Introduction to Heart Transplant
A Heart Transplant is a life-saving surgical procedure in which a diseased or failing heart is replaced with a healthy donor heart. It is typically recommended for patients with end-stage heart failure — a condition where the heart can no longer pump blood efficiently enough to meet the body's needs. The donor heart usually comes from a deceased individual whose family has consented to organ donation.
Heart transplantation represents one of the most advanced achievements in modern medicine. Since the first successful human heart transplant in 1967, surgical techniques, post-operative care, and immunosuppressive therapies have evolved dramatically. Today, the survival rates and quality of life for transplant recipients have improved significantly, with average survival exceeding 10-15 years, and some patients living well beyond two decades.
This surgery is often considered the final treatment option for patients who have not responded to medications, implanted devices, or less invasive surgical interventions. Conditions leading to transplantation include cardiomyopathy, coronary artery disease, congenital heart defects, or severe valvular disorders.
A heart transplant not only prolongs life but also restores normal physical activity, work capacity, and psychological well-being. However, it remains a complex procedure that requires lifelong medical monitoring and commitment from both the patient and healthcare team.
Causes and Risks Leading to Heart Transplant
Heart transplantation becomes necessary when other medical or surgical treatments can no longer support the failing heart. The underlying causes leading to this advanced stage vary depending on age, genetics, and lifestyle factors.
A. Common Causes of End-Stage Heart Failure:
-
Coronary Artery Disease (CAD):
The most common cause. Blocked or narrowed arteries restrict blood flow to the heart, leading to repeated heart attacks and irreversible muscle damage. -
Dilated Cardiomyopathy:
The heart's main pumping chamber (left ventricle) enlarges and weakens, reducing its ability to circulate blood effectively. -
Congenital Heart Disease:
Structural heart defects present from birth may lead to chronic heart failure even after surgical correction. -
Valvular Heart Disease:
Damage or narrowing of heart valves forces the heart to work harder, eventually leading to failure. -
Restrictive or Hypertrophic Cardiomyopathy:
Abnormal thickening or stiffening of heart muscle restricts blood flow and reduces efficiency. -
Viral or Inflammatory Myocarditis:
Viral infections or autoimmune responses can cause inflammation and permanent heart muscle damage. -
Severe Arrhythmias:
Chronic irregular heart rhythms can impair cardiac function over time. -
Toxic Damage:
Long-term alcohol abuse, chemotherapy drugs, or certain medications can damage heart tissue irreversibly.
B. Risk Factors That May Contribute:
-
Long-standing high blood pressure (hypertension).
-
Diabetes mellitus.
-
Obesity and sedentary lifestyle.
-
Smoking and excessive alcohol intake.
-
Family history of heart disease.
-
Previous heart surgeries or implanted devices like LVADs (Left Ventricular Assist Devices).
When the heart's pumping ability is severely compromised and medications or mechanical support are no longer effective, heart transplantation remains the only viable option to restore life and function.
Symptoms and Signs Indicating the Need for Heart Transplant
Patients who may require a heart transplant typically exhibit advanced heart failure symptoms that persist despite maximal medical therapy. These symptoms are progressive and often affect daily living.
Common Symptoms Include:
-
Severe Shortness of Breath:
Especially during exertion or even at rest, due to poor oxygen circulation. -
Chronic Fatigue and Weakness:
Resulting from inadequate blood supply to muscles and organs. -
Swelling (Edema):
Accumulation of fluid in the legs, ankles, or abdomen due to poor cardiac output. -
Rapid or Irregular Heartbeat:
Palpitations or arrhythmias are common as the heart struggles to compensate. -
Persistent Cough:
Often caused by fluid buildup in the lungs (congestive heart failure). -
Weight Gain from Fluid Retention:
Sudden increase in body weight due to excess fluid accumulation. -
Reduced Exercise Tolerance:
Patients may find it difficult to climb stairs, walk short distances, or perform basic tasks. -
Chest Pain or Pressure:
Particularly in patients with coronary artery disease. -
Dizziness or Fainting (Syncope):
Caused by reduced blood flow to the brain.
When symptoms persist despite medications, device therapy (like pacemakers or LVADs), and lifestyle changes, patients are evaluated for heart transplant eligibility.
Diagnosis and Evaluation Before Heart Transplant
Heart transplant candidacy requires thorough medical evaluation to ensure that the patient will benefit from the procedure and can tolerate lifelong immunosuppression.
A. Diagnostic and Preoperative Assessment:
-
Echocardiography (Echo):
Evaluates heart size, ejection fraction, valve function, and wall motion abnormalities. -
Electrocardiogram (ECG):
Detects arrhythmias and prior heart attack evidence. -
Cardiac Catheterization:
Measures pressures in heart chambers and assesses coronary artery blockages. -
Chest X-Ray and MRI:
Helps evaluate heart enlargement and lung conditions. -
Cardiopulmonary Exercise Testing (VO2 Max):
Determines how well the heart and lungs deliver oxygen — a key factor for transplant eligibility. -
Blood Tests:
To assess liver and kidney function, infection status, and tissue compatibility. -
Right Heart Catheterization:
Measures blood pressure and oxygen levels in the lungs to evaluate pulmonary hypertension. -
Psychological and Social Evaluation:
Determines mental readiness and availability of family or caregiver support post-transplant.
B. Eligibility Criteria:
A patient may be listed for a heart transplant if they:
-
Have end-stage heart failure with life expectancy <1 year.
-
Have no other serious medical conditions (e.g., cancer, severe infections).
-
Are non-smokers and free from substance abuse.
-
Can adhere to complex medical regimens post-surgery.
Once approved, patients are placed on an organ waiting list based on medical urgency, blood type, body size, and geographic location.
Treatment Options: The Heart Transplant Procedure
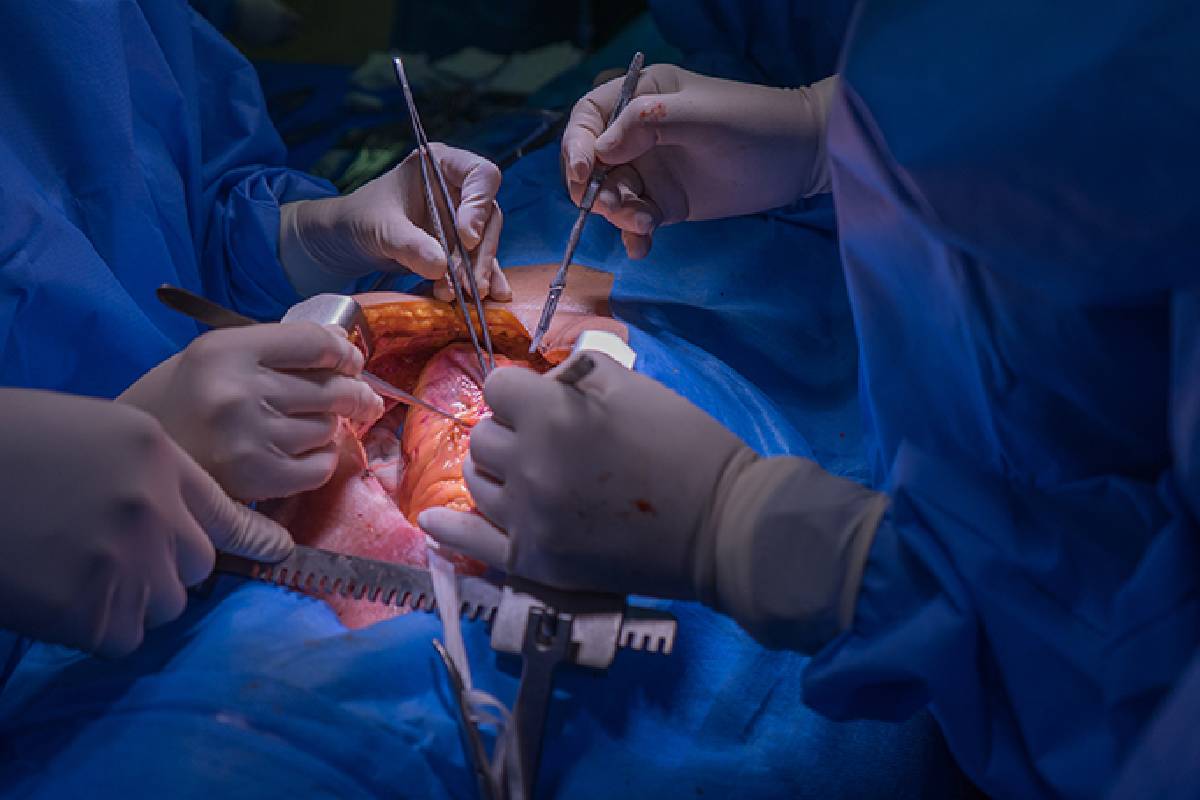
The heart transplant procedure is a complex, life-saving operation for end-stage heart failure, performed in carefully selected patients when other treatments have failed. It involves replacing the recipient's diseased heart with a healthy donor heart, using advanced surgical and anesthesia techniques.
A. Overview of the Procedure:
A heart transplant surgery involves the removal of the patient's failing heart and replacing it with a healthy donor heart. The surgery typically lasts 4 to 6 hours and is performed under general anesthesia by a specialized cardiothoracic surgical team.
B. Step-by-Step Process:
-
Preparation:
The patient is placed on a cardiopulmonary bypass machine that temporarily takes over heart and lung function. -
Removal of Diseased Heart:
The surgeon removes the majority of the failing heart, leaving part of the back walls of the atria intact. -
Donor Heart Implantation:
The donor heart is sewn into place, connecting the major blood vessels (aorta, pulmonary artery, and vena cava). -
Reperfusion:
Once connected, blood flow is restored, and the new heart begins beating — sometimes with mild electrical stimulation. -
Closure and Recovery:
The chest is closed, and the patient is transferred to the intensive care unit (ICU) for close monitoring.
C. Postoperative Recovery:
-
The patient remains in the ICU for 1-2 weeks under continuous cardiac monitoring.
-
Immunosuppressive medications are started immediately to prevent organ rejection.
-
Most patients can resume normal activities within 3-6 months with proper rehabilitation.
D. Alternatives to Heart Transplant:
For patients not suitable for transplantation, alternative therapies include:
-
Left Ventricular Assist Devices (LVADs): Mechanical pumps that assist heart function.
-
Total Artificial Heart (TAH): Fully mechanical heart replacement for selected patients.
-
Stem Cell Therapy and Regenerative Medicine: Experimental approaches showing promise for future treatment.
Prevention and Management After Heart Transplant
Post-transplant management is critical for long-term success and includes a combination of medication, lifestyle changes, and regular medical follow-up.
A. Medical Management:
-
Immunosuppressive Therapy:
Medications such as cyclosporine, tacrolimus, and prednisone are used to prevent immune rejection.
These drugs must be taken lifelong, and dosage is carefully adjusted to balance protection and side effects. -
Infection Prevention:
Due to immune suppression, patients are at increased risk for infections. Maintaining hygiene, avoiding crowded areas, and adhering to vaccination schedules are essential. -
Cardiac Rehabilitation:
A supervised exercise program helps rebuild strength, improve circulation, and promote cardiovascular health. -
Regular Monitoring:
Frequent endomyocardial biopsies, echocardiograms, and lab tests detect early rejection or complications.
B. Lifestyle and Preventive Measures:
-
Eat a heart-healthy diet (low in salt, fat, and cholesterol).
-
Maintain an optimal body weight.
-
Avoid smoking, alcohol, and illicit drugs.
-
Manage stress and prioritize adequate sleep.
-
Stay physically active with moderate daily exercise.
With adherence to medical recommendations, most transplant recipients lead full, active lives with high functional capacity.
Complications of Heart Transplant
While outcomes have greatly improved, certain complications can occur either immediately or years after transplantation.
A. Early Complications:
-
Acute Organ Rejection:
The body's immune system attacks the donor heart — often within the first six months. Detected through biopsies and managed with immunosuppressants. -
Infection:
Due to immunosuppression, even minor infections can become serious. -
Bleeding and Blood Clots:
Related to surgery or anticoagulant therapy. -
Kidney Damage:
Caused by long-term use of immunosuppressive drugs.
B. Long-Term Complications:
-
Chronic Rejection (Cardiac Allograft Vasculopathy):
Gradual thickening of coronary arteries in the transplanted heart leading to poor circulation. -
Hypertension and High Cholesterol:
Common side effects of long-term medication use. -
Cancer:
Increased risk, particularly of skin cancers and lymphomas, due to immune suppression. -
Osteoporosis:
Bone weakening caused by steroid therapy.
Despite these risks, ongoing medical advancements have significantly reduced complication rates, allowing most recipients to enjoy a decade or more of healthy life post-surgery.
Living with the Condition After Heart Transplant
Life after a heart transplant requires commitment, discipline, and close medical follow-up. Patients often experience profound improvement in energy levels, endurance, and emotional well-being.
A. Post-Transplant Lifestyle:
-
Regular Exercise: Walking, cycling, or swimming strengthens the heart.
-
Healthy Diet: Emphasize fruits, vegetables, lean protein, and whole grains.
-
Mental Health Support: Counseling or support groups help patients adapt emotionally.
-
Routine Follow-ups: Essential to detect complications early and adjust medications.
B. Emotional and Social Recovery:
Patients may experience emotional highs and lows after surgery. Counseling, family support, and mindfulness-based therapies can help reduce anxiety and promote long-term stability.
C. Prognosis and Quality of Life:
Modern advances in surgery and immunotherapy have improved survival dramatically:
-
1-Year Survival Rate: Over 90%.
-
5-Year Survival Rate: 75-80%.
-
10-Year Survival Rate: Around 65%.
Most recipients return to normal daily life — including work, travel, and recreation — enjoying an active and fulfilling lifestyle for many years after transplantation.
Top 10 Frequently Asked Questions about Heart Transplant
1. What is a Heart Transplant?
A Heart Transplant is a life-saving surgical procedure
in which a diseased or failing heart is replaced with a healthy
donor heart from a person who has recently died.
It's usually recommended for patients with end-stage heart failure when
medications, lifestyle changes, or other surgeries no longer work. The goal is to
restore normal heart function, improve quality of life, and extend
survival.
2. Who needs a Heart Transplant?
A heart transplant may be recommended for patients who have severe, irreversible heart disease, such as:
-
End-stage heart failure (when the heart cannot pump enough blood)
-
Coronary artery disease with damaged heart muscle
-
Cardiomyopathy (dilated or restrictive)
-
Congenital heart defects unresponsive to surgery
-
Severe valvular heart disease
-
Life-threatening arrhythmias (abnormal heart rhythms)
Candidates are those for whom all other treatments have failed but who are otherwise healthy enough to undergo major surgery.
3. How is a Heart Transplant performed?
The surgery is done under general anesthesia and typically takes
4-6 hours.
Steps include:
-
The diseased heart is removed, leaving the back wall of the left atrium in place.
-
The donor heart is then sewn into position and connected to major blood vessels.
-
The surgeon restarts the new heart, often with an electric shock.
-
The patient is placed on a heart-lung bypass machine during the procedure to maintain oxygen and blood flow.
After surgery, patients stay in the intensive care unit (ICU) for close monitoring.
4. How long does it take to recover from a Heart Transplant?
Recovery typically occurs in stages:
-
Hospital stay: About 2-3 weeks after surgery.
-
Initial recovery: 2-3 months, focusing on wound healing and medication adjustment.
-
Full recovery: Usually 6 months to 1 year, depending on individual progress.
Patients participate in cardiac rehabilitation to regain strength and are monitored regularly for signs of organ rejection or infection.
5. What are the risks or complications of Heart Transplant surgery?
Like any major surgery, a heart transplant carries some risks, including:
-
Organ rejection (the immune system attacking the donor heart)
-
Infection due to immune-suppressing drugs
-
Bleeding or blood clots
-
Coronary artery vasculopathy (thickening of heart arteries)
-
Kidney damage from long-term medications
-
Cancer risk (rare, due to immunosuppressants)
Regular follow-ups, medications, and healthy lifestyle choices greatly reduce these risks.
6. What is organ rejection and how is it managed?
Organ rejection occurs when the immune system identifies the new heart
as foreign and tries to attack it.
To prevent this:
-
Patients must take immunosuppressive (anti-rejection) medications for life.
-
Regular biopsies and blood tests are performed to detect rejection early.
Symptoms of rejection may include fatigue, shortness of breath, swelling, or fever.
Most rejection episodes are treatable if caught early.
7. What medications are needed after a Heart Transplant?
After a heart transplant, patients must take immunosuppressive drugs to prevent rejection. Common medications include:
-
Tacrolimus (Prograf) or Cyclosporine
-
Mycophenolate mofetil (CellCept)
-
Prednisone (steroid)
Additionally, other drugs may be prescribed to: -
Control blood pressure and cholesterol
-
Prevent infection and blood clots
-
Manage side effects of anti-rejection medications
Medication adherence is crucial for long-term success.
8. How successful is a Heart Transplant?
Heart transplants have excellent success rates with modern techniques and medications:
-
1-year survival rate: Around 85-90%
-
5-year survival rate: About 75%
-
Average life expectancy post-transplant: 10-15 years, with many patients living longer.
Success depends on age, overall health, and lifestyle choices after surgery.
9. What lifestyle changes are needed after a Heart Transplant?
A heart transplant requires lifelong commitment to healthy living, including:
-
Taking medications exactly as prescribed.
-
Regular exercise and participation in cardiac rehabilitation.
-
Healthy diet low in salt, fat, and cholesterol.
-
Avoiding smoking, alcohol, and recreational drugs.
-
Regular follow-up visits with your cardiologist.
Maintaining these habits helps ensure long-term heart health and overall well-being.
10. What is life like after a Heart Transplant?
Most patients enjoy a dramatically improved quality of life after recovery. They experience:
-
More energy and mobility
-
Better breathing and stamina
-
Ability to return to work or hobbies
-
A renewed sense of independence and well-being
While lifelong monitoring and medication are necessary, most transplant recipients lead active, fulfilling lives for many years.


