Introduction to Hernia Revision Surgery
A Hernia Revision Surgery is a specialized surgical procedure performed to correct a recurrent or failed hernia repair. While hernia repair surgeries are common and typically successful, there are instances where the hernia reappears due to factors such as improper healing, mesh complications, infection, or excessive physical strain after the first operation. In such cases, revision surgery becomes essential to restore abdominal wall integrity and prevent further complications.
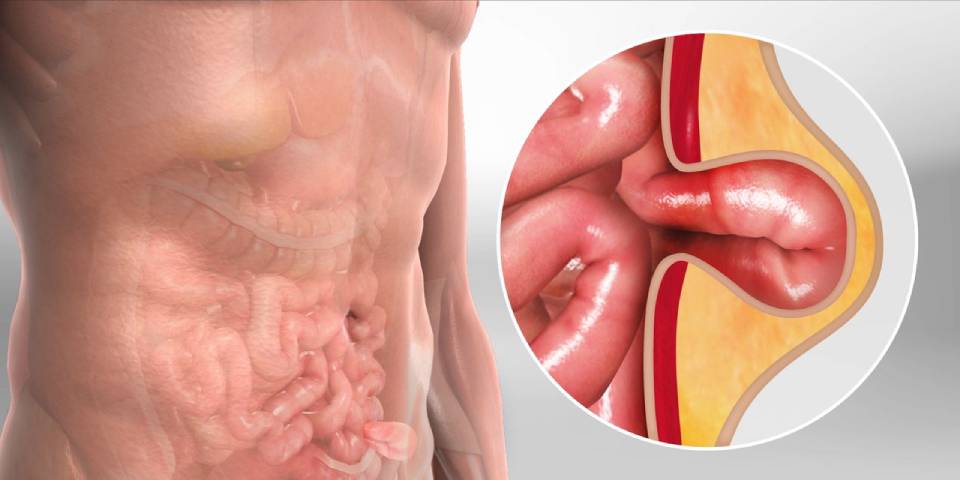
A hernia occurs when an internal organ or tissue protrudes through a weak spot in the surrounding muscle or connective tissue (fascia). The most common types include inguinal (groin), umbilical (navel), incisional (post-surgery scar), femoral, and hiatal (upper stomach) hernias.
When a previously repaired hernia reoccurs, the condition is referred to as a recurrent hernia. Hernia revision surgery aims to:
-
Repair the weakened or damaged area of the abdominal wall.
-
Remove or reposition old surgical mesh.
-
Address scar tissue or infection from prior surgery.
-
Restore normal anatomy and function.
Hernia revision procedures are typically more complex and delicate than primary repairs due to the presence of scar tissue, previous mesh material, and changes in anatomy from earlier surgery. They require the expertise of an experienced surgeon who specializes in abdominal wall reconstruction.
Modern advancements, including robotic-assisted and laparoscopic revision techniques, have made it possible to perform this surgery with greater precision, reduced pain, and faster recovery times. For patients suffering from chronic pain, bulging, or discomfort after an initial hernia repair, revision surgery offers a path to lasting relief and improved quality of life.
Causes and Risk Factors Leading to Hernia Revision Surgery
A recurrent or failed hernia repair can result from a combination of surgical, biological, and lifestyle factors. Understanding these causes is crucial to prevent recurrence after revision surgery.
A. Common Causes of Hernia Recurrence
-
Inadequate Initial Repair:
If the initial hernia repair was poorly executed or tension was not evenly distributed, the site may fail to heal properly. -
Infection at the Repair Site:
Postoperative infections can weaken tissue and lead to breakdown of the repaired area. -
Poor Quality Mesh or Improper Placement:
Incorrect mesh size, folding, or migration of the mesh can cause structural failure and hernia recurrence. -
Excessive Physical Strain Post-Surgery:
Engaging in heavy lifting or intense activity too soon after surgery puts pressure on the repair site. -
Chronic Coughing or Constipation:
Conditions that repeatedly increase abdominal pressure can gradually weaken the surgical repair. -
Smoking and Poor Nutrition:
Both impair tissue healing and collagen formation, leading to poor surgical outcomes. -
Obesity:
Excess weight exerts continuous pressure on the abdominal wall, increasing the likelihood of hernia recurrence. -
Age and Weak Connective Tissue:
Natural tissue degeneration with age can contribute to repair failure.
B. Risk Factors for Needing Hernia Revision Surgery
-
Multiple previous abdominal surgeries.
-
Use of inappropriate mesh material.
-
Failure to follow postoperative restrictions.
-
Diabetes or other metabolic disorders delaying healing.
-
Smoking or alcohol use during recovery.
-
Chronic lung disease causing frequent coughing.
Revision surgery is particularly complex when infection, large defects, or multiple recurrences are involved. Such cases often require customized surgical planning and sometimes the involvement of reconstructive plastic surgeons.
Symptoms and Signs Indicating the Need for Hernia Revision Surgery
Symptoms of hernia recurrence or failed repair often mimic those of the original hernia, but may also include additional discomfort due to scarring or mesh complications.
A. Common Symptoms Include:
-
Bulge or Lump at the Site of Previous Surgery:
The most typical sign of recurrence; may increase in size when standing or straining. -
Pain or Discomfort:
Aching, pulling, or sharp pain at or near the original surgical site. -
Swelling or Redness:
Inflammation around the incision or mesh site may suggest infection. -
Feeling of Pressure or Heaviness:
A persistent sensation of fullness in the affected area. -
Digestive Symptoms (in Abdominal Hernias):
Nausea, bloating, or constipation may occur if intestinal loops are involved. -
Mesh-Related Pain:
If the previous mesh becomes folded or displaced, it can irritate nearby nerves or tissues.
B. Severe Symptoms Requiring Immediate Medical Attention
-
Severe abdominal pain.
-
Vomiting or inability to pass gas/stool (signs of bowel obstruction).
-
Fever and chills (possible infection).
-
Sudden enlargement of hernia with intense pain (possible strangulation).
When such symptoms appear, prompt surgical evaluation is critical to prevent life-threatening complications like intestinal strangulation or gangrene.
Diagnosis of Recurrent Hernia (Before Revision Surgery)
Diagnosing a recurrent hernia requires a combination of clinical assessment, imaging tests, and detailed surgical history review.
A. Clinical Examination
The surgeon performs a physical exam while the patient is standing and lying down. The doctor checks for visible bulges, tenderness, and changes with coughing or straining.
B. Diagnostic Tests
-
Ultrasound:
A non-invasive tool to detect small or hidden hernias. -
CT Scan (Computed Tomography):
Provides detailed images of abdominal wall structures, previous mesh placement, and tissue weakness. -
MRI Scan:
Useful for assessing soft tissue damage, scar tissue, or mesh migration. -
Herniography:
Involves injecting a contrast dye into the abdominal cavity to visualize the hernia defect. -
Blood Tests:
Performed to rule out infection or inflammatory responses before planning surgery.
Once the exact site, size, and cause of recurrence are identified, a customized surgical plan is developed for optimal outcomes.
Treatment Options and Surgical Techniques for Hernia Revision Surgery
Hernia revision surgery requires precision and expertise because scar tissue and mesh from previous operations make the anatomy more complex. The surgical approach depends on the location, type, and size of the hernia, as well as the patient's general health.
A. Surgical Techniques
-
Open Hernia Revision:
A traditional method where the surgeon makes an incision over the previous repair site, removes damaged mesh or scar tissue, and repairs the defect using a new mesh or sutures.-
Ideal for large or complicated recurrences.
-
Allows better visualization of scarred tissues.
-
-
Laparoscopic Hernia Revision:
Involves small keyhole incisions and insertion of a laparoscope (camera). The surgeon repairs the hernia from within using specialized instruments.-
Less pain and quicker recovery.
-
Reduced wound complications and scarring.
-
-
Robotic-Assisted Hernia Revision:
The most advanced form of revision surgery. Robotic systems offer greater precision, 3D visualization, and superior suturing capability.-
Especially useful for complex or multiple recurrent hernias.
-
-
Mesh Reconstruction or Removal:
If old mesh is infected, wrinkled, or displaced, it is removed and replaced with new biocompatible mesh.
B. Anesthesia and Hospital Stay
-
Typically performed under general anesthesia.
-
Hospital stay varies from 1 to 3 days, depending on the complexity of the procedure.
C. Postoperative Recovery
-
Patients are encouraged to walk within 24 hours.
-
Full recovery generally takes 4-6 weeks.
-
Pain is managed through medications and gradual physical rehabilitation.
Prevention and Management After Hernia Revision Surgery
The success of revision surgery largely depends on postoperative care and preventive lifestyle choices.
A. Prevention Tips
-
Avoid Heavy Lifting:
For at least 6-8 weeks after surgery to prevent strain on the repaired site. -
Maintain Healthy Weight:
Reduces constant pressure on the abdominal wall. -
Quit Smoking:
Smoking interferes with wound healing and weakens connective tissue. -
High-Fiber Diet:
Prevents constipation, which otherwise increases intra-abdominal pressure. -
Control Chronic Cough or Lung Disease:
Treat respiratory conditions to avoid excessive abdominal strain. -
Adhere to Follow-Up Appointments:
Regular check-ups ensure early detection of potential issues.
B. Management After Surgery
-
Use abdominal binders or support garments as advised.
-
Take prescribed painkillers and antibiotics.
-
Monitor incision sites for redness, swelling, or discharge.
-
Gradually resume physical activity as approved by your surgeon.
Proper postoperative management minimizes recurrence risk and ensures a stable and durable repair.
Complications of Hernia Revision Surgery
Although generally safe, revision hernia surgery carries higher risks compared to primary repairs due to the presence of scar tissue and prior mesh.
Common Complications Include:
-
Infection:
Especially if old mesh was infected. Managed with antibiotics or removal. -
Bleeding or Hematoma:
May occur at the surgical site. -
Seroma Formation:
Fluid accumulation beneath the skin; often resolves with drainage. -
Nerve Injury or Chronic Pain:
May result from nerve entrapment during surgery; usually temporary. -
Recurrence:
Although rare with proper care, can still occur if risk factors persist. -
Bowel Injury:
Possible when intestines adhere to old mesh or scar tissue.
The risk of these complications can be minimized by choosing an experienced surgeon and following all postoperative care instructions carefully.
Living with the Condition After Hernia Revision Surgery
Life after hernia revision surgery typically brings long-term relief and restored functionality. Most patients resume normal activities within a few weeks and experience minimal discomfort once healing is complete.
A. Recovery Timeline
-
First Week: Pain and swelling reduce with medication.
-
Weeks 2-4: Resume light household activities and walking.
-
After 6 Weeks: Gradual return to full physical activity and exercise.
B. Diet and Lifestyle
-
Consume fiber-rich foods like whole grains, fruits, and vegetables.
-
Stay hydrated to prevent constipation.
-
Maintain good posture to support abdominal muscles.
C. Emotional and Physical Well-being
Hernia recurrence can be emotionally distressing. Patients often feel anxious about a second operation. However, with modern surgical advancements, revision surgeries have excellent success rates and help restore confidence, mobility, and normalcy in daily life.
Top 10 Frequently Asked Questions about Hernia Revision Surgery
1. What is Hernia Revision Surgery?
Hernia revision surgery (also known as hernia repair revision or recurrent hernia repair) is a surgical procedure performed to correct a recurrent or failed hernia repair. A hernia may return after initial surgery due to factors like infection, poor healing, mesh complications, or excessive strain on the surgical site.
In revision surgery, the surgeon identifies and repairs the defect again—often by removing or replacing old mesh, reinforcing the abdominal wall, and ensuring stronger tissue support to prevent further recurrence.
2. Why Does a Hernia Recur After Surgery?
A hernia can recur for various reasons, even after successful initial repair. Common causes include:
-
Infection at or around the mesh or surgical site
-
Improper healing due to smoking, diabetes, or obesity
-
Weak connective tissue in the abdominal wall
-
Excessive strain from heavy lifting or chronic coughing
-
Inappropriate mesh placement or use of poor-quality mesh
-
Surgical technique issues
Hernia recurrence is more likely if the original repair was performed under emergency conditions or without adequate reinforcement.
3. When is Hernia Revision Surgery Needed?
Your doctor may recommend revision surgery if you experience one or more of the following:
-
A visible bulge or lump at the site of previous repair
-
Pain or discomfort that persists or worsens after initial surgery
-
Swelling or redness around the surgical site
-
Digestive symptoms such as nausea, vomiting, or bowel obstruction
-
Infection or mesh rejection symptoms (drainage, fever, inflammation)
Hernia revision is advised when symptoms affect quality of life or pose a risk of complications like strangulation or obstruction.
4. How is Hernia Revision Surgery Performed?
Hernia revision surgery can be performed using open or minimally invasive (laparoscopic/robotic) techniques, depending on the hernia's location, size, and complexity.
Open surgery:
-
The surgeon reopens the previous incision.
-
Scar tissue and old mesh are carefully removed if necessary.
-
The defect is repaired with sutures and reinforced with new mesh if appropriate.
Laparoscopic or robotic surgery:
-
Performed through small incisions using advanced tools and a camera.
-
Allows precise dissection and repair with minimal tissue trauma.
-
Offers faster recovery and lower infection risk.
Your surgeon will determine the best approach based on your medical history and prior surgical outcomes.
5. What Are the Challenges in Hernia Revision Surgery?
Revision hernia surgery is often more complex than the first operation because of:
-
Scar tissue (adhesions) from the previous surgery
-
Altered anatomy and weakened tissues
-
Presence of old mesh that may need removal
-
Risk of organ injury, especially if intestines or other structures are involved
Hence, it's crucial that the procedure is performed by an experienced hernia specialist or reconstructive surgeon who frequently handles revision cases.
6. What Are the Risks and Complications of Hernia Revision Surgery?
While the success rate is high, revision surgery carries certain risks, such as:
-
Bleeding or infection
-
Seroma or fluid buildup
-
Recurrence of hernia (especially in complex or large cases)
-
Injury to surrounding organs (intestine, bladder, nerves)
-
Chronic pain or numbness
-
Mesh-related complications (if used again)
However, with modern surgical techniques, the risk of recurrence after revision surgery is significantly reduced when proper precautions are followed.
7. What Is the Recovery Time After Hernia Revision Surgery?
Recovery depends on the surgical method, hernia size, and patient health:
-
Laparoscopic/robotic repair: Recovery is faster, with most patients returning to work in 2-3 weeks.
-
Open repair: Full recovery may take 4-6 weeks, especially for complex hernias.
During recovery, patients are advised to:
-
Avoid heavy lifting or strenuous activity for at least 6 weeks.
-
Follow a high-protein, nutrient-rich diet for tissue healing.
-
Attend follow-up appointments to ensure proper recovery.
-
Wear abdominal support garments if prescribed.
8. How Can I Prevent Another Hernia After Revision Surgery?
To reduce the risk of another recurrence:
-
Maintain a healthy body weight to reduce abdominal pressure.
-
Quit smoking, as it delays wound healing.
-
Avoid heavy lifting or straining after surgery.
-
Manage chronic cough or constipation that increases abdominal pressure.
-
Follow your surgeon's rehabilitation plan and activity guidelines.
-
Focus on core strengthening exercises after complete recovery (under medical supervision).
A disciplined recovery approach can drastically lower the chance of hernia recurrence.
9. What Are the Success Rates of Hernia Revision Surgery?
Modern hernia revision techniques have greatly improved outcomes.
-
Success rates range from 85% to 95%, depending on the complexity of the case and patient health.
-
Laparoscopic and robotic revisions offer fewer complications and faster recovery than traditional open repairs in many cases.
Choosing a specialized hernia surgeon with experience in complex revisions is the key to achieving the best results and preventing future recurrence.
10. What Is the Cost and Insurance Coverage for Hernia Revision Surgery?
The cost of hernia revision surgery varies based on:
-
Type of procedure (open vs. laparoscopic)
-
Hospital or surgical center fees
-
Use of mesh or other materials
-
Surgeon's expertise and geographical location
Most insurance plans cover hernia revision surgery if it is medically necessary. Patients are encouraged to check coverage details, pre-authorization requirements, and co-pay options with their insurance provider before scheduling surgery.


