Introduction to Heart Valve Replacement
The human heart has four essential valves - the aortic, mitral, tricuspid, and pulmonary valves - that control the direction of blood flow, ensuring that blood moves smoothly through the heart's chambers and out to the body. These valves act as gates that open and close with every heartbeat, maintaining the circulation of oxygen-rich blood. However, when one or more of these valves are damaged, narrowed (stenosis), or fail to close properly (regurgitation), the heart must work harder to pump blood efficiently. Over time, this extra strain can weaken the heart muscle and lead to heart failure if left untreated.
Heart Valve Replacement is a surgical or minimally invasive procedure in which a damaged valve is replaced with a new artificial or biological valve to restore normal blood flow. It is often recommended when valve repair is not possible due to severe damage, calcification, or deformity. This procedure can be life-saving for individuals suffering from advanced valvular heart disease.
With advancements in medical technology, heart valve replacement surgeries have become safer, more effective, and less invasive. Minimally invasive and transcatheter procedures (like TAVR - Transcatheter Aortic Valve Replacement) have dramatically reduced recovery times and improved outcomes, especially in older or high-risk patients. Heart valve replacement not only relieves symptoms such as breathlessness and fatigue but also enhances overall heart function, improving both longevity and quality of life.
Causes and Risk Factors of Heart Valve Disease Leading to Replacement
Heart valve disease can develop from a range of underlying conditions, and when it becomes severe or irreversible, valve replacement may be the best treatment option.
Common Causes
-
Degenerative (age-related) changes: As we age, calcium can build up on the valve leaflets, making them stiff and unable to open or close properly. This is a leading cause of aortic stenosis in older adults.
-
Rheumatic heart disease: In developing regions, untreated streptococcal throat infections can cause rheumatic fever, leading to long-term valve damage, scarring, and deformity - especially of the mitral and aortic valves.
-
Congenital heart defects: Some people are born with malformed valves, such as a bicuspid aortic valve (two flaps instead of three), which predisposes them to early degeneration or narrowing.
-
Infective endocarditis: A bacterial or fungal infection of the heart valves can cause holes, thickening, or scarring, sometimes necessitating valve replacement.
-
Radiation therapy: Patients who have received chest radiation for cancer may develop late-onset valve damage years after treatment.
-
Connective tissue disorders: Conditions such as Marfan syndrome or lupus can weaken valve structures and cause progressive deterioration.
Risk Factors
-
Advanced age is the most significant risk factor, as valves naturally degenerate over time.
-
High blood pressure, high cholesterol, diabetes, and obesity accelerate the wear and tear of heart valves.
-
A family history of heart disease or congenital valve abnormalities increases susceptibility.
-
Smoking and a sedentary lifestyle further increase the risk.
-
Poor dental hygiene and untreated infections may raise the risk of bacterial endocarditis, which can directly affect the valves.
Understanding these causes and risk factors helps in early diagnosis and prevention. While not all causes can be avoided, early medical care and lifestyle management can slow disease progression and delay the need for replacement.
Symptoms and Signs of Heart Valve Disease
Heart valve disease often develops silently, progressing over many years before symptoms become noticeable. In the early stages, patients might feel entirely normal or attribute mild symptoms to ageing or lack of fitness. As the disease advances, however, the heart struggles to maintain normal blood flow, and noticeable symptoms appear.
Common Symptoms Include:
-
Shortness of breath during physical activity or while lying flat, indicating fluid buildup in the lungs.
-
Chest pain or discomfort, especially in cases of aortic stenosis.
-
Extreme fatigue or weakness, as the body receives less oxygenated blood.
-
Heart palpitations or irregular heartbeat, sometimes associated with atrial fibrillation.
-
Swelling of the ankles, feet, or abdomen, which signals fluid retention due to heart failure.
-
Dizziness or fainting spells, often seen in severe aortic valve disease.
Physical Signs Doctors May Detect:
-
A distinct heart murmur (a whooshing or blowing sound) heard through a stethoscope.
-
Signs of heart enlargement or pulmonary congestion on imaging.
-
Elevated jugular venous pressure and fluid retention in severe cases.
Recognizing these symptoms early is vital. Once valve disease progresses to advanced stages, the heart muscle may become permanently damaged, even after valve replacement. Therefore, prompt medical evaluation and regular follow-ups can make a significant difference in outcomes.
Diagnosis of Heart Valve Disease
The diagnosis of heart valve disease begins with a thorough medical history and a physical examination. A cardiologist listens for abnormal heart sounds (murmurs) that indicate turbulent blood flow through a damaged valve. If valve disease is suspected, a series of diagnostic tests are performed to confirm the condition, assess its severity, and plan the most appropriate treatment.
Diagnostic Methods Include:
-
Echocardiography (Echo): This ultrasound-based test is the cornerstone of diagnosis. It visualizes the heart's valves and chambers, measuring the extent of stenosis or regurgitation and evaluating the heart's pumping function.
-
Transesophageal Echocardiogram (TEE): Provides clearer, high-resolution images by inserting a small probe down the esophagus to closely examine valve structure and function.
-
Electrocardiogram (ECG): Detects abnormal rhythms or strain patterns caused by valve disease.
-
Chest X-ray: Helps visualize heart size and detect fluid accumulation in the lungs.
-
Cardiac MRI or CT Scan: Offers detailed imaging of valve anatomy, particularly useful for surgical or catheter-based procedure planning.
-
Cardiac Catheterization: Measures pressures inside the heart and checks for blockages in the coronary arteries before surgery.
Once test results are analyzed, cardiologists classify the disease as mild, moderate, or severe. When symptoms are significant or heart function declines, valve replacement is usually recommended. Early diagnosis through regular checkups can prevent irreversible heart damage and improve surgical outcomes.
Treatment Options for Heart Valve Replacement
When valve disease reaches a critical stage and repair is no longer feasible, heart valve replacement becomes the treatment of choice. The goal of the procedure is to restore normal blood flow, relieve symptoms, and improve heart performance.
Types of Replacement Valves:
-
Mechanical Valves: Made of durable materials like titanium or carbon, these valves are long-lasting and suitable for younger patients. However, they require lifelong anticoagulant medication to prevent blood clots.
-
Biological (Tissue) Valves: Derived from animal tissues (bovine or porcine) or human donors, these valves mimic natural valve movement and do not usually require lifelong blood thinners. They may, however, wear out over time and need replacement after 10-20 years.
-
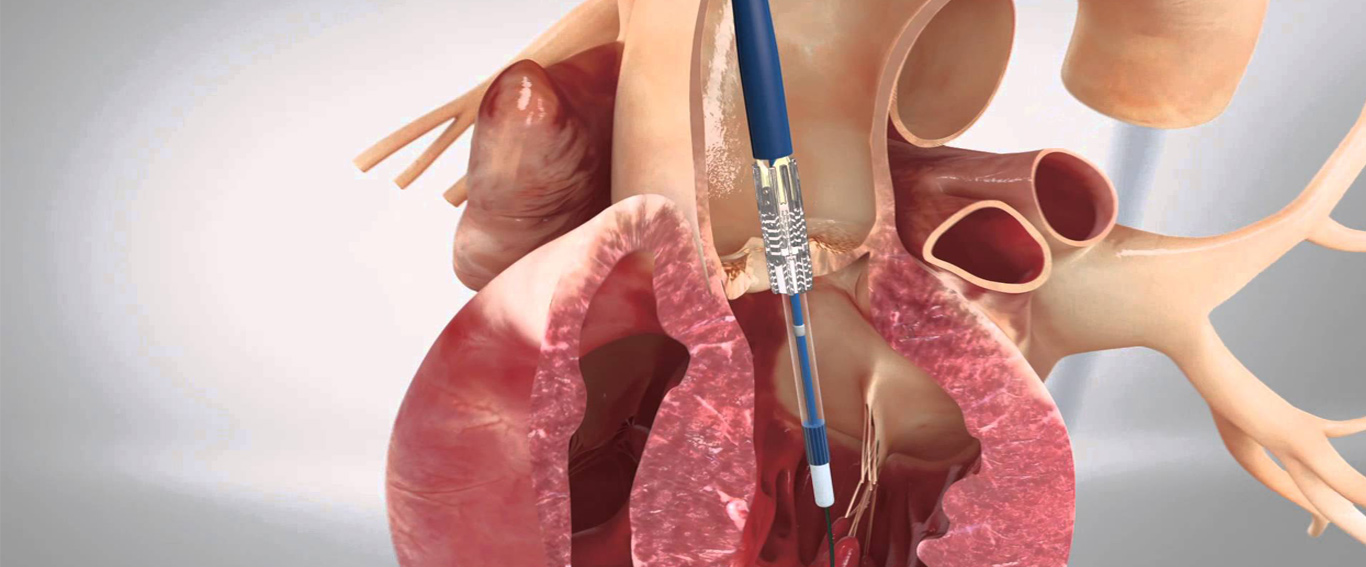
Transcatheter Valves: These are implanted using a catheter, usually through the groin, without open-heart surgery. Transcatheter Aortic Valve Replacement (TAVR) is especially beneficial for elderly or high-risk patients.
Surgical Approaches:
-
Open-heart surgery: The traditional approach, involving a chest incision and cardiopulmonary bypass. This method provides direct access to replace the valve.
-
Minimally invasive surgery: Smaller incisions between the ribs reduce recovery time and post-operative discomfort.
-
Transcatheter procedures (TAVR): A minimally invasive option performed under imaging guidance, often with quicker recovery and fewer complications.
Post-Operative Care:
After valve replacement, patients are closely monitored in intensive care. They are gradually mobilized and enrolled in cardiac rehabilitation programs to rebuild strength. Medications, including anticoagulants and heart-protective drugs, are prescribed. Recovery times vary from weeks to months depending on the procedure type and overall health.
Prevention and Management of Heart Valve Disease
Preventing valve disease and managing it effectively before it becomes severe enough to require replacement is a crucial aspect of heart health.
Prevention Tips:
-
Treat infections promptly: Untreated strep throat can lead to rheumatic fever and valve damage.
-
Maintain excellent oral hygiene: This reduces the risk of bacterial endocarditis.
-
Manage blood pressure, cholesterol, and diabetes: These conditions accelerate heart and valve deterioration.
-
Avoid smoking and maintain a healthy weight: Lifestyle choices play a major role in heart health.
-
Get regular heart check-ups: Early detection allows for timely treatment before complications arise.
Post-Replacement Management:
-
Regular follow-ups with a cardiologist are essential.
-
Patients with mechanical valves need lifelong anticoagulation monitoring.
-
Adhering to medication schedules, dietary guidelines, and exercise recommendations is crucial.
-
Enrolling in cardiac rehabilitation helps improve recovery and heart function.
By focusing on prevention and disciplined management, patients can maintain strong heart health and enjoy a longer, better quality of life after valve replacement.
Complications of Heart Valve Replacement
Although heart valve replacement surgery is generally safe and successful, potential complications can occur during or after the procedure.
Possible Complications Include:
-
Bleeding or infection: Common surgical risks that are carefully managed with antibiotics and close monitoring.
-
Blood clots: Particularly in patients with mechanical valves, requiring strict anticoagulation control.
-
Stroke or heart attack: May result from dislodged blood clots during or after surgery.
-
Arrhythmias: Abnormal heart rhythms can develop after surgery, sometimes requiring pacemaker insertion.
-
Valve degeneration: Biological valves may deteriorate over time, leading to leakage or narrowing.
-
Endocarditis: Infection of the artificial valve, which can be serious and require re-operation.
These risks can be minimized with careful surgical planning, patient education, and consistent follow-up care. Most patients recover well and enjoy significant improvement in symptoms and quality of life after valve replacement.
Living with a Heart Valve Replacement
Life after heart valve replacement often brings a new beginning - with renewed energy, relief from symptoms, and improved heart performance. However, recovery and long-term care are critical to ensure the success of the surgery.
Post-Surgery Recovery:
Patients typically stay in the hospital for several days, followed by a recovery period at home. Activities are resumed gradually under medical supervision. Cardiac rehabilitation programs are invaluable for regaining strength and confidence.
Long-Term Lifestyle Tips:-
Take prescribed medications consistently, especially anticoagulants if you have a mechanical valve.
-
Follow a heart-healthy diet - low in saturated fat, salt, and processed foods.
-
Engage in moderate physical activity as advised by your cardiologist.
-
Avoid smoking and excessive alcohol.
-
Maintain good dental hygiene and inform your dentist about your heart valve condition before any procedure.
-
Report any new symptoms such as breathlessness, swelling, palpitations, or fever immediately.
With modern medical care and lifestyle management, most patients with valve replacements live long, active, and fulfilling lives. Regular check-ups, healthy habits, and awareness are key to ensuring that your new valve functions well for years to come.
Top 10 Frequently Asked Questions about Heart Valve Replacement
1. What is Heart Valve Replacement Surgery?
Heart valve replacement is a surgical procedure that involves removing a damaged or diseased heart valve and replacing it with a new artificial valve to restore normal blood flow through the heart.
The heart has four valves - aortic, mitral, tricuspid, and pulmonary - that ensure blood flows in the right direction. When one or more valves become too narrow (stenosis) or leaky (regurgitation), it strains the heart and leads to symptoms such as fatigue, chest pain, or shortness of breath.
When the valve cannot be repaired, replacement becomes necessary to improve heart function, relieve symptoms, and prevent heart failure.
2. Why Would Someone Need a Heart Valve Replacement?
A person may need heart valve replacement if the valve is severely damaged or deformed, making repair impossible. The most common causes include:
-
Aortic stenosis - narrowing of the aortic valve
-
Mitral regurgitation - leakage of blood backward through the mitral valve
-
Congenital valve defects - abnormalities present from birth
-
Infective endocarditis - infection damaging the valve tissue
-
Rheumatic heart disease - scarring caused by untreated strep throat
-
Degenerative changes - due to aging or calcium buildup
Valve replacement helps restore normal blood circulation, reduce strain on the heart, and enhance the patient's quality of life.
3. What Types of Heart Valves Are Used in Replacement Surgery?
There are two main types of replacement valves used in surgery:
1. Mechanical Valves:
-
Made from durable materials like titanium or carbon.
-
Designed to last a lifetime.
-
Require lifelong use of anticoagulant (blood-thinning) medications to prevent clots.
2. Biological (Tissue) Valves:
-
Made from animal tissue (porcine or bovine) or donated human tissue.
-
Do not usually require long-term anticoagulants.
-
May wear out over time and need replacement after 10-20 years.
The choice depends on the patient's age, health, lifestyle, and medical history. Younger patients often receive mechanical valves, while older patients may benefit from biological ones.
4. How is Heart Valve Replacement Surgery Performed?
Heart valve replacement can be done through open-heart surgery or minimally invasive procedures:
Open-heart surgery:
-
The chest is opened through a sternotomy (incision through the breastbone).
-
The patient is placed on a heart-lung bypass machine to maintain circulation.
-
The damaged valve is removed and replaced with a new one.
-
The heart is restarted, and the chest is closed carefully.
Minimally invasive or transcatheter procedures (TAVR/TAVI):
-
Done through small incisions in the groin or chest.
-
A new valve is inserted via a catheter and expanded inside the old one.
-
Usually suitable for patients at high risk for open-heart surgery.
The choice of technique depends on the patient's age, condition, and overall health.
5. What Are the Symptoms That Indicate the Need for Valve Replacement?
Common symptoms that may suggest severe valve disease requiring replacement include:
-
Shortness of breath, especially during physical activity
-
Chest pain or tightness
-
Dizziness or fainting spells
-
Irregular or rapid heartbeat
-
Fatigue or weakness
-
Swelling in the ankles, feet, or abdomen
If these symptoms persist despite medical therapy, your cardiologist may recommend heart valve replacement surgery to prevent further complications.
6. What Are the Risks Associated with Heart Valve Replacement?
Like any major surgery, heart valve replacement carries certain risks. However, with modern surgical advancements, complications are rare. Possible risks include:
-
Bleeding during or after surgery
-
Infection at the incision site or in the valve (endocarditis)
-
Blood clots leading to stroke or heart attack
-
Irregular heart rhythms (arrhythmias)
-
Reaction to anesthesia
-
Valve failure or leakage (rare)
Experienced cardiac centers and surgeons have success rates exceeding 95%, and most patients recover safely with proper care.
7. How Long Is the Recovery Period After Heart Valve Replacement?
Recovery varies depending on the type of surgery performed:
-
Open-heart surgery: Hospital stay is usually 5-7 days, with full recovery in 6-8 weeks.
-
Minimally invasive or TAVR procedures: Hospital stay is 2-4 days, and patients recover within 2-3 weeks.
During recovery, patients are encouraged to:
-
Participate in cardiac rehabilitation programs
-
Follow a heart-healthy diet
-
Take prescribed medications regularly
-
Avoid strenuous activities until cleared by the doctor
Gradual exercise, adequate rest, and emotional support play an essential role in successful recovery.
8. How Long Does a Replaced Heart Valve Last?
The lifespan of a replacement valve depends on its type:
-
Mechanical valves: Can last 25 years or more, often for a lifetime.
-
Biological (tissue) valves: Usually last 10-20 years before possibly needing replacement.
Factors such as age, lifestyle, and underlying heart conditions can influence valve durability. Regular check-ups and echocardiograms help monitor valve function over time.
9. What Lifestyle Changes Are Needed After Heart Valve Replacement?
To ensure long-term success and protect the new valve, patients should adopt several healthy lifestyle habits:
-
Take all medications as prescribed (especially anticoagulants for mechanical valves).
-
Eat a heart-healthy diet rich in fruits, vegetables, lean proteins, and low sodium.
-
Exercise regularly under medical guidance.
-
Avoid smoking and limit alcohol intake.
-
Monitor INR levels if taking blood thinners like warfarin.
-
Attend all follow-up appointments to detect issues early.
Maintaining a balanced lifestyle helps improve heart performance and reduces the risk of complications.
10. What is the Long-Term Outlook After Heart Valve Replacement?
The long-term prognosis after heart valve replacement is excellent for most patients. The surgery relieves symptoms, restores normal heart function, and significantly improves life expectancy.
With proper care:
-
Most patients return to work and normal activities within a few months.
-
Survival rates exceed 85-90% after 5 years and 75% after 10 years.
-
Quality of life improves dramatically, with reduced fatigue and better exercise tolerance.
Regular follow-up with a cardiologist, adherence to medications, and a healthy lifestyle are key to maintaining long-term success.


