Introduction to Hip Arthroscopy
The human hip is one of the largest and most stable joints in the body, built to support body weight, allow mobility, and sustain the stresses of daily life and physical activity. It functions as a ball-and-socket joint, where the head of the femur (thigh bone) fits perfectly into the acetabulum (hip socket) of the pelvis. Both the femoral head and the acetabulum are lined with smooth cartilage that allows painless, fluid motion. However, when injuries, deformities, or wear affect the cartilage, labrum (the ring of cartilage that surrounds the socket), or surrounding structures, pain and restricted motion often occur.
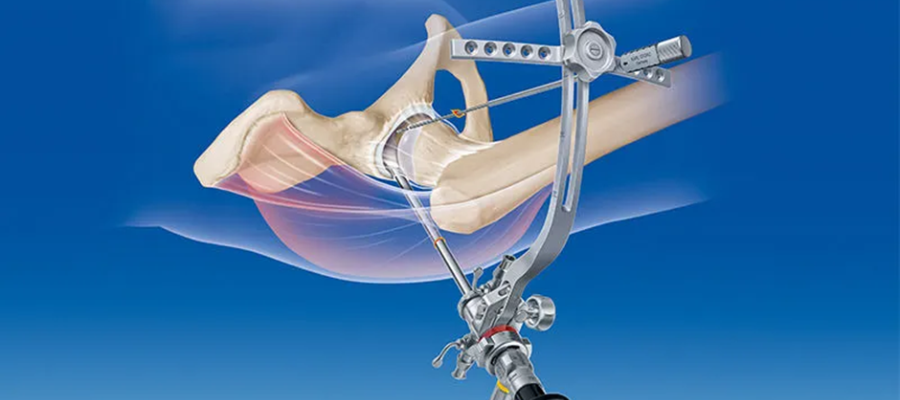
Hip arthroscopy is a minimally invasive surgical procedure designed to diagnose and treat various disorders inside the hip joint. Unlike open hip surgery, which requires large incisions, hip arthroscopy is performed through small keyhole cuts. A tiny camera (arthroscope) is inserted into the hip joint, allowing the surgeon to view internal structures on a video monitor. Fine surgical instruments are then used to repair or remove damaged tissues.
Hip arthroscopy is commonly performed to treat labral tears, femoroacetabular impingement (FAI), cartilage injuries, loose bodies, and synovial inflammation. This procedure has revolutionized the management of hip joint disorders because it minimizes tissue damage, reduces postoperative pain, and allows faster recovery. It is particularly valuable for young and active patients who wish to preserve their natural hip joint and avoid early arthritis or hip replacement.
Causes and Risk Factors Leading to Hip Arthroscopy
Hip arthroscopy is not performed for every hip problem but is specifically indicated for structural or soft-tissue abnormalities inside the joint. The causes that often lead to hip arthroscopy can be broadly categorized into injury-related, degenerative, and anatomical causes.
1. Femoroacetabular Impingement (FAI):
This is one of the most common conditions treated with hip arthroscopy. FAI occurs when the ball and socket of the hip do not fit together properly, leading to friction during movement. Over time, this friction damages the cartilage and labrum. There are two main types - cam impingement (extra bone growth on the femoral head) and pincer impingement (extra bone on the acetabular rim).
2. Labral Tears:
The labrum is a ring of cartilage that cushions the hip socket and provides stability. Injuries, repetitive twisting, or structural abnormalities can cause it to tear. Labral tears often result in deep groin pain, clicking, or catching sensations in the hip.
Cartilage Damage or Arthritis:
Excessive wear and tear due to sports injuries, aging, or trauma can damage the cartilage covering the bones, leading to pain and stiffness. Arthroscopy allows surgeons to remove loose fragments or perform cartilage repair techniques to delay further joint degeneration.
4. Loose Bodies and Synovitis:
Small bone or cartilage fragments (loose bodies) may float inside the joint, causing locking or catching. Synovitis - inflammation of the hip's lining - can also cause persistent pain and swelling. Arthroscopy can remove loose bodies and inflamed tissue.
Risk Factors:
-
High-impact sports (football, hockey, dance, martial arts).
-
Repetitive hip flexion or rotation.
-
Prior hip injuries or surgeries.
-
Congenital deformities such as hip dysplasia.
-
Obesity or sedentary lifestyle increasing mechanical stress.
-
Genetic predisposition to bone shape abnormalities.
Identifying and addressing these underlying causes early can prevent progression to severe cartilage damage and arthritis, which might later require total hip replacement.
Symptoms and Signs of Hip Problems Leading to Arthroscopy
Patients who eventually undergo hip arthroscopy usually present with persistent hip pain that interferes with daily activities. The symptoms can be subtle at first but gradually worsen over time, especially with movement.
Common Symptoms Include:
-
Groin or Anterior Hip Pain: Most patients feel discomfort deep in the groin area, which may radiate to the thigh or knee. Pain typically worsens with prolonged sitting, climbing stairs, or athletic activities.
-
Catching, Clicking, or Locking Sensation: These mechanical symptoms occur when a torn labrum or loose body interferes with smooth hip movement.
-
Stiffness or Restricted Range of Motion: Difficulty bending, rotating, or flexing the hip joint.
-
Pain During Sports or Exercise: Especially in sports requiring twisting or pivoting movements.
-
Hip Instability: A feeling that the hip might give way or slip during activity.
Physical Signs:
On examination, patients often have reduced hip flexion and internal rotation. Specific clinical tests such as the FADIR (flexion, adduction, internal rotation) and FABER (flexion, abduction, external rotation) may reproduce pain, suggesting intra-articular pathology.
Chronic pain that does not respond to medication, physiotherapy, or rest - especially when accompanied by mechanical symptoms - often points to structural damage inside the joint that may benefit from hip arthroscopy.
Diagnosis of Hip Disorders
The diagnosis of hip problems suitable for arthroscopy is made through a combination of clinical evaluation and imaging studies.
1. Medical History and Physical Examination:
A detailed history of symptoms, previous injuries, and activity levels helps determine the possible cause. The doctor will evaluate hip range of motion, stability, and pain triggers.
2. Imaging Tests:
-
X-rays: The first-line investigation to assess bone structure, joint space, and signs of impingement or arthritis.
-
MRI or MR Arthrogram: Provides detailed images of soft tissues, helping detect labral tears, cartilage injury, or inflammation.
-
CT Scan: Used for detailed bone mapping, especially in complex deformities like FAI.
-
Diagnostic Hip Injection: Sometimes an anesthetic is injected into the hip joint - if pain relief follows, it confirms the hip joint as the pain source.
Diagnosis and Decision for Surgery:
Once non-surgical treatments fail, and imaging confirms a correctable structural problem (such as labral tear or impingement), hip arthroscopy becomes the best treatment option. The surgeon will evaluate factors such as patient age, cartilage condition, and overall hip health before recommending surgery.
Treatment Options - Hip Arthroscopy and Its Procedures
Treatment of hip conditions starts with conservative management, including physical therapy, anti-inflammatory medications, and lifestyle adjustments. However, when these fail, hip arthroscopy offers an effective, minimally invasive surgical option.
Hip Arthroscopy Procedure:
The procedure is performed under general or spinal anesthesia. The surgeon makes two to three small incisions (portals) around the hip. A slender camera (arthroscope) and surgical instruments are inserted to visualize the joint interior. The procedure is performed under traction, gently pulling the leg to create space within the joint.
Common Procedures Performed During Hip Arthroscopy:
-
Labral Repair or Debridement: Torn labrum is either sutured back to the bone or trimmed if irreparable.
-
Femoroplasty and Acetabuloplasty: Bone reshaping to correct cam or pincer deformities in FAI.
-
Cartilage Repair: Techniques like microfracture stimulate cartilage healing.
-
Removal of Loose Bodies: Eliminates floating fragments that cause locking or catching.
-
Synovectomy: Removal of inflamed synovial tissue.
-
Capsular Tightening: For patients with hip instability.
Advantages of Hip Arthroscopy:
-
Smaller incisions and minimal tissue damage.
-
Less postoperative pain and faster recovery.
-
Lower risk of infection compared to open surgery.
-
Early return to work and sports.
Postoperatively, patients usually begin walking with crutches within a few days. Rehabilitation is essential to regain motion, strength, and stability.
Prevention and Management Before and After Hip Arthroscopy
Before Surgery:
Patients are advised to maintain an optimal weight, manage chronic health issues (like diabetes), and stop smoking to enhance healing. Preoperative physiotherapy (“prehab”) helps strengthen hip and core muscles, making postoperative recovery smoother.
After Surgery:
Postoperative care focuses on healing, regaining mobility, and protecting the repair.
-
Pain Control: Medications and cold therapy reduce discomfort.
-
Weight Bearing: Limited initially, then gradually increased as per surgeon's instructions.
-
Physical Therapy: Begins within days of surgery, progressing from gentle movements to strengthening and balance exercises.
-
Lifestyle Modifications: Avoid squatting, heavy lifting, and high-impact sports during early recovery.
-
Follow-Up: Regular assessments ensure proper healing and monitor for complications.
Long-term management includes maintaining flexibility, avoiding repetitive hip strain, and continuing strengthening exercises. Proper rehabilitation ensures a stable and pain-free hip joint with improved performance.
Complications of Hip Arthroscopy
Although hip arthroscopy is generally safe, potential complications can occur, as with any surgical procedure.
Common Complications Include:
-
Nerve Injury: Temporary numbness or tingling in the thigh due to traction used during surgery.
-
Infection or Bleeding: Rare due to minimally invasive technique.
-
Hip Stiffness or Persistent Pain: Often related to scar tissue or incomplete recovery.
-
Cartilage or Labral Re-tear: May occur if postoperative precautions are not followed.
-
Deep Vein Thrombosis (DVT): Blood clot formation, preventable with early mobility and medication.
-
Heterotopic Ossification: Abnormal bone formation in soft tissue, rare but manageable.
-
Conversion to Hip Replacement: In advanced arthritis or persistent symptoms, some patients may eventually need hip replacement surgery.
Proper surgical technique, patient selection, and adherence to rehabilitation protocols minimize the chances of complications.
Living After Hip Arthroscopy
Life after hip arthroscopy is typically active and pain-free for most patients. Recovery timelines vary depending on the type of repair and the individual's physical condition, but noticeable improvement is often seen within weeks.
Recovery Milestones:
-
First 1-2 weeks: Crutches for support, pain well controlled.
-
3-6 weeks: Begin weight-bearing and light physical therapy.
-
6-12 weeks: Improved range of motion, normal daily activities resumed.
-
3-6 months: Return to sports and higher-impact activities.
Lifestyle Guidance:
-
Maintain a healthy body weight to reduce hip stress.
-
Continue regular stretching and strengthening exercises.
-
Avoid repetitive hip strain or extreme range movements.
-
Follow the physiotherapist's advice for long-term joint protection.
Patients who undergo hip arthroscopy generally report significant pain relief, better flexibility, and improved quality of life. Most return to sports, work, and active lifestyles with full function restored.
Top 10 Frequently Asked Questions about Hip Arthroscopy
1. What is Hip Arthroscopy?
Hip arthroscopy is a minimally invasive surgical procedure used to diagnose and treat problems inside the hip joint. During the surgery, a small camera called an arthroscope is inserted into the hip through tiny incisions, allowing the surgeon to view the joint on a screen and use specialized instruments to repair damaged tissue.
This procedure is often recommended when non-surgical treatments such as physical therapy or medications fail to relieve hip pain or mobility issues.
2. When is Hip Arthroscopy Needed?
Hip arthroscopy is commonly performed to treat a variety of hip joint conditions, including:
-
Femoroacetabular impingement (FAI): Abnormal bone growth causing hip joint friction.
-
Labral tear: Damage to the cartilage (labrum) that cushions the hip socket.
-
Loose fragments: Removal of bone or cartilage pieces inside the joint.
-
Hip dysplasia: Structural abnormalities in the hip socket.
-
Snapping hip syndrome: When tendons or muscles snap over the hip bone.
-
Inflammation or synovitis: Irritation of the joint lining.
It's often chosen for young, active adults or athletes who experience pain without severe arthritis.
3. How is Hip Arthroscopy Performed?
The procedure is usually performed under general or regional anesthesia and takes about 1 to 2 hours.
Here's what happens during the surgery:
-
Small incisions are made around the hip joint.
-
A thin arthroscope (camera) is inserted to visualize the joint on a monitor.
-
Specialized instruments are used to remove damaged tissue, repair tears, or reshape bone.
-
The incisions are closed with stitches or surgical strips.
Since it's minimally invasive, it causes less tissue damage, less pain, and faster recovery compared to traditional open surgery.
4. What Are the Benefits of Hip Arthroscopy?
Hip arthroscopy offers numerous advantages, including:
-
Minimally invasive approach with smaller incisions.
-
Faster recovery and shorter hospital stay.
-
Reduced pain and scarring.
-
Improved hip function and mobility.
-
Accurate diagnosis of joint problems.
-
Early return to normal activities or sports.
It helps delay or prevent the need for more invasive procedures, such as hip replacement, in younger patients.
5. What Are the Risks or Complications of Hip Arthroscopy?
While hip arthroscopy is considered safe, some risks may occur, as with any surgery. These include:
-
Bleeding or infection.
-
Temporary numbness or tingling (due to traction on the leg).
-
Blood clots (rare).
-
Hip stiffness or swelling.
-
Incomplete pain relief or recurrence of symptoms.
-
Nerve or vessel injury (extremely rare).
An experienced orthopedic surgeon minimizes these risks and ensures the best possible outcome.
6. What is the Recovery Time After Hip Arthroscopy?
Recovery time varies depending on the condition treated and the patient's overall health.
In general:
-
Hospital stay: Usually outpatient or 1 day.
-
Walking: With crutches for 1-2 weeks post-surgery.
-
Physical therapy: Begins within a few days to restore strength and mobility.
-
Return to normal activities: 4-6 weeks for mild cases.
-
Return to sports or strenuous work: 3-6 months, depending on healing.
Following your surgeon's and physiotherapist's rehabilitation plan is crucial for a full and lasting recovery.
7. Is Hip Arthroscopy Painful?
Patients don't feel pain during the surgery because it's done under anesthesia. Afterward, mild discomfort or stiffness around the hip joint is common but well managed with pain-relieving medications, ice therapy, and physical therapy.
Most patients report less post-operative pain and faster recovery compared to traditional hip surgeries.
8. What Should I Expect After Hip Arthroscopy?
After surgery, you can expect:
-
Mild swelling or bruising around the incision site.
-
Restricted movement initially, followed by gradual improvement.
-
Use of crutches or a walker for a short period.
-
Physical therapy sessions to regain motion and strength.
-
Follow-up visits for wound inspection and progress monitoring.
Your surgeon will provide specific post-operative instructions on wound care, medications, and activity restrictions.
9. How Successful is Hip Arthroscopy?
Hip arthroscopy has a success rate of 85-95%, depending on the condition being treated and patient compliance with rehabilitation.
It effectively relieves pain, restores movement, and allows most patients to return to their daily activities and sports. However, patients with advanced arthritis or severe joint damage may require additional treatment or hip replacement later on.
10. How Can I Prepare for Hip Arthroscopy?
Before surgery, your surgeon will perform a thorough evaluation, including imaging tests such as MRI or X-rays, to identify the exact cause of hip pain.
To prepare:
-
Avoid eating or drinking as instructed before surgery.
-
Stop blood-thinning medications if advised.
-
Arrange for someone to drive you home after surgery.
-
Set up your recovery area at home with comfortable seating and easy access to essentials.
Discuss all medications, allergies, and medical conditions with your healthcare team prior to the procedure.


