Introduction to Hydrocele
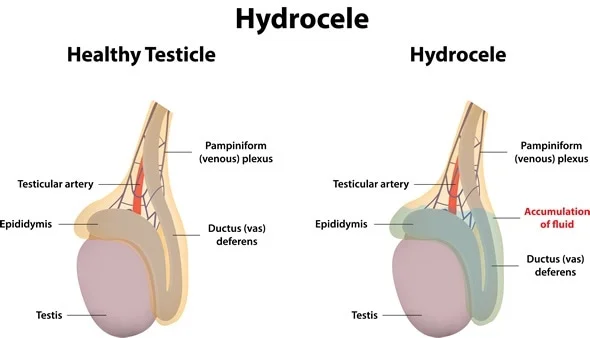
A hydrocele is a common medical condition characterized by the accumulation of fluid in the sac surrounding the testicle, leading to swelling in the scrotum. This fluid builds up within the tunica vaginalis - a thin membrane that encloses each testicle - and results in a soft, often painless enlargement that may affect one or both sides of the scrotum. Hydroceles can occur in newborns, infants, or adults and are typically benign, though in some cases they may be a sign of underlying testicular disease.
In infants, hydroceles are usually congenital, meaning they develop before birth due to the incomplete closure of a channel between the abdomen and scrotum known as the processus vaginalis. This allows fluid from the abdomen to flow into the scrotal sac. In adults, hydroceles are generally acquired, developing secondary to inflammation, trauma, infection, or conditions that disrupt fluid balance within the scrotum.
While many hydroceles cause no serious harm, large or symptomatic ones can cause discomfort, a feeling of heaviness, or embarrassment. In most cases, the condition is harmless and can resolve on its own, especially in infants. However, persistent or very large hydroceles often require medical attention or surgical intervention known as hydrocelectomy. Advances in urological surgery have made treatment simpler and highly effective, ensuring a complete cure and preventing recurrence.
Causes and Risk Factors of Hydrocele
Hydroceles develop when there is an imbalance between the production and absorption of the fluid surrounding the testicle. This imbalance can result from either congenital developmental issues or secondary causes in adults. Understanding these causes is crucial for effective management and prevention.
Congenital Hydrocele
In newborn boys, the testicles descend from the abdomen into the scrotum through a tunnel known as the processus vaginalis. Normally, this tunnel closes after birth, but when it remains partially open, fluid from the abdomen can pass into the scrotum, forming a congenital hydrocele. This type is common in newborns and premature babies and usually resolves spontaneously within the first year of life as the connection closes naturally.
Acquired Hydrocele
In adults, hydroceles are often the result of:
-
Injury or Trauma: A blow or strain to the scrotum can cause fluid accumulation as a protective response.
-
Infection or Inflammation: Infections such as epididymitis (inflammation of the epididymis) or orchitis (inflammation of the testicle) can cause fluid buildup.
-
Post-surgical Effects: Hydroceles sometimes occur after surgeries in the groin region, such as hernia repair.
-
Obstruction of Lymphatic Drainage: Conditions like filariasis (parasitic infection common in tropical areas) can block lymphatic vessels, leading to massive hydrocele formation.
-
Tumors or Testicular Disorders: Rarely, hydroceles may form secondary to testicular tumors or other growths within the scrotum.
Risk Factors
-
Premature birth (in infants).
-
Scrotal trauma or previous surgery.
-
Infection or inflammation of reproductive organs.
-
Chronic conditions affecting lymphatic circulation.
-
Living in regions where filarial infection is common.
Hydroceles can occur at any age, but adult males over 40 years are more prone to developing them, often as a result of other underlying scrotal pathologies.
Symptoms and Signs of Hydrocele
The primary sign of a hydrocele is painless scrotal swelling. The swelling typically increases gradually and can vary in size throughout the day. While most hydroceles are not painful, large ones may cause discomfort due to their size and weight.
Common Symptoms Include:
-
Scrotal Swelling: Usually smooth and soft to touch, affecting one or both sides.
-
Heaviness or Discomfort: A feeling of fullness in the scrotum, particularly when standing or walking for long periods.
-
Change in Size: The swelling may appear smaller in the morning and enlarge later in the day.
-
Mild Pain or Pressure: May occur in larger hydroceles or when inflammation coexists.
-
Cosmetic Concerns: The enlarged scrotum can be distressing or embarrassing for some patients.
Physical Signs:
Upon examination, a hydrocele typically appears as a fluid-filled, non-tender swelling in the scrotum. The testicle may be difficult to feel through the fluid. A key diagnostic feature is transillumination - when a light is shone through the scrotum, the hydrocele glows with a translucent appearance, confirming the presence of fluid.
If the swelling is firm, irregular, or associated with severe pain, it may indicate other conditions such as hernia, varicocele, or tumor, and further evaluation is required.
Diagnosis of Hydrocele
A correct diagnosis is essential to differentiate a hydrocele from other causes of scrotal enlargement, such as hernias or tumors.
Diagnostic Steps:
-
Medical History and Physical Examination:
The doctor will ask about the duration of swelling, presence of pain, history of trauma, infections, or surgery. During the exam, transillumination helps identify fluid in the scrotum. -
Ultrasound Scan:
A scrotal ultrasound is the most reliable test to confirm the diagnosis. It distinguishes hydrocele from hernias, varicoceles, and testicular tumors. It also shows whether the hydrocele is simple or complex (with septations, thickened walls, or debris). -
Additional Tests:
-
Urine and Blood Tests: To detect infection or inflammation.
-
Testing for Filariasis: In endemic regions, a blood test may identify the parasite responsible.
-
Differential Diagnosis:
Conditions that mimic hydrocele include:
-
Inguinal Hernia: Soft swelling that may reduce when lying down.
-
Varicocele: Dilated veins, described as a “bag of worms.”
-
Testicular Tumor: Solid, non-transilluminating mass, often painless.
-
Epididymal Cyst: Small, separate swelling near the testicle.
An accurate diagnosis ensures appropriate management and avoids unnecessary anxiety or delay in treating serious underlying causes.
Treatment Options for Hydrocele
Treatment depends on the cause, size, and symptoms of the hydrocele, as well as the patient's age.
Observation and Conservative Management:
-
In newborns and infants, hydroceles often resolve naturally within 12-24 months without any intervention.
-
Adults with small, asymptomatic hydroceles may be monitored regularly if no underlying disease is present.
Surgical Treatment:
Surgery is the definitive treatment for hydroceles that are large, symptomatic, or recurrent. The main surgical procedure is hydrocelectomy.
Hydrocelectomy Procedure:
-
Performed under local or general anesthesia.
-
A small incision is made in the scrotum or lower abdomen.
-
The fluid is drained, and the sac lining is either excised or everted to prevent recurrence.
-
Stitches are placed, and a dressing or scrotal support is applied postoperatively.
Hydrocelectomy is a quick, safe procedure, often completed within 30-60 minutes. Most patients can return home the same day.
Aspiration and Sclerotherapy:
For patients who cannot undergo surgery (elderly or medically unfit), aspiration (fluid removal with a needle) may provide temporary relief. To prevent recurrence, a sclerosing agent can be injected to seal the sac. However, this method carries a higher recurrence risk compared to surgery.
Postoperative Care:
-
Mild pain and swelling may persist for a few days.
-
Wearing a scrotal support helps reduce swelling.
-
Avoid strenuous activity for 2-3 weeks.
-
Follow-up visits ensure proper healing and detect any recurrence early.
Prevention and Management of Hydrocele
Although not all hydroceles can be prevented, certain measures can reduce the risk of developing or worsening the condition.
Preventive Measures:
-
Protect the Scrotum: Avoid trauma or prolonged pressure on the scrotal area.
-
Prompt Treatment of Infections: Managing testicular or epididymal infections early prevents inflammation that can cause fluid accumulation.
-
Avoid Heavy Lifting or Straining: This prevents excessive pressure buildup in the groin.
-
Manage Filarial Infections: In endemic regions, preventive medications and mosquito control are important.
Post-treatment Management:
-
Maintain proper hygiene and wear loose, supportive clothing.
-
Attend follow-up appointments to ensure the hydrocele does not return.
-
Engage in regular physical activity but avoid direct scrotal impact.
-
Monitor for recurrence, pain, or redness, and seek medical review if any changes occur.
Early medical evaluation remains key to preventing complications and ensuring timely treatment.
Complications of Hydrocele
Hydroceles are generally harmless, but if left untreated or if associated with other conditions, they can lead to complications.
Untreated Hydrocele Complications:
-
Infection: Fluid buildup may become infected, leading to pain, redness, and fever.
-
Pressure Effects: Large hydroceles can cause discomfort, difficulty walking, or pain during sexual activity.
-
Testicular Atrophy: Chronic pressure from large hydroceles can reduce blood supply to the testicle, leading to shrinkage.
-
Masking Serious Conditions: Hydroceles can obscure underlying tumors or hernias, delaying their diagnosis.
Post-surgical Complications (Rare):
-
Bleeding or hematoma formation in the scrotum.
-
Wound infection or inflammation.
-
Temporary swelling or discomfort.
-
Recurrence of hydrocele (rare with proper surgery).
-
Very rarely, injury to nearby structures like the epididymis.
With modern surgical techniques, the risk of major complications is minimal, and most patients recover fully within a few weeks.
Living with the Condition of Hydrocele
Most patients with hydrocele lead normal, healthy lives both before and after treatment. For those who undergo surgery, recovery is typically smooth, and long-term outcomes are excellent.
Post-surgical Lifestyle:
-
Rest for a few days and gradually resume normal activities.
-
Avoid driving or heavy lifting for at least two weeks.
-
Maintain scrotal support for comfort and to minimize swelling.
-
Continue gentle exercises once cleared by the doctor to promote circulation.
-
Maintain regular medical checkups to monitor for recurrence.
Emotional and Social Impact:
Hydrocele can sometimes cause embarrassment or anxiety due to scrotal swelling, especially in younger men. It is important to understand that this condition is common, treatable, and not linked to infertility or sexual dysfunction.
Prognosis:
With appropriate treatment, the prognosis for hydrocele is excellent. Recurrence is rare, and the majority of patients regain full function and comfort after surgery. Infants usually outgrow the condition naturally without any lasting effects.
Top 10 Frequently Asked Questions about Hydrocele
1. What is a Hydrocele?
A hydrocele is a fluid-filled sac that forms around a testicle, causing swelling in the scrotum. It is usually painless and non-cancerous. Hydroceles are common in newborns but can also occur in adult men, often due to injury, infection, or inflammation within the scrotum.
While most hydroceles are harmless, persistent swelling or discomfort may require medical evaluation to rule out other conditions like hernias or tumors.
2. What Causes a Hydrocele?
The causes of hydrocele differ depending on age:
In infants:
-
It occurs when the tunnel (processus vaginalis) between the abdomen and scrotum fails to close completely before birth, allowing fluid to collect around the testicle.
-
This is called a congenital hydrocele.
In adults:
-
May develop due to injury or inflammation within the scrotum.
-
Infection of the testicle (orchitis) or epididymis (epididymitis).
-
Blockage of lymphatic drainage leading to fluid buildup.
-
Occasionally linked to inguinal hernias.
Most adult hydroceles are secondary, meaning they occur due to an underlying condition rather than being present from birth.
3. What Are the Common Symptoms of a Hydrocele?
Typical symptoms include:
-
Swelling in one or both sides of the scrotum.
-
Heaviness or discomfort in the scrotal area.
-
A smooth, soft lump that may feel like a water balloon.
-
In some cases, pain or pressure if the hydrocele is large.
Hydroceles are usually painless, but significant swelling can cause difficulty sitting, walking, or wearing tight clothing.
4. How is a Hydrocele Diagnosed?
Doctors typically diagnose a hydrocele through a physical examination and simple diagnostic tests such as:
-
Transillumination: Shining a light through the scrotum to confirm fluid presence.
-
Ultrasound scan: To rule out hernia, tumor, or other causes of swelling.
-
Blood or urine tests: If infection is suspected.
Diagnosis is quick and non-invasive, allowing your doctor to determine whether treatment is necessary.
5. Can a Hydrocele Go Away on Its Own?
In infants, most hydroceles disappear naturally within the first 12 to 18 months of life as the fluid is reabsorbed by the body.
In adults, hydroceles typically do not resolve on their
own and may increase in size over time.
Persistent or large hydroceles often require surgical treatment to
prevent complications or discomfort.
6. What Are the Treatment Options for a Hydrocele?
Treatment depends on the size, cause, and symptoms:
1. Observation:
-
Small, painless hydroceles may simply be monitored if they don't cause discomfort.
2. Aspiration:
-
The fluid is drained using a needle.
-
This is a temporary solution, as the hydrocele often recurs.
3. Hydrocelectomy (Surgical Removal):
-
A minor surgical procedure to remove the hydrocele sac and prevent recurrence.
-
Usually performed under local or general anesthesia.
-
It provides a permanent cure in most cases.
Your doctor will recommend the most appropriate approach based on your age and condition.
7. What is a Hydrocelectomy and How is it Performed?
A hydrocelectomy is the definitive surgical treatment for hydrocele.
During the procedure:
-
A small incision is made in the scrotum or groin.
-
The fluid is drained, and the hydrocele sac is removed or turned inside out to prevent fluid accumulation.
-
The incision is closed with absorbable stitches.
It usually takes 30-45 minutes, and patients can return home the
same day or the next day.
Recovery is quick, with minimal post-operative pain and swelling.
8. What is the Recovery Time After Hydrocele Surgery?
Most patients recover fully within 1-2 weeks after surgery.
Post-surgery care includes:
-
Wearing supportive underwear (scrotal support).
-
Keeping the area clean and dry.
-
Avoiding heavy lifting, strenuous exercise, or sexual activity for at least 2-3 weeks.
-
Using painkillers or ice packs to reduce discomfort and swelling.
Mild swelling or bruising is common but usually subsides within a few days.
9. Are There Any Complications of Untreated Hydrocele?
While hydroceles are usually harmless, untreated cases can lead to:
-
Increased swelling causing discomfort or mobility issues.
-
Pressure on nearby structures, leading to testicular damage.
-
Infection or inflammation (rare).
-
Difficulty detecting other testicular problems like tumors or hernias.
For adults, persistent hydroceles should be medically evaluated to rule out underlying causes.
10. Can a Hydrocele Come Back After Surgery?
Recurrence after surgery is rare, especially when performed by an
experienced surgeon.
However, hydroceles can occasionally reappear if:
-
The original cause (like infection or trauma) persists.
-
Incomplete removal of the hydrocele sac.
Following post-operative instructions and attending follow-up appointments significantly reduces the risk of recurrence.


