Introduction to Hemorrhoidectomy
A Hemorrhoidectomy is a surgical procedure designed to remove severe or long-standing hemorrhoids - swollen, inflamed veins in the rectum and anus that cause pain, bleeding, and discomfort. Hemorrhoids are among the most common anorectal disorders, affecting millions of adults worldwide. While most mild cases respond to conservative treatments such as dietary changes, topical creams, or minimally invasive therapies, advanced hemorrhoids that fail to improve require definitive surgical management through hemorrhoidectomy.
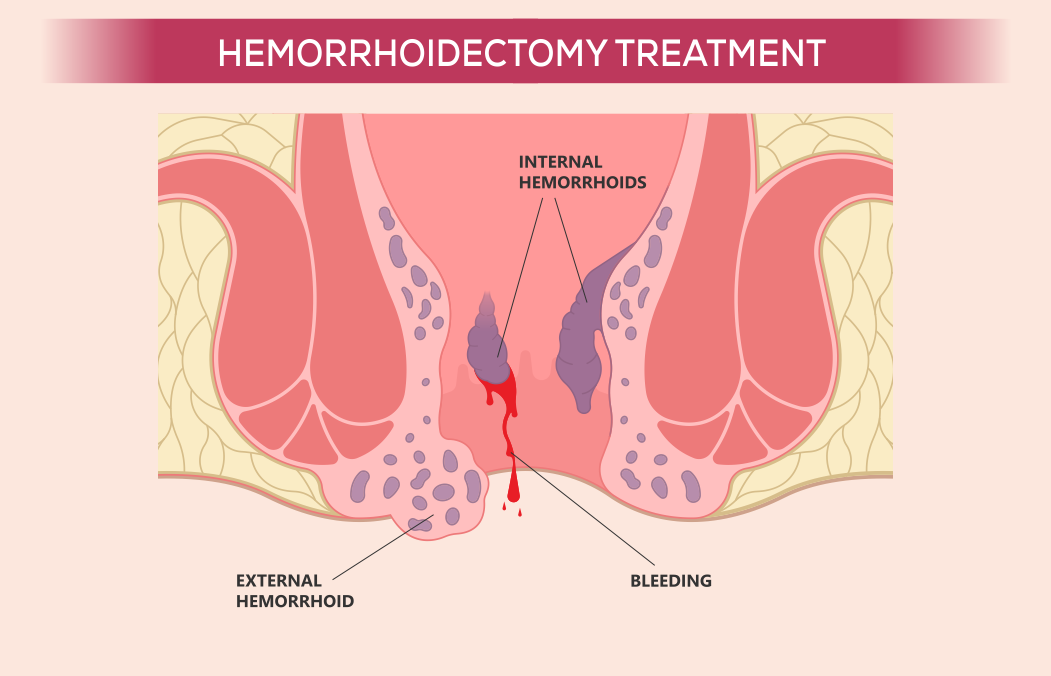
Hemorrhoids are typically classified into two major types:
-
Internal Hemorrhoids: Located inside the rectum, often causing painless bleeding.
-
External Hemorrhoids: Found under the skin surrounding the anus, often associated with pain and swelling.
In severe cases, internal hemorrhoids may prolapse - that is, protrude outside the anal canal - leading to significant discomfort, hygiene issues, and even infection. When these hemorrhoids become thrombosed (clotted) or persistently prolapsed, surgical removal becomes essential to restore normal anal anatomy and function.
Modern hemorrhoidectomy has evolved far beyond traditional open techniques. Advancements in laser surgery, stapled hemorrhoidopexy, and Doppler-guided hemorrhoidal artery ligation have made the procedure safer, less painful, and faster to recover from. These techniques minimize blood loss, postoperative pain, and the risk of recurrence.
Ultimately, a hemorrhoidectomy not only relieves the distressing symptoms of hemorrhoids but also helps patients regain their confidence, mobility, and quality of life. It is a procedure that combines surgical precision with long-term relief.
Causes and Risk Factors of Hemorrhoids
Hemorrhoids form when venous pressure increases in the rectal and anal veins, causing them to stretch, swell, and become inflamed. The anal canal contains vascular cushions that aid in controlling stool passage. However, when these veins are constantly under strain, they lose elasticity and become engorged, resulting in hemorrhoidal disease.
A. Major Causes of Hemorrhoids
-
Chronic Constipation:
Straining during bowel movements increases pressure on the anal veins. Over time, this pressure weakens vein walls and causes hemorrhoids. -
Low-Fiber Diet:
Insufficient dietary fiber leads to hard, dry stools, forcing excessive straining during defecation. -
Prolonged Sitting:
Sitting for extended periods, particularly on the toilet, restricts blood flow to the rectum and contributes to venous congestion. -
Pregnancy and Childbirth:
Hormonal changes, coupled with increased abdominal pressure, make pregnant women prone to hemorrhoids. The condition may worsen after vaginal delivery. -
Obesity:
Excess body weight exerts additional pressure on the pelvic veins, promoting hemorrhoid formation. -
Chronic Diarrhea:
Frequent bowel movements irritate the anal mucosa and cause inflammation of hemorrhoidal tissue. -
Aging:
With age, the connective tissue supporting rectal veins weakens, increasing the risk of hemorrhoidal prolapse. -
Heavy Lifting:
Regularly lifting heavy objects or straining during exercise can elevate intra-abdominal pressure and trigger hemorrhoids. -
Genetic Predisposition:
Some individuals inherit weak venous walls or connective tissues, predisposing them to hemorrhoidal disease.
B. Risk Factors Necessitating Hemorrhoidectomy
While not all hemorrhoids require surgery, certain conditions make a hemorrhoidectomy the best treatment choice:
-
Recurrent bleeding leading to anemia.
-
Severe pain and swelling from thrombosed external hemorrhoids.
-
Large, prolapsed hemorrhoids (Grade III and IV).
-
Chronic prolapse unresponsive to non-surgical interventions.
-
Combined internal and external hemorrhoids causing hygiene issues.
When hemorrhoids persist despite lifestyle modifications or outpatient procedures like rubber band ligation or sclerotherapy, surgical excision becomes the most effective and permanent solution.
Symptoms and Signs of Hemorrhoids
The symptoms of hemorrhoids depend on their type, size, and stage of progression. In the early stages, the condition may cause minor irritation or bleeding, but as it advances, symptoms become more severe and disruptive to daily life.
Common Symptoms Include:
-
Rectal Bleeding:
The most common symptom, often appearing as bright red blood on toilet paper or in the toilet bowl after bowel movements. -
Anal Pain and Burning Sensation:
Pain occurs particularly with external or thrombosed hemorrhoids, and may worsen during sitting or bowel movements. -
Swelling or Lump Near the Anus:
A tender lump can often be felt around the anal opening, representing an external hemorrhoid or a prolapsed internal hemorrhoid. -
Itching and Irritation:
Mucus discharge from prolapsed hemorrhoids can cause itching and irritation of the surrounding skin. -
Mucosal Prolapse:
Internal hemorrhoids may protrude through the anus during defecation and retract spontaneously or require manual repositioning. -
Feeling of Incomplete Evacuation:
The sensation that the bowels haven't completely emptied, even after defecation. -
Painful Defecation:
Due to inflammation, swelling, or thrombosis of hemorrhoids. -
Anemia (in chronic cases):
Recurrent blood loss from bleeding hemorrhoids can result in fatigue, weakness, and low hemoglobin levels.
If these symptoms persist despite conservative measures, it's often a sign that surgical hemorrhoidectomy is necessary for complete resolution.
Diagnosis of Hemorrhoidectomy
A precise diagnosis is critical to rule out other causes of rectal bleeding or discomfort, such as fissures, abscesses, polyps, or colorectal cancer.
A. Clinical Evaluation
The doctor begins with a detailed medical history, focusing on bowel habits, dietary intake, family history, and previous treatments.
B. Diagnostic Tests and Examinations
-
Visual Inspection:
External hemorrhoids or prolapsed internal hemorrhoids are visible around the anal opening. -
Digital Rectal Examination (DRE):
The physician uses a gloved, lubricated finger to feel for lumps, tenderness, or thickening inside the rectum. -
Anoscopy:
A short, lighted tube allows direct visualization of internal hemorrhoids. -
Proctoscopy or Sigmoidoscopy:
Used to examine deeper parts of the rectum and sigmoid colon, ruling out other causes of bleeding. -
Colonoscopy:
Recommended for patients over 50 or with a family history of colorectal disease to exclude malignancy.
C. Classification by Grade
-
Grade I: Hemorrhoids bleed but do not prolapse.
-
Grade II: Prolapse during bowel movement but retract spontaneously.
-
Grade III: Require manual reduction.
-
Grade IV: Permanently prolapsed and irreducible.
Grades III and IV typically require surgical hemorrhoidectomy for complete treatment.
Treatment Options for Hemorrhoidectomy
Treatment depends on the severity and grade of hemorrhoids.
A. Non-Surgical Management
-
Lifestyle Changes:
-
Eat a high-fiber diet (whole grains, vegetables, fruits).
-
Drink plenty of water (at least 2-3 liters per day).
-
Avoid straining or prolonged sitting during defecation.
-
-
Medications:
-
Topical creams (hydrocortisone, lidocaine).
-
Stool softeners and mild laxatives to ease bowel movements.
-
Anti-inflammatory agents to reduce swelling.
-
-
Office Procedures:
-
Rubber Band Ligation: Elastic bands cut off blood flow to hemorrhoids, causing them to shrink.
-
Sclerotherapy: A chemical injection causes veins to collapse.
-
Infrared Coagulation: Heat destroys small internal hemorrhoids.
-
B. Surgical Treatment (Hemorrhoidectomy Techniques)
-
Conventional Hemorrhoidectomy (Open or Closed):
The most common and effective approach, involving surgical excision of hemorrhoids using a scalpel, scissors, or electrocautery.-
Open technique: Wound left open to heal naturally.
-
Closed technique: Wound sutured for faster healing.
-
-
Stapled Hemorrhoidopexy (PPH):
A circular stapler repositions the hemorrhoids and removes excess mucosal tissue.-
Less pain and faster recovery.
-
Minimal blood loss.
-
-
Laser Hemorrhoidectomy:
Uses laser energy to precisely vaporize hemorrhoidal tissue with minimal trauma, bleeding, and postoperative discomfort. -
Doppler-Guided Hemorrhoidal Artery Ligation (DG-HAL):
Ultrasound identifies arteries supplying hemorrhoids, which are then tied off to cut blood flow and shrink hemorrhoidal tissue.
Each technique is selected based on the patient's condition, hemorrhoid grade, and medical history.
Prevention and Management After Hemorrhoidectomy
Preventing hemorrhoid recurrence after surgery involves maintaining bowel regularity and minimizing rectal strain.
A. Preventive Measures
-
Consume fiber-rich foods daily.
-
Stay hydrated at all times.
-
Avoid prolonged sitting or standing.
-
Exercise regularly to improve circulation.
-
Refrain from straining during bowel movements.
B. Postoperative Management
-
Use stool softeners to prevent constipation.
-
Take warm sitz baths 2-3 times a day to relieve pain and reduce swelling.
-
Maintain excellent anal hygiene using mild soap and water.
-
Avoid spicy and greasy foods that may irritate the rectum.
-
Follow up regularly with the surgeon to monitor healing progress.
Most patients resume normal activity within 2-3 weeks after surgery.
Complications of Hemorrhoidectomy
While modern hemorrhoidectomy is generally safe, some potential complications may occur, most of which are minor and temporary.
A. Common Complications
-
Pain and Discomfort: Common during the first week; managed with analgesics and sitz baths.
-
Bleeding: Light bleeding is expected; heavy bleeding requires medical attention.
-
Infection: Prevented through antibiotics and good hygiene.
-
Urinary Retention: Temporary due to pelvic swelling; resolves naturally.
-
Anal Stenosis: Rare narrowing of the anal canal due to scarring.
-
Recurrence: Uncommon when proper care and lifestyle modifications are maintained.
Careful postoperative care significantly minimizes these risks.
Living with the Condition After Hemorrhoidectomy
After hemorrhoidectomy, patients typically experience a dramatic improvement in quality of life. Pain subsides, bleeding stops, and normal bowel movements resume within weeks.
A. Recovery Timeline
-
First Week: Pain and swelling gradually decrease.
-
2-3 Weeks: Most patients return to work and normal activities.
-
1-2 Months: Complete healing and tissue recovery occur.
B. Lifestyle Adjustments
-
Eat high-fiber foods daily to maintain soft stools.
-
Stay active - walking and light exercises aid circulation.
-
Avoid sitting for long durations.
-
Continue proper hydration habits permanently.
C. Long-Term Outlook
A well-performed hemorrhoidectomy offers permanent relief for more than 95% of patients. With appropriate lifestyle management, recurrence is rare. Most patients report a restored sense of confidence, freedom, and comfort after complete recovery.
Top 10 Frequently Asked Questions about Hemorrhoidectomy
1. What is a Hemorrhoidectomy?
A hemorrhoidectomy is a surgical procedure to remove swollen and inflamed veins (hemorrhoids) in the rectum and anus that cause pain, bleeding, itching, or discomfort. It is typically recommended when other treatments such as medications, lifestyle changes, or minimally invasive procedures (like rubber band ligation or sclerotherapy) fail to provide relief.
During the surgery, the surgeon removes the hemorrhoidal tissue and seals the blood vessels to prevent bleeding. It's usually performed under spinal or general anesthesia, depending on the case.
Hemorrhoidectomy is considered the most effective long-term solution for severe or recurrent hemorrhoids.
2. When is a Hemorrhoidectomy Necessary?
A hemorrhoidectomy is usually recommended in the following situations:
-
Large internal hemorrhoids (Grade III or IV) that protrude outside the anus.
-
External hemorrhoids causing severe pain or bleeding.
-
Thrombosed hemorrhoids (blood clots in external hemorrhoids).
-
Failure of nonsurgical treatments like creams, dietary changes, or rubber band ligation.
-
Persistent symptoms such as bleeding, itching, or discomfort affecting daily life.
Your doctor will recommend surgery after evaluating the severity of your hemorrhoids and your overall health condition.
3. How is Hemorrhoidectomy Performed?
There are several surgical techniques for hemorrhoid removal, and the choice depends on the size and location of the hemorrhoids:
1. Conventional (Open) Hemorrhoidectomy:
-
The surgeon removes the hemorrhoids using a scalpel, laser, or cautery device.
-
The wound may be left open to heal naturally or closed with stitches.
2. Closed Hemorrhoidectomy:
-
The wound is sutured after hemorrhoid removal, leading to faster healing and less postoperative pain.
3. Stapled Hemorrhoidectomy (PPH):
-
A circular stapling device removes excess tissue and repositions the hemorrhoids inside the rectum.
-
It's less painful and has a shorter recovery time but is suitable for specific cases.
4. Laser Hemorrhoidectomy:
-
Uses laser energy to shrink hemorrhoidal tissue with minimal bleeding and faster recovery.
4. What Are the Benefits of Hemorrhoidectomy?
A hemorrhoidectomy offers several long-term benefits:
-
Permanent relief from pain, bleeding, and itching.
-
Improved quality of life and ability to perform daily activities without discomfort.
-
Lower recurrence rate compared to non-surgical treatments.
-
Better control of symptoms like prolapse (bulging of tissue outside the anus).
While recovery can be uncomfortable, the results are usually excellent and long-lasting.
5. What Are the Risks or Complications of a Hemorrhoidectomy?
Like any surgical procedure, a hemorrhoidectomy carries certain risks, although complications are rare when performed by experienced surgeons. Possible complications include:
-
Pain or discomfort during recovery (most common)
-
Bleeding during or after surgery
-
Infection at the surgical site
-
Urinary retention (temporary)
-
Anal narrowing or stricture (rare)
-
Delayed wound healing
Most side effects are temporary and manageable with medication and proper post-operative care.
6. What is the Recovery Time After Hemorrhoidectomy?
Recovery time depends on the surgical method and the patient's overall health. Typically:
-
Initial healing takes about 2-3 weeks.
-
Full recovery may take 4-6 weeks.
Patients may experience mild pain, swelling, or discomfort during bowel movements for the first few days. Pain-relief medications, warm sitz baths, and a high-fiber diet help speed up recovery.
Most patients can return to light activities within one week and resume normal work after 2-3 weeks, depending on the type of job.
7. What Should I Expect After a Hemorrhoidectomy?
After surgery, mild pain, swelling, or bleeding during bowel movements is normal. Your doctor will prescribe:
-
Pain medications for comfort
-
Antibiotics to prevent infection
-
Laxatives or stool softeners to ease bowel movements
You'll be advised to take sitz baths (soaking the anal area in warm water) 2-3 times daily to reduce pain and promote healing.
Follow-up appointments are important to ensure proper wound healing and rule out any complications.
8. How Can I Manage Pain After Hemorrhoidectomy?
Pain management is a key part of recovery. Here are effective ways to reduce discomfort:
-
Take prescribed painkillers as directed by your doctor.
-
Use warm sitz baths several times daily.
-
Avoid sitting for long periods; use a soft cushion or donut pillow.
-
Eat high-fiber foods and drink plenty of water to prevent constipation.
-
Avoid straining during bowel movements.
With proper care, pain usually subsides within one to two weeks.
9. Are There Alternatives to Hemorrhoidectomy?
Yes, several non-surgical or minimally invasive alternatives exist, depending on the severity of hemorrhoids:
-
Rubber band ligation: Cuts off blood supply to the hemorrhoid.
-
Sclerotherapy: Injection of a chemical solution to shrink hemorrhoids.
-
Infrared coagulation: Uses heat to destroy hemorrhoidal tissue.
-
Cryotherapy: Freezing the hemorrhoid with liquid nitrogen.
These are effective for mild to moderate hemorrhoids, but for severe or recurrent cases, surgical hemorrhoidectomy remains the gold standard.
10. What Lifestyle Changes Can Prevent Hemorrhoids After Surgery?
Adopting healthy habits after surgery helps prevent recurrence and supports overall bowel health:
-
Eat a high-fiber diet: Include fruits, vegetables, and whole grains.
-
Stay hydrated: Drink at least 8-10 glasses of water daily.
-
Avoid prolonged sitting or standing.
-
Exercise regularly to improve digestion and circulation.
-
Do not strain during bowel movements - use stool softeners if necessary.
-
Maintain a healthy weight.
These lifestyle changes ensure smooth bowel function and reduce the risk of hemorrhoid recurrence.


