Introduction to Hiatal Hernia Repair
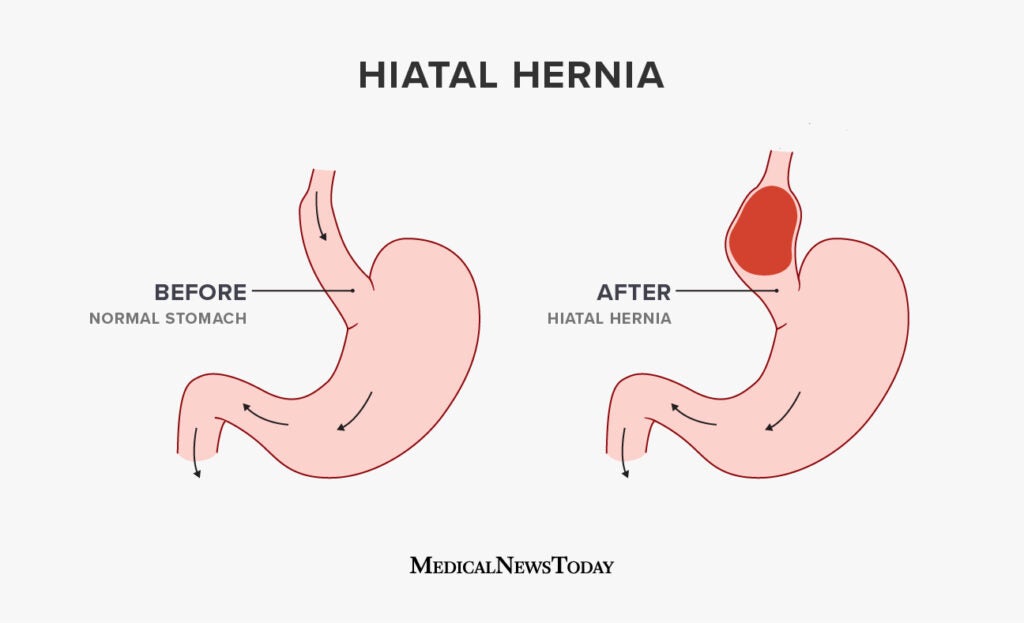
A hiatal hernia occurs when part of the stomach or another abdominal organ pushes upward through the diaphragm into the chest cavity through an opening called the hiatus. The diaphragm is a large muscle that separates the chest from the abdomen and plays an essential role in breathing. Normally, the esophagus passes through this opening to connect with the stomach. However, when the hiatus becomes enlarged or weakened, a portion of the stomach can slip upward, leading to a hiatal hernia.
There are two main types of hiatal hernias: sliding hiatal hernias and paraesophageal hiatal hernias. In a sliding hiatal hernia, the stomach and the lower part of the esophagus slide up into the chest during swallowing or straining, which often causes acid reflux. In a paraesophageal hernia, part of the stomach pushes beside the esophagus, potentially leading to more serious complications like strangulation or obstruction.
Hiatal hernia repair is a surgical procedure performed to correct this condition when it becomes symptomatic or complicated. The goal of the surgery is to return the displaced portion of the stomach to its normal position, tighten the opening in the diaphragm, and strengthen the junction between the esophagus and stomach to prevent reflux. In some cases, a fundoplication (wrapping the upper part of the stomach around the lower esophagus) is performed alongside the repair to enhance reflux control.
While many hiatal hernias cause mild symptoms and can be managed with medication and lifestyle changes, large or complicated hernias often require surgery. Thanks to modern advances, most repairs are now done laparoscopically or robotically, offering smaller incisions, reduced pain, faster recovery, and excellent long-term outcomes.
Causes and Risk Factors of Hiatal Hernia
A hiatal hernia develops primarily due to weakening of the diaphragm muscles or increased pressure inside the abdomen. This combination allows the stomach or other abdominal organs to push upward through the esophageal hiatus.
Common Causes Include:
-
Age-related muscle weakening:
As people age, the diaphragm and surrounding tissues lose their elasticity and strength, making it easier for the stomach to slip through the opening. -
Increased intra-abdominal pressure:
Pressure rises inside the abdomen due to chronic coughing, heavy lifting, obesity, pregnancy, or repeated straining during bowel movements. -
Injury or trauma:
Previous surgeries or blunt injuries to the abdomen or chest can disrupt or enlarge the diaphragm opening. -
Congenital defects:
Some individuals are born with an unusually large hiatus, predisposing them to develop a hernia. -
Lifestyle factors:
Smoking, poor posture, or lifting heavy objects frequently can also increase the likelihood of developing a hernia.
Risk Factors:
-
Age: Most common in people over 50.
-
Obesity: Extra weight puts added strain on the abdominal wall.
-
Pregnancy: Repeated pregnancies can weaken diaphragm muscles.
-
Chronic straining: From constipation or persistent cough.
-
Sedentary lifestyle: Lack of exercise leads to weak abdominal muscles and poor posture.
Not all hiatal hernias require surgery, but when they lead to severe reflux, bleeding, obstruction, or strangulation, surgical hiatal hernia repair becomes essential to prevent life-threatening complications.
Symptoms and Signs of Hiatal Hernia
Many individuals with a hiatal hernia experience mild or no symptoms at all, especially in early stages. However, larger hernias or those causing reflux often produce distinct and sometimes debilitating symptoms.
Common Symptoms:
-
Heartburn and Acid Reflux:
The most frequent complaint, caused when stomach acid backs up into the esophagus. This leads to burning sensations in the chest, especially after eating or lying down. -
Regurgitation of Food or Acid:
Patients may experience sour or bitter fluid rising into the throat or mouth. -
Difficulty Swallowing (Dysphagia):
The hernia may narrow the lower esophagus, making it hard for food to pass. -
Chest Pain or Discomfort:
Sometimes mistaken for cardiac pain, this occurs due to acid irritation or compression by the herniated stomach. -
Bloating and Belching:
Trapped air can cause a sensation of fullness after small meals. -
Shortness of Breath:
Large hernias can push on the lungs, leading to difficulty breathing. -
Vomiting or Nausea:
Especially if the hernia becomes obstructed. -
Anemia or Fatigue:
Chronic bleeding from an ulcerated herniated stomach lining may lead to low hemoglobin.
Severe or Complicated Signs:
In paraesophageal hernias, part of the stomach may become trapped or twisted, cutting off its blood supply - a condition called gastric volvulus or strangulation. This causes sudden severe chest pain, vomiting, and difficulty swallowing and requires emergency surgical repair.
Persistent symptoms despite medication or complications such as these are strong indicators that surgical repair is necessary.
Diagnosis of Hiatal Hernia
Diagnosing a hiatal hernia involves a combination of clinical evaluation, imaging, and endoscopic procedures. Because symptoms can mimic those of acid reflux disease or heart disorders, proper diagnosis is vital before deciding on treatment.
Diagnostic Procedures:
-
Physical Examination:
Doctors will review symptoms, medical history, and risk factors. -
Barium Swallow X-ray:
The patient swallows a contrast liquid (barium), which highlights the esophagus and stomach on X-ray, clearly showing the hernia's size and shape. -
Upper Endoscopy (EGD):
A flexible tube with a camera is inserted through the mouth to view the esophagus, stomach, and diaphragm opening. It helps detect inflammation, ulcers, or tissue damage caused by acid reflux. -
Esophageal Manometry:
Measures pressure and muscle coordination of the esophagus to check for swallowing disorders. -
pH Monitoring:
Evaluates acid levels in the esophagus to confirm reflux severity. -
CT Scan or MRI:
May be used in large or complex hernias for detailed imaging, especially if there's a suspicion of organ strangulation.
These diagnostic tests help determine not only the presence of a hiatal hernia but also its type, size, and severity, guiding whether conservative management or surgical repair is appropriate.
Treatment Options - Hiatal Hernia Repair and Other Therapies
The treatment of a hiatal hernia depends on the severity of symptoms, hernia size, and the risk of complications.
Non-Surgical Management:
For mild cases or sliding hernias without major symptoms:
-
Lifestyle modifications: Eat smaller meals, avoid lying down after eating, lose excess weight, avoid spicy or acidic foods, quit smoking, and elevate the head while sleeping.
-
Medications: Antacids, proton pump inhibitors (PPIs), and H2 blockers can reduce acid production and alleviate reflux symptoms.
-
Avoiding heavy lifting or straining: Reduces abdominal pressure and prevents hernia enlargement.
Surgical Treatment - Hiatal Hernia Repair:
When symptoms persist or the hernia is large or paraesophageal, surgery is recommended.
Goals of Surgery:
-
Reposition the stomach back into the abdomen.
-
Tighten or close the enlarged opening in the diaphragm.
-
Strengthen the lower esophageal sphincter to prevent reflux.
Common Surgical Techniques:
-
Laparoscopic Hiatal Hernia Repair:
The most common method. Small incisions are made, and specialized instruments repair the hernia with minimal scarring and quick recovery. -
Open Hiatal Hernia Repair:
Used in very large or complex hernias. Involves a larger incision and longer recovery period. -
Fundoplication (Nissen or Partial):
Often combined with repair. The upper part of the stomach (fundus) is wrapped around the lower esophagus to reinforce the valve and prevent reflux. -
Robotic-Assisted Repair:
Offers precise control, smaller incisions, and reduced postoperative discomfort.
Postoperative Recovery:
Patients usually stay in the hospital for one to two days. They begin with
liquid diets, gradually advancing to soft and then normal foods over several
weeks. Pain control, gentle activity, and avoiding heavy lifting are essential
for successful healing.
Prevention and Management Before and After Hiatal Hernia Repair
Before Surgery:
-
Optimize overall health by maintaining a balanced diet and healthy weight.
-
Stop smoking and manage chronic cough or constipation.
-
Discuss medications (especially blood thinners) with the surgeon.
-
Follow preoperative fasting instructions carefully.
After Surgery:
-
Dietary care: Begin with clear liquids, progress to soft foods, and slowly reintroduce solid foods. Eat smaller, frequent meals. Avoid carbonated drinks and foods that cause gas.
-
Physical activity: Walk regularly but avoid strenuous activity or heavy lifting for several weeks.
-
Wound care: Keep incision sites clean and dry to prevent infection.
-
Follow-up appointments: Essential to monitor healing and ensure no recurrence.
Long-Term Prevention:
Even after successful repair, adopting healthy habits is vital to prevent recurrence:
-
Maintain a healthy weight.
-
Eat slowly and chew thoroughly.
-
Avoid tight clothing that compresses the abdomen.
-
Manage reflux symptoms promptly.
-
Stay active and maintain strong core muscles through moderate exercise.
Complications of Hiatal Hernia Repair
While modern hiatal hernia repair is very safe, like any surgery, it carries potential risks and complications. Understanding these helps patients make informed decisions.
Possible Short-Term Complications:
-
Bleeding or infection at incision sites.
-
Injury to nearby organs (esophagus, stomach, or spleen).
-
Temporary difficulty swallowing (dysphagia).
-
Gas-bloat syndrome - inability to burp or vomit, causing discomfort.
-
Reaction to anesthesia.
Long-Term Complications:
-
Recurrence of the hernia if the diaphragm weakens again.
-
Persistent reflux or swallowing difficulties if the wrap is too tight or loosens.
-
Scar tissue formation leading to narrowing of the esophagus.
-
Mesh-related issues if reinforcement mesh was used.
Proper surgical technique, postoperative care, and adherence to recovery guidelines minimize these risks. Most patients experience complete relief from symptoms and rarely encounter major issues.
Living After Hiatal Hernia Repair
Recovery from hiatal hernia repair typically takes several weeks, but most patients report a significant improvement in their quality of life. Once healed, they often enjoy eating comfortably again and experience relief from reflux, heartburn, and chest discomfort.
Postoperative Lifestyle Tips:
-
Diet: Eat small, frequent meals and avoid overeating. Stay upright for at least 30-45 minutes after eating.
-
Activity: Gentle walking promotes recovery and reduces blood clot risk. Avoid lifting heavy objects or bending sharply.
-
Hydration: Drink plenty of fluids, but avoid carbonated drinks.
-
Sleep: Elevate the head of the bed to prevent reflux at night.
-
Follow-up: Attend all check-ups with your surgeon and inform them of any recurring symptoms like chest pain, difficulty swallowing, or reflux.
With modern surgical techniques and proper lifestyle modifications, patients who undergo hiatal hernia repair can lead a normal, active, and pain-free life. The surgery not only corrects the hernia but also resolves chronic reflux, prevents complications, and greatly enhances overall well-being.
Top 10 Frequently Asked Questions about Hiatal Hernia Repair
1. What is a Hiatal Hernia?
A hiatal hernia occurs when part of the stomach pushes upward through
the diaphragm - the muscle that separates the chest cavity from the
abdomen - into the chest area.
Normally, the esophagus passes through a small opening in the diaphragm called the
hiatus, and connects to the stomach. When this opening enlarges or
weakens, part of the stomach can bulge upward, creating a hiatal hernia.
There are two main types:
-
Sliding hiatal hernia - the most common type, where the stomach and lower esophagus slide up into the chest.
-
Paraesophageal hiatal hernia - less common but more serious, where part of the stomach pushes through beside the esophagus and can become trapped.
2. What is Hiatal Hernia Repair Surgery?
Hiatal hernia repair is a surgical procedure performed to reposition the stomach into the abdomen and close or tighten the enlarged opening (hiatus) in the diaphragm.
The surgery often includes a fundoplication, in which the upper part of the stomach (the fundus) is wrapped around the lower esophagus to prevent acid reflux.
This procedure is recommended when:
-
Symptoms of acid reflux (GERD) persist despite medications.
-
The hernia is large or at risk of strangulation.
-
There are breathing problems, chest pain, or swallowing difficulties due to the hernia.
3. What Are the Symptoms That Indicate the Need for Hiatal Hernia Repair?
Common symptoms of a hiatal hernia that may require surgery include:
-
Frequent heartburn or acid reflux
-
Regurgitation of food or sour liquid
-
Chest pain or discomfort after eating
-
Difficulty swallowing
-
Chronic cough, hoarseness, or sore throat
-
Shortness of breath (if the hernia compresses the lungs)
If these symptoms persist despite medication and lifestyle changes, surgery is often the best option to correct the problem permanently.
4. How is Hiatal Hernia Repair Surgery Performed?
Hiatal hernia repair can be performed using either open surgery or minimally invasive laparoscopic surgery.
1. Laparoscopic (Minimally Invasive) Surgery:
-
The surgeon makes a few small incisions in the abdomen.
-
A tiny camera (laparoscope) and instruments are used to pull the stomach back into place.
-
The diaphragm opening is tightened, and fundoplication may be done to prevent acid reflux.
-
Patients experience less pain, faster recovery, and smaller scars.
2. Open Surgery:
-
A larger incision is made in the chest or abdomen.
-
Usually performed for large or complex hernias, or when laparoscopic repair isn't suitable.
Most patients are candidates for laparoscopic repair, which is now the gold standard for hiatal hernia surgery.
5. How Long Does Hiatal Hernia Repair Surgery Take?
The procedure usually takes about 1 to 2 hours, depending on the size
and type of hernia and whether additional procedures (like fundoplication) are
performed.
Laparoscopic surgery generally requires less operating time and results
in faster recovery compared to open surgery.
6. What Are the Benefits of Hiatal Hernia Repair Surgery?
Hiatal hernia repair offers several important health benefits:
-
Long-term relief from acid reflux and heartburn.
-
Improved digestion and ability to swallow.
-
Reduced risk of strangulation or obstruction.
-
Better breathing and less chest pressure.
-
Improved quality of life without dependence on reflux medications.
Most patients experience significant symptom improvement within a few days after surgery.
7. What Are the Risks or Complications of Hiatal Hernia Repair?
Hiatal hernia repair is considered safe, but like any surgery, it carries some risks, including:
-
Bleeding or infection at the incision site
-
Injury to nearby organs such as the esophagus or stomach
-
Temporary difficulty swallowing (dysphagia)
-
Gas bloating or inability to burp
-
Recurrence of hernia (rare with modern techniques)
Choosing an experienced gastrointestinal or laparoscopic surgeon greatly reduces these risks.
8. What is the Recovery Time After Hiatal Hernia Repair?
Recovery time varies based on the surgical approach and individual health:
-
Laparoscopic repair: Most patients go home within 24-48 hours and return to normal activities in 2-3 weeks.
-
Open surgery: Hospital stay may last 3-5 days, with full recovery in 4-6 weeks.
During recovery, patients should:
-
Eat small, soft meals for the first few weeks.
-
Avoid heavy lifting or strenuous exercise.
-
Elevate the head while sleeping to prevent reflux.
-
Follow all post-surgery dietary and lifestyle recommendations.
9. What Lifestyle Changes Are Needed After Hiatal Hernia Repair?
After surgery, maintaining a healthy lifestyle helps prevent recurrence and supports healing. Recommended changes include:
-
Eat smaller meals and avoid lying down immediately after eating.
-
Avoid trigger foods like spicy, fried, or acidic items.
-
Maintain a healthy weight to reduce abdominal pressure.
-
Quit smoking and limit alcohol consumption.
-
Exercise regularly (after doctor approval).
-
Avoid tight clothing around the waist.
Following these guidelines ensures long-term success of the surgery and minimizes reflux symptoms.
10. What is the Success Rate and Long-Term Outlook After Hiatal Hernia Repair?
Hiatal hernia repair has a high success rate, especially with laparoscopic techniques.
-
Over 90% of patients experience significant and lasting relief from symptoms.
-
Recurrence rates are low when lifestyle and dietary recommendations are followed.
-
Most patients can discontinue long-term use of acid reflux medications after surgery.
With proper post-operative care, patients can expect permanent relief and a greatly improved quality of life.


