs, additional treatments (like bleb revision or laser procedures) can help restore drainage.


