Introduction to Grommet Insertion or Removal
Grommet insertion or removal, medically known as tympanostomy tube insertion or extraction, is a common surgical procedure performed to treat conditions involving fluid buildup or poor ventilation in the middle ear. Grommets are tiny, hollow tubes-usually made from silicone, plastic, or metal-that are surgically placed in the eardrum (tympanic membrane). Their purpose is to allow air to circulate between the middle ear and the outer ear, helping equalize pressure and drain trapped fluid. This simple yet effective procedure can dramatically improve hearing and prevent recurrent ear infections, especially in children who frequently suffer from otitis media with effusion (OME) or recurrent middle ear infections.
The grommet itself acts as a small ventilation channel that keeps the middle ear dry and prevents pressure buildup caused by malfunctioning Eustachian tubes-the passages connecting the middle ear to the back of the nose. In children, these tubes are often narrower and more prone to blockage, which leads to fluid accumulation. By providing a bypass route, grommets help restore normal ear function and reduce symptoms like muffled hearing, ear pain, and balance problems.
In most cases, the grommet naturally falls out on its own after several months as the eardrum heals, but sometimes removal is necessary if the grommet remains in place too long, causes persistent discharge, or becomes blocked. The removal procedure is minor and usually performed under local or light general anesthesia. Whether inserted or removed, grommet procedures are among the most frequently performed ear surgeries worldwide, offering significant improvements in hearing, speech development, and quality of life-especially for children affected by chronic ear problems.
Causes and Risk Factors Leading to Grommet Insertion or Removal
The primary reason for grommet insertion is poor drainage or ventilation of the middle ear, most commonly due to Eustachian tube dysfunction. The Eustachian tube's role is to equalize air pressure and allow fluid to drain from the middle ear into the throat. When it fails to function properly-because of inflammation, infection, or anatomical narrowing-fluid builds up behind the eardrum, leading to glue ear, a condition that can cause significant hearing loss and discomfort.
Common causes for grommet insertion include:
-
Recurrent middle ear infections (acute otitis media): Multiple infections within a short period, typically more than three in six months or four in a year.
-
Chronic otitis media with effusion (glue ear): Persistent fluid buildup that affects hearing and speech development.
-
Eustachian tube dysfunction: Often seen in children due to smaller or immature tubes, but can also occur in adults due to allergies, sinus infections, or structural problems.
-
Barotrauma or pressure-related ear pain: Frequent travelers or divers may experience pressure imbalance causing ear pain, where grommets can provide relief.
-
Cleft palate or craniofacial abnormalities: These can interfere with Eustachian tube function, making fluid buildup more likely.
Risk factors necessitating grommet placement or removal include:
-
Chronic sinus or nasal allergy issues.
-
Passive smoking exposure (which increases upper respiratory infections).
-
Family history of recurrent ear problems.
-
Previous ear surgeries or trauma.
-
Environmental factors like cold climates or frequent infections in daycare settings.
Grommet removal becomes necessary if the tube stays in place for more than 18-24 months, gets blocked, causes persistent infection, or leaves a small perforation in the eardrum. Understanding these causes and risks allows timely surgical intervention, ensuring optimal ear health and preventing long-term hearing damage.
Symptoms and Signs of Conditions Requiring Grommet Insertion or Removal
The symptoms leading to grommet surgery typically stem from fluid accumulation or pressure imbalance in the middle ear. The signs vary by age and severity but often include hearing impairment, ear discomfort, or recurrent infections.
Common Symptoms in Children:
-
Frequent ear infections that return soon after antibiotic treatment.
-
Delayed speech development due to hearing difficulties.
-
Poor attention span, difficulty following instructions, or behavioral changes.
-
Tugging or pulling at the ear (a sign of discomfort or pressure).
-
Difficulty balancing or frequent falls in toddlers.
Common Symptoms in Adults:
-
Persistent ear fullness or “blocked” sensation.
-
Muffled hearing or tinnitus (ringing in the ear).
-
Recurrent ear pain or drainage.
-
Discomfort during altitude changes (flying or diving).
Physical Signs Seen by Doctors:
-
Dull or retracted eardrum upon examination.
-
Visible fluid bubbles behind the eardrum.
-
Reduced eardrum movement (detected via tympanometry).
-
Conductive hearing loss revealed through audiometric testing.
In some cases, if the grommet remains too long or becomes clogged, symptoms such as continuous ear discharge, pain, or temporary hearing changes may signal the need for removal. Recognizing these signs early helps prevent complications like permanent hearing loss or chronic middle ear inflammation.
Diagnosis Before Grommet Insertion or Removal
Diagnosis is based on a comprehensive evaluation of middle ear function and hearing capacity. ENT specialists use various diagnostic tools and clinical assessments to determine the necessity of a grommet.
Key Diagnostic Procedures:
-
Otoscopy: A visual examination of the eardrum using a lighted instrument to detect fluid, redness, or perforation.
-
Tympanometry: A simple test that measures eardrum movement and identifies fluid buildup or pressure changes in the middle ear.
-
Audiometry (Hearing Test): Measures the degree of hearing loss and helps distinguish between conductive and sensorineural causes.
-
Nasopharyngeal Assessment: Examines the back of the nose and adenoid tissue, as enlarged adenoids often contribute to poor Eustachian tube function.
-
Medical History and Risk Review: Identifying allergies, sinus problems, and frequency of infections.
For grommet removal, diagnosis involves reviewing the patient's ear health post-insertion. If the tube causes chronic discharge, fails to extrude naturally after 18 months, or leads to persistent perforation, removal is recommended. The ENT specialist ensures the middle ear is dry and well-ventilated before proceeding.
Accurate diagnosis not only ensures the necessity of surgery but also helps determine the appropriate grommet type (short-term or long-term) and optimal surgical approach.
Treatment Options for Grommet Insertion or Removal
Grommet (ventilation tube) insertion and removal are minimally invasive procedures performed primarily to treat persistent middle ear effusion (glue ear), frequent ear infections, and Eustachian tube dysfunction. The main treatment options involve quick day-surgery, and the grommets often fall out on their own, but removal can be performed if needed.
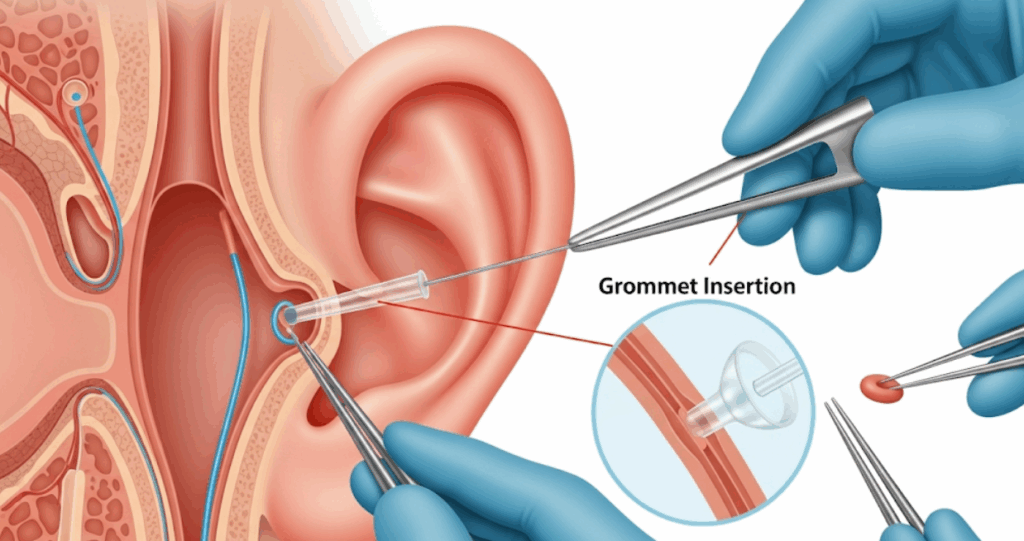
A. Grommet Insertion Procedure
Grommet insertion is a short and safe procedure, usually performed under general anesthesia for children and local anesthesia for adults. The surgeon makes a tiny incision in the eardrum (myringotomy), gently removes any fluid from the middle ear using suction, and places the grommet into the incision. The entire process typically takes 10 to 20 minutes.
There are two main types of grommets:
-
Short-term grommets: Designed to stay in place for 6-12 months, often falling out naturally.
-
Long-term grommets: Shaped differently to stay longer (12-24 months) and used in more chronic conditions.
B. Grommet Removal Procedure
If the grommet doesn't fall out naturally, removal is performed-usually under a microscope in a clinic or minor surgical suite. The surgeon gently extracts the tube, allowing the eardrum to heal. If a small hole remains, it often heals spontaneously, though in rare cases, surgical patching (tympanoplasty) may be required.
C. Postoperative Care
After insertion or removal, patients use antibiotic and anti-inflammatory drops to prevent infection. Hearing usually improves within days, and normal activities can resume quickly. Follow-up visits ensure that the eardrum is healing correctly and pressure is stable.
Prevention and Long-Term Management
Preventing the need for repeated grommet procedures involves addressing the underlying causes of ear dysfunction and maintaining healthy ear hygiene.
Preventive Strategies:
-
Manage Allergies and Sinus Infections: Use prescribed nasal sprays, antihistamines, and avoid allergens.
-
Treat Adenoid Enlargement: Adenoidectomy may be performed alongside grommet insertion in children with chronic Eustachian tube blockage.
-
Avoid Passive Smoking: Tobacco smoke irritates the airways and increases ear infection risk.
-
Boost Immunity: Encourage a balanced diet and proper sleep to strengthen resistance to infections.
Post-Surgical Management:
-
Attend regular check-ups to ensure grommets function properly.
-
Keep the ear dry when bathing or swimming (use earplugs if advised).
-
Report any discharge or discomfort immediately.
-
Ensure follow-up hearing tests to track improvement or detect recurrence.
Consistent care reduces complications and enhances long-term hearing outcomes, especially in children developing language skills.
Complications of Grommet Insertion or Removal
Although generally safe, grommet procedures can occasionally lead to minor complications, most of which are easily manageable.
Potential Complications:
-
Ear Discharge (Otorrhea): The most common issue, usually treated with antibiotic drops.
-
Grommet Blockage: May prevent proper drainage, requiring replacement.
-
Premature Extrusion: The grommet may fall out too soon, leading to recurrence of symptoms.
-
Persistent Eardrum Perforation: Rarely, the eardrum may not close after the tube falls out.
-
Scarring (Tympanosclerosis): Hardening of tissue on the eardrum; typically harmless.
-
Infection Around the Tube: May cause temporary discomfort but resolves with treatment.
In the case of removal, the risks are minimal. Occasionally, patients may experience brief discomfort, mild bleeding, or temporary hearing fluctuation. Close monitoring ensures quick intervention if needed.
Living with Grommet Insertion or Removal
Living with grommets is generally uncomplicated, and most patients notice immediate improvements in hearing, comfort, and quality of life. Children become more attentive, perform better in school, and develop speech more effectively. Parents often report reduced ear infections and fewer antibiotic treatments.
After surgery, patients can return to daily activities within 24-48 hours. Swimming and bathing are safe if approved by the surgeon, although some may recommend using earplugs for additional protection. Regular follow-up visits are crucial to check if the grommets remain functional and if the eardrum is healthy.
After grommet removal, the healing process is typically smooth, and hearing remains stable. If the underlying problem persists-such as allergies or sinus congestion-managing these conditions prevents recurrence. Adopting healthy habits like maintaining good nasal hygiene, avoiding smoking exposure, and controlling infections ensures long-term ear health.
For most patients, grommet insertion or removal is a simple, life-improving procedure that restores ear function, enhances hearing, and prevents chronic ear disease, leading to a healthier, more active, and confident life.
Top 10 Frequently Asked Questions about Grommet Insertion or Removal
1. What is Grommet Insertion?
Grommet insertion (also known as tympanostomy or
ventilation tube insertion) is a minor surgical procedure in which a
tiny tube (grommet) is placed into the eardrum to help
drain trapped fluid and equalize pressure in the
middle ear.
It is commonly performed to treat recurrent ear infections (otitis
media) or persistent fluid buildup that affects hearing,
especially in children.
2. Why is Grommet Insertion needed?
Grommet insertion is recommended when:
-
There are repeated ear infections despite medical treatment.
-
Fluid remains behind the eardrum for more than 3 months (glue ear).
-
The child or adult experiences hearing loss due to middle ear fluid.
-
Speech or learning delays develop from hearing problems.
-
There is chronic Eustachian tube dysfunction (poor ventilation of the middle ear).
The goal is to restore normal hearing, reduce infections, and prevent long-term ear damage.
3. How is Grommet Insertion performed?
The procedure is done under general anesthesia (for children) or
local anesthesia (for adults).
Steps include:
-
The surgeon makes a tiny incision in the eardrum (myringotomy).
-
Any trapped fluid in the middle ear is gently suctioned out.
-
A small grommet (ventilation tube) is placed in the incision to keep it open.
The entire surgery usually takes 10-15 minutes, and most patients can go home the same day.
4. What is Grommet Removal and when is it required?
In most cases, grommets fall out naturally after 6-12
months as the eardrum heals.
However, surgical removal may be required if:
-
The grommet stays in too long (beyond 18 months).
-
It causes discomfort, infection, or persistent discharge.
-
The eardrum does not heal properly after extrusion.
Grommet removal is a simple, quick procedure usually performed under local anesthesia.
5. What are the benefits of Grommet Insertion?
Key benefits include:
-
Improved hearing by draining trapped fluid.
-
Reduced frequency and severity of ear infections.
-
Better speech and learning development in children.
-
Relief from ear pressure, pain, and balance issues.
-
Improved quality of life for children and adults with chronic ear problems.
The procedure is safe, effective, and provides immediate improvement in most cases.
6. What are the possible risks or complications?
Grommet insertion is generally very safe, but some potential (and usually minor) risks include:
-
Ear discharge or infection (usually treatable with drops).
-
Scarring or small hole in the eardrum (rare).
-
Temporary hearing changes.
-
Grommet blockage or premature extrusion.
-
Persistent perforation after the grommet falls out (very rare).
These risks are minimal when the procedure is performed by an experienced ENT specialist.
7. How long do grommets stay in place?
Most grommets stay in place for 6-12 months, though some may fall out
earlier or last longer depending on the type of grommet and the individual's healing
process.
Once the grommet falls out, the eardrum usually heals naturally without
any intervention.
8. What should I expect after Grommet Insertion?
After surgery:
-
Mild discomfort or ear drainage may occur for a few days.
-
Hearing often improves immediately.
-
Avoid getting water in the ears while bathing or swimming (unless cleared by the doctor).
-
Regular follow-up appointments will monitor the grommet's position and ear health.
Children can typically return to school or normal activities within 1-2 days.
9. Will Grommets affect hearing or swimming?
Grommets do not interfere with hearing - in fact, most patients
experience improved hearing.
As for swimming:
-
Surface swimming is usually safe.
-
Avoid diving or deep underwater swimming, as pressure changes can affect the ears.
-
Ear plugs or swimming caps may be recommended to prevent water entry, depending on your doctor's advice.
10. What happens after the Grommet falls out or is removed?
Once the grommet falls out:
-
The eardrum heals naturally, and hearing remains normal in most cases.
-
Some patients may need another grommet insertion if ear fluid builds up again or infections recur.
-
Regular hearing and ENT check-ups are advised to monitor long-term ear health.
Most children eventually outgrow the need for grommets as their Eustachian tube function improves with age.


