Introduction to Heart Valve Repair
The human heart is equipped with four essential valves - the mitral, aortic, tricuspid and pulmonary valves - each acting like a one-way gate to ensure blood flows in the correct direction at each heartbeat. When one or more of these valves become damaged, narrowed (stenosis), leaky (regurgitation) or dysfunctional, the heart's ability to pump efficiently is compromised. This condition is collectively known as heart valve disease. While in many cases the damaged valve is replaced, modern cardiac surgery increasingly prefers heart valve repair whenever feasible - that is, adjusting, reconstructing or reshaping the existing valve rather than replacing it entirely.
Heart valve repair surgery aims to preserve as much of the patient's native valve tissue as possible, maintain better heart function, reduce complications associated with artificial valves, and improve long-term outcomes. Such repair techniques may involve trimming valve leaflets, reinforcing the valve annulus (ring), repairing supporting cords or reinserting native tissue. Advancements in minimally invasive and transcatheter approaches now allow many patients to undergo repair with smaller incisions, less trauma and quicker recovery times. When successful, valve repair not only relieves symptoms like shortness of breath, fatigue and chest pain, but also helps prevent progression to heart failure, extends life expectancy and enhances quality of life.
Given the complex interplay between valve structure, heart chambers, blood flow and patient health status, valve repair is a highly individualized procedure - it requires a multidisciplinary heart team (cardiac surgeon, cardiologist, imaging specialist) and sophisticated imaging and surgical planning. For patients whose anatomy allows it, repair is often the preferred option over replacement. Understanding the causes, risks, symptoms, diagnostic process, treatment pathways, prevention/management, complications and life-after surgery is critical for both patients and clinicians alike.
Causes and Risk Factors of Valve Disease Leading to Repair
The most common causes and risk factors of heart valve disease that lead to valve repair include congenital defects, age-related degeneration, infections, and other cardiovascular conditions. These issues can result in stenosis (narrowing), regurgitation (leakage), or prolapse of the heart valves, requiring surgical or catheter-based intervention.
A. Causes of Valve Disease
Valve disease emerges from a variety of causes. Some of the most common include:
-
Degenerative changes with aging: As patients grow older, valve leaflets may become thickened, calcified and less flexible, leading to stenosis (narrowing) or regurgitation (leakage).
-
Rheumatic fever (though less common in developed countries): Prior infection can leave scarred, fused valve tissue.
-
Congenital heart defects: Some individuals are born with malformed valves (for example bicuspid aortic valve) that predispose them to early dysfunction.
-
Infective endocarditis: An infection of the valve can destroy leaflets or supporting structures, resulting in acute dysfunction.
-
Ischemic heart disease or myocardial infarction: Damage to heart muscle can deform valve apparatus (especially the mitral valve) causing regurgitation.
-
Connective tissue disorders or other comorbidities: For instance Marfan syndrome, lupus or other conditions may affect valve integrity or support structures.
-
Radiation therapy, trauma or prior cardiac surgery: These may adversely affect valve tissue or nearby structures, making repair more challenging.
B. Risk Factors That Affect Progression
Individuals with one or more of the following factors are at higher risk of developing significant valve disease requiring repair:
-
Advanced age (50+ to 70+).
-
Hypertension, diabetes and other cardiovascular risk factors.
-
Family history of valve disease.
-
Prior history of rheumatic disease or endocarditis.
-
High cholesterol or calcium burden (affecting valve leaflets).
-
Obesity, sedentary lifestyle and smoking (contribute to overall cardiac stress).
-
Existing heart conditions (e.g., left ventricular dysfunction, arrhythmias) that increase strain on the valves.
C. Risks Specific to Repair Eligibility
Not all valve-disease patients are candidates for repair. Some eyes into risk include:
-
Severe calcification or destruction of valve tissue may preclude repair in favour of replacement.
-
Poor ventricular function or other comorbidities (kidney, lung, liver disease) raise surgical risk.
-
Repeated prior surgeries or severe scarring may complicate a repair approach.
-
Anatomical complexities (multiple valve involvement, combined valve disease) may reduce success of repair technique.
Understanding these underlying causes and risk factors helps in the timely identification of patients who may benefit from repair rather than simply "waiting until replacement is necessary."
Symptoms and Signs Indicating Need for Heart Valve Repair
Valve disease often progresses gradually - and in many cases symptoms are subtle until more advanced disease sets in. Recognising the early signs helps enable timely intervention, which improves outcomes.
Common Symptoms
Depending on whether the valve problem causes obstruction (stenosis) or regurgitation, symptoms vary:
-
Shortness of breath, especially on exertion (e.g., climbing stairs) or when lying flat (orthopnea).
-
Fatigue and weakness: The heart must work harder, so patients tire more easily.
-
Palpitations or irregular heartbeat: Valve disease can provoke arrhythmias.
-
Chest pain or discomfort: Especially if the heart is under stress.
-
Swelling in feet, ankles or abdomen (edema) due to backward pressure in the circulation.
-
Reduced ability to exercise, dizziness or fainting spells: More common in severe stenosis.
-
Fluid retention or rapid weight gain: Suggests worsening heart performance.
Clinical Signs on Physical Examination
-
Murmur heard on auscultation: Depending on valve affected, characteristic murmurs (whooshing, blowing or harsh sounds) may be detected.
-
Changes in heart sounds: An S3 or S4 heart sound, valve click or opening snap may be present.
-
Signs of heart failure: Elevated jugular venous pressure (JVP), crackles in the lungs, hepatomegaly.
-
Evidence of reduced perfusion: Cool extremities, weak pulses.
-
Associated findings: For example: if mitral regurgitation leads to left atrial enlargement, one may detect atrial fibrillation on ECG.
When these symptoms and signs appear - especially in the context of known valve disease - cardiologists and surgeons will often evaluate the patient for potential valve repair rather than waiting for full-blown failure.
Diagnosis of Heart Valve Disease and Repair Eligibility
Diagnosis of heart valve disease is a stepwise process that combines history, physical examination, and a selection of specialized tests. Eligibility for heart valve repair depends on the valve involved, severity, symptoms, heart function, comorbidities, and risk assessment.
Diagnostic Components
-
Echocardiography (Transthoracic and/or Transesophageal): The primary and most informative test. It assesses valve morphology (leaflets, annulus, cords), function (degree of regurgitation or stenosis), chamber sizes, pressures, and heart function.
-
Cardiac MRI or CT scan: Useful in complex anatomy (e.g., congenital valves, multiple valve disease, evaluation of associated structures).
-
Cardiac catheterisation (in selected cases): Helps assess coronary arteries or confirm haemodynamic severity pre-surgery.
-
Electrocardiogram (ECG) and chest X-ray: Basic tests to detect arrhythmias, chamber enlargement, pulmonary congestion.
-
Exercise stress testing or cardiopulmonary testing: May be used to evaluate functional capacity, symptom correlation and surgical risk.
-
Preoperative assessment: Blood tests (kidney, liver, coagulation), lung function tests, and evaluation of comorbidities. Surgical risk is discussed with the heart team.
Assessment of Repair Suitability
The determination between repair versus replacement depends on multiple factors:
-
Valve type (mitral valves are often more repairable than aortic).
-
Extent of tissue damage or calcification.
-
Ventricular function and overall heart performance.
-
Patient age, comorbidities, expected lifespan and patient preference.
-
Surgical center and surgeon experience (repair success is better in high-volume specialized centres).
-
Presence of other cardiac interventions needed (e.g., bypass surgery) influences timing and approach.
By integrating these diagnostic findings and risk assessments, the heart team decides whether valve repair is feasible, advisable and expected to offer better outcomes than replacement.
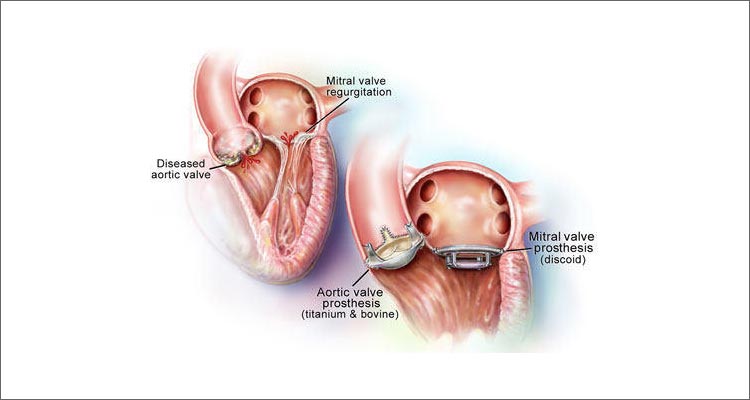
Treatment Options: Heart Valve Repair and Surgical Procedure
Treatment options for heart valve disease focus on either repairing or replacing the diseased valve, using open-heart surgery, minimally invasive/robotic approaches, or catheter-based interventions depending on the valve, anatomy, severity, and patient risk.
A. Non-Surgical and Less-Invasive Options
Before or alongside surgical repair, certain treatments may be considered:
-
Medical therapy to control heart failure symptoms (diuretics, ACE inhibitors, beta-blockers).
-
Percutaneous or transcatheter procedures (e.g., balloon valvuloplasty for stenotic valves, transcatheter edge-to-edge repair for mitral or tricuspid regurgitation).
-
Close monitoring with regular imaging if valve disease is mild and stable.
However, when symptoms are moderate to severe, ventricular dysfunction is present or the valve disease is progressing despite conservative management, surgical repair becomes necessary.
B. Surgical Repair - Techniques and Procedure
Heart valve repair surgery involves a variety of approaches depending on which valve is involved (mitral, aortic, tricuspid, pulmonary), and whether the approach is open-heart or minimally invasive.
Typical Steps of Valve Repair
-
Anesthesia and Surgical Access: Traditionally via a
median sternotomy (chest bone split) or via minimally invasive incisions
(mini-thoracotomy, keyhole).
-
Cardiopulmonary Bypass: The heart may be temporarily
stopped and a bypass machine sustains circulation.
-
Valve Inspection: The surgeon assesses the valve
leaflets, cords, annulus, and adjacent structures.
-
Repair Techniques:
-
Patch repair of leaflets (to close holes or defects).
-
Shortening or replacing broken chordae (cords that support
leaflets).
-
Annuloplasty (placing a ring or band around the valve annulus) to
reshape and reinforce.
-
Removal of excess tissue or calcium, reshaping of leaflets, or
separation of fused leaflets.
-
Special techniques tailored for each valve (e.g., mitral valve
edge-to-edge repair, aortic root repair).
-
Testing and Closure: The repaired valve is tested by
filling the heart with fluid to check for leakage or stenosis, then
surgical closure is performed.
-
Recovery Support: The patient is weaned from bypass,
heart restarted, chest closed, and recovery begins.
Emerging Techniques
-
Minimally invasive repair via smaller incisions reduces
trauma, decreases blood loss and shortens recovery.
-
Transcatheter repair devices (e.g., MitraClip, TriClip)
for high-risk patients who may not tolerate open surgery.
-
Hybrid approaches combining surgical and catheter
techniques.
C. Choosing Repair Over Replacement
Anesthesia and Surgical Access: Traditionally via a median sternotomy (chest bone split) or via minimally invasive incisions (mini-thoracotomy, keyhole).
Cardiopulmonary Bypass: The heart may be temporarily stopped and a bypass machine sustains circulation.
Valve Inspection: The surgeon assesses the valve leaflets, cords, annulus, and adjacent structures.
Repair Techniques:
-
Patch repair of leaflets (to close holes or defects).
-
Shortening or replacing broken chordae (cords that support leaflets).
-
Annuloplasty (placing a ring or band around the valve annulus) to reshape and reinforce.
-
Removal of excess tissue or calcium, reshaping of leaflets, or separation of fused leaflets.
-
Special techniques tailored for each valve (e.g., mitral valve edge-to-edge repair, aortic root repair).
Testing and Closure: The repaired valve is tested by filling the heart with fluid to check for leakage or stenosis, then surgical closure is performed.
Recovery Support: The patient is weaned from bypass, heart restarted, chest closed, and recovery begins.
Minimally invasive repair via smaller incisions reduces trauma, decreases blood loss and shortens recovery.
Transcatheter repair devices (e.g., MitraClip, TriClip) for high-risk patients who may not tolerate open surgery.
Hybrid approaches combining surgical and catheter techniques.
When feasible, repair offers several advantages:
-
Preservation of native valve geometry and function.
-
Better long-term survival and fewer complications (e.g., no lifelong blood thinners required in many cases).
-
Lower risk of prosthetic valve failure or thrombosis.
-
Often better quality of life post-surgery.
However, repair is not always possible - the surgical team will determine based on individual anatomy, disease severity and comorbidities.
Prevention and Management After Valve Repair
Prevention and management after heart valve repair focus on structured recovery, ongoing medication, lifestyle adjustments, infection prevention, and careful follow-up to ensure valve health and minimize long-term complications.
A. Prevention of Valve Disease Progression
Though some causes are non-modifiable (genetics, congenital defects), the progression of valve disease can often be slowed through:
-
Maintaining healthy blood pressure, cholesterol and blood sugar.
-
Avoiding smoking, maintaining healthy weight and exercising.
-
Managing infections and dental hygiene to reduce risk of endocarditis (infection of the valve).
-
Regular cardiology check-ups - early detection of valve disease allows timely intervention before advanced damage occurs.
-
Treating associated cardiac conditions (e.g., coronary artery disease, atrial fibrillation) which can strain valves.
B. Post-Repair Management
After successful valve repair surgery the following steps are vital:
-
Hospital Recovery: Initially monitored in intensive care unit, gradually moved to standard ward; early mobilization begins.
-
Medications: Post-operative medications may include anticoagulants (depending on repair type), antibiotics (to prevent infection), and standard heart medications (ACE inhibitors, beta-blockers).
-
Lifestyle & Rehabilitation: Cardiac rehabilitation programs guide safe return to exercise, optimise cardiovascular conditioning and educate patients on heart-healthy lifestyle.
-
Follow-Up Imaging: Echocardiograms at defined intervals to verify valve function, chamber size, and detect early signs of recurrent disease.
-
Monitoring for Complications: Signs such as new murmurs, arrhythmias, increasing fatigue or fluid retention warrant prompt evaluation.
-
Long-Term Care: Lifelong surveillance is important - even after a successful repair, valve disease may recur, and comorbid conditions may evolve.
Complications of Heart Valve Repair
While valve repair is highly beneficial and often preferable to replacement, it does carry inherent risks - as does any cardiac surgery. Awareness of possible complications helps patients anticipate and engage in preventive care.
Common Risks Include:
-
Bleeding or haematoma at surgical site.
-
Infection, including endocarditis of the repaired valve.
-
Arrhythmias, such as atrial fibrillation, which may require temporary or permanent treatment.
-
Residual leakage or stenosis of the repaired valve if repair is not ideal.
-
Thromboembolism (clot formation) especially if repair involves prosthetic material or if atrial fibrillation is present.
-
Heart failure or reduced cardiac function if ventricular damage is significant.
-
Need for re-operation: Repair may fail over time requiring either repeat repair or replacement.
-
Minimally invasive/ transcatheter risks: Device malfunction, vascular access complications, leaflet damage.
While these risks sound significant, in experienced surgical centres and with careful patient selection, repair success rates are very high and complication rates are acceptably low.
Living with Heart Valve Repair - Long-Term Outlook and Lifestyle
People living with a repaired heart valve can usually anticipate a good long-term outlook, with most returning to vibrant, active, and fulfilling lives. Modern valve repair techniques are highly durable and offer excellent symptom relief, improved function, and increased life expectancy when combined with healthy lifestyle habits and ongoing care.
A. Recovery Experience
In many cases, patients resume normal activities within several weeks, depending on the invasiveness of the repair (open vs minimally invasive). Fatigue and discomfort gradually fade, and many report significantly improved quality of life - more energy, less breathlessness, resumed physical activity and improved heart performance.
B. Lifestyle Adjustments
Post-repair life should include:
-
Regular moderate-intensity exercise (as recommended by the cardiac rehab team).
-
Heart-healthy diet (rich in fruits, vegetables, whole grains, lean proteins) and maintenance of healthy body weight.
-
Avoiding tobacco and limiting alcohol consumption.
-
Routine follow-up with cardiologist for echocardiograms, ECGs and clinical review.
-
Awareness of infection risk: maintain good dental hygiene, notify physician before dental/surgical procedures (to assess need for antibiotic prophylaxis).
-
Adherence to prescribed medications, particularly for blood pressure, heart rhythm or anticoagulation if required.
C. Emotional and Psychological Impact
Undergoing heart valve surgery can be life-changing. Many patients experience relief from debilitating symptoms, increased productivity and better emotional well-being. Still, some may face anxiety about future health, follow-up tests or possible recurrence. Engagement in support groups, counselling or a cardiac rehab community can help adjust to the "new normal."
D. Long-Term Prognosis
When valve repair is successful and the patient adheres to follow-up and lifestyle recommendations, prognosis is excellent:
-
Reduced progression to heart failure.
-
Lower need for prosthetic valve complications (thrombosis, replacement).
-
Better survival rates compared to replacement in appropriate patients.
-
Many patients enjoy decades of active life post-repair - with freedom from many of the symptoms and limitations that preceded surgery.
Top 10 Frequently Asked Questions about Heart Valve Repair
1. What is Heart Valve Repair Surgery?
Heart valve repair is a surgical procedure that corrects problems in one or more of the heart's valves to ensure blood flows properly through the heart. Unlike valve replacement, which involves removing the damaged valve and inserting an artificial one, valve repair preserves the patient's natural valve and restores its normal function.
It is most commonly performed on the mitral or tricuspid valves, though the aortic and pulmonary valves can also be repaired in certain cases. The goal is to improve heart efficiency, reduce symptoms such as shortness of breath and fatigue, and prevent heart failure.
2. Why Would Someone Need Heart Valve Repair?
Heart valve repair is usually recommended for patients suffering from valvular heart disease, where one or more valves do not open or close properly.
Common conditions that may require valve repair include:
-
Mitral valve prolapse or regurgitation: When the valve doesn't close completely, allowing blood to leak backward.
-
Aortic valve stenosis: Narrowing of the valve, restricting blood flow.
-
Congenital valve defects: Abnormalities present at birth.
-
Endocarditis: Infection that damages the valve tissue.
-
Rheumatic heart disease: Scarring from past infections.
Repairing the valve early can prevent further damage to the heart muscle and improve long-term survival.
3. How is Heart Valve Repair Surgery Performed?
Heart valve repair can be done using open-heart surgery or minimally invasive techniques, depending on the patient's condition and the valve involved.
Open-heart surgery:
-
The chest is opened through a sternotomy (a cut along the breastbone).
-
The patient is connected to a heart-lung bypass machine that maintains blood circulation.
-
The surgeon repairs the damaged valve by reshaping the leaflets, tightening or replacing the ring around the valve (annuloplasty), or removing calcium deposits.
Minimally invasive valve repair:
-
Smaller incisions are made between the ribs using specialized instruments or robotic assistance.
-
This approach offers faster recovery, less pain, and smaller scars.
The choice of technique depends on the severity of damage, patient's age, and overall health.
4. What Are the Different Types of Heart Valve Repair Techniques?
Several surgical techniques may be used to repair a damaged valve:
-
Annuloplasty: Reinforcing or tightening the ring around the valve with a synthetic band or ring.
-
Commissurotomy: Removing scar tissue or calcium deposits that prevent valve leaflets from opening fully (used in stenosis).
-
Leaflet repair or resection: Reshaping or trimming valve leaflets to improve closure and stop leakage.
-
Chordal repair or replacement: Replacing stretched or broken tendons (chordae tendineae) that help valve leaflets move.
-
Patching: Repairing holes or tears in the valve using pericardial tissue patches.
The goal is always to preserve the patient's natural valve structure and function whenever possible.
5. Who is a Candidate for Heart Valve Repair?
A person may be a good candidate for heart valve repair if they have:
-
Valve disease that can be corrected without replacement
-
No severe calcification or extensive tissue damage
-
Preserved heart muscle function
-
No active infection or severe comorbidities
Younger patients are often better candidates for repair, as it avoids the need for long-term anticoagulation (blood-thinning) required with mechanical valve replacements.
A detailed evaluation with echocardiography, cardiac MRI, or catheterization helps the surgical team decide whether repair or replacement is most appropriate.
6. What Are the Benefits of Heart Valve Repair Over Valve Replacement?
Heart valve repair offers several advantages compared to replacement:
-
Preserves the natural heart tissue and function.
-
Reduces the risk of infection (endocarditis).
-
No need for lifelong blood-thinning medications in most cases.
-
Improved long-term survival rates and better heart performance.
-
Lower risk of stroke and complications.
Whenever possible, surgeons prefer repair over replacement, especially for mitral and tricuspid valves, as it provides more durable and natural outcomes.
7. What Are the Risks Involved in Heart Valve Repair Surgery?
Like any major surgery, heart valve repair carries some risks, though modern techniques have made it very safe. Potential risks include:
-
Bleeding or infection
-
Blood clots or stroke
-
Irregular heart rhythms (arrhythmias)
-
Reaction to anesthesia
-
Valve leakage or narrowing recurring over time
The overall risk depends on factors like the patient's age, heart function, and existing medical conditions. In experienced hands, success rates for valve repair exceed 95%.
8. How Long Is the Recovery Period After Heart Valve Repair?
Recovery time varies depending on the surgical method:
-
Open-heart repair: Hospital stay of 5-7 days, with complete recovery in 6-8 weeks.
-
Minimally invasive repair: Hospital stay of 3-4 days, recovery in 2-4 weeks.
Patients typically begin cardiac rehabilitation soon after discharge to help regain strength and restore cardiovascular fitness.
Lifestyle modifications, such as eating a heart-healthy diet, exercising moderately, and avoiding smoking, also play an essential role in recovery.
9. What Lifestyle Changes Are Needed After Heart Valve Repair?
After heart valve repair, patients should adopt healthy lifestyle habits to protect heart function and prolong surgical success:
-
Follow-up care: Attend regular cardiology visits for echocardiograms and blood tests.
-
Medication adherence: Take prescribed drugs (such as blood thinners or beta-blockers) as directed.
-
Healthy diet: Limit salt, saturated fat, and processed foods.
-
Exercise: Engage in light to moderate activity as approved by your doctor.
-
Quit smoking and manage stress.
Maintaining overall cardiovascular health helps prevent future valve or heart issues.
10. What is the Long-Term Outlook After Heart Valve Repair?
The long-term outlook after heart valve repair is excellent for most patients. With modern surgical advancements, over 90% of patients experience significant symptom relief and improved heart function.
Many can return to work, enjoy regular physical activity, and lead a normal, active
life.
The durability of valve repair often exceeds 15-20 years, especially
for mitral valve repairs performed by experienced surgeons.
However, lifelong follow-up with a cardiologist is necessary to monitor valve performance and detect any recurrence early.


