Introduction to Hysteroscopy
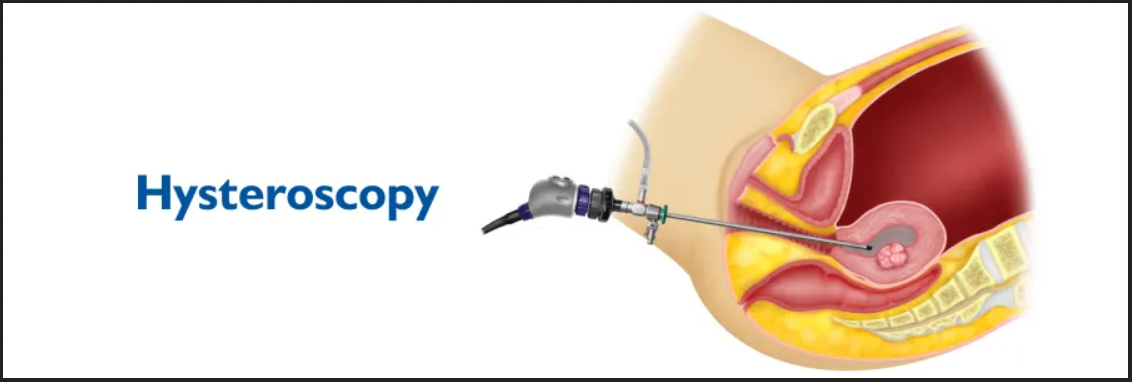
Hysteroscopy is a minimally invasive diagnostic and therapeutic procedure that allows a doctor to directly view the inside of the uterus (womb) using a specialized instrument known as a hysteroscope - a thin, lighted tube inserted through the vagina and cervix. This technique provides real-time visualization of the uterine cavity without the need for major incisions or open surgery, making it a preferred method in modern gynecology for both evaluation and treatment of various uterine conditions.
Hysteroscopy serves two primary purposes:
-
Diagnostic hysteroscopy, which helps identify abnormalities within the uterine cavity such as polyps, fibroids, septum, or causes of abnormal bleeding or infertility.
-
Operative hysteroscopy, which allows simultaneous treatment of these abnormalities by inserting miniature surgical instruments through the hysteroscope.
This procedure has revolutionized women's health management by offering a safe, accurate, and quick method for diagnosing uterine issues, eliminating the need for exploratory surgeries like laparotomy in many cases. It is commonly performed on an outpatient basis and allows women to return home the same day, often with minimal discomfort.
In today's medical practice, hysteroscopy plays a vital role in diagnosing abnormal uterine bleeding, recurrent miscarriages, uterine scarring, congenital malformations, and infertility-related concerns. It is often paired with imaging techniques like ultrasound or laparoscopy for comprehensive reproductive evaluation.
With advancements in fiber-optic imaging and endoscopic technology, hysteroscopy has become a cornerstone in gynecologic care - enabling precision, safety, and improved fertility outcomes.
Causes and Risk Factors of Hysteroscopy
While hysteroscopy is a procedure rather than a disease, it is performed to investigate or treat underlying causes of uterine or reproductive abnormalities. Understanding these causes helps identify the medical necessity of the procedure.
A. Common Conditions Requiring Hysteroscopy
-
Abnormal Uterine Bleeding (AUB):
Heavy, prolonged, or irregular menstrual bleeding, or bleeding after menopause. -
Uterine Polyps or Fibroids:
Benign growths that can distort the uterine cavity, cause pain, or interfere with fertility. -
Recurrent Miscarriages:
When structural abnormalities like uterine septum or adhesions are suspected. -
Infertility Evaluation:
To assess the uterine cavity for hidden defects that might prevent implantation. -
Retained Products of Conception:
After miscarriage or delivery, retained tissue can cause infection or bleeding. -
Endometrial Abnormalities:
Investigation of thickened endometrium, hyperplasia, or suspected malignancy. -
Intrauterine Adhesions (Asherman's Syndrome):
Scar tissue inside the uterus that causes menstrual irregularities or infertility. -
Foreign Body Removal:
Such as intrauterine devices (IUDs) that have become embedded or misplaced.
B. Risk Factors for Needing Hysteroscopy
Certain women are more likely to require hysteroscopy due to:
-
Age: Women over 40, or approaching menopause, are more prone to uterine bleeding issues.
-
Hormonal Imbalances: Caused by polycystic ovarian syndrome (PCOS) or thyroid disorders.
-
Previous Pelvic Surgery: May increase the likelihood of uterine scarring or adhesions.
-
Reproductive Challenges: Such as repeated miscarriages or failed IVF cycles.
-
Obesity or Diabetes: Contributing to hormonal and endometrial dysfunctions.
While hysteroscopy is safe for most women, certain health conditions - like pelvic infection, cervical cancer, or pregnancy - may pose higher risks and are contraindications for the procedure.
Symptoms and Signs Indicating the Need for Hysteroscopy
Hysteroscopy is recommended when a woman experiences symptoms that suggest uterine cavity abnormalities, or when other diagnostic tests fail to provide clarity.
Common Symptoms Include:
-
Abnormal Vaginal Bleeding:
-
Heavy periods (menorrhagia)
-
Prolonged bleeding between cycles (metrorrhagia)
-
Bleeding after menopause
-
Spotting between periods or after intercourse
-
-
Pelvic Pain or Pressure:
Persistent cramping, heaviness, or pain during menstruation can signal fibroids or polyps. -
Infertility or Repeated Pregnancy Loss:
Structural uterine problems such as septum or adhesions may prevent successful implantation. -
Unexplained Vaginal Discharge:
Sometimes due to retained tissue or infection within the uterus. -
Failure to Conceive Despite Treatment:
Hysteroscopy is often used as part of fertility evaluation before assisted reproductive techniques (IVF or IUI). -
Detection of Uterine Abnormalities on Ultrasound:
For example, when imaging reveals endometrial thickening or an abnormal growth, hysteroscopy helps confirm and treat the condition directly.
These signs help gynecologists determine whether hysteroscopy is necessary for accurate diagnosis and management.
Diagnosis and Evaluation Before Hysteroscopy
Before performing hysteroscopy, a complete clinical assessment and diagnostic workup are essential to ensure suitability and safety. This preparation ensures that any underlying conditions are identified and that the patient is fully informed.
A. Preoperative Assessment
-
Medical History Review:
Includes menstrual cycle patterns, previous surgeries, pregnancies, and allergies. -
Physical and Pelvic Examination:
Evaluates for infections, cervical abnormalities, or anatomical issues. -
Ultrasound Scan:
Transvaginal or pelvic ultrasound provides preliminary insight into uterine structure and identifies polyps, fibroids, or abnormal tissue. -
Blood Tests:
Complete blood count, coagulation profile, and sometimes hormonal levels to evaluate bleeding risk.
B. Diagnostic Imaging
-
Sonohysterography (Saline Infusion Ultrasound):
Uses sterile saline and ultrasound for initial visualization of uterine cavity. -
MRI (Magnetic Resonance Imaging):
Occasionally used when fibroids or complex uterine malformations are suspected.
C. Indications for Diagnostic vs. Operative Hysteroscopy
-
Diagnostic hysteroscopy is performed purely for visualization and assessment.
-
Operative hysteroscopy is performed to correct the identified abnormalities simultaneously, reducing the need for repeat procedures.
This dual purpose - diagnosis and treatment - makes hysteroscopy a cornerstone of modern gynecological practice.
Treatment Procedure: Hysteroscopy
The hysteroscopy procedure is a minimally invasive technique that allows a doctor to look inside the uterus using a thin, lighted telescope called a hysteroscope. It is performed for both diagnostic and operative (treatment) reasons, such as investigating abnormal bleeding, removing polyps or fibroids, and assessing infertility.
A. How the Procedure is Performed
-
Anesthesia:
Depending on the complexity, it may be done under local, regional, or general anesthesia. -
Insertion of the Hysteroscope:
The hysteroscope, a slender telescope-like device, is gently inserted through the vagina and cervix into the uterus. -
Distention of Uterine Cavity:
Sterile saline or carbon dioxide gas is introduced to expand the uterine cavity for better visualization. -
Examination and Intervention:
The camera transmits real-time images to a monitor, allowing the doctor to inspect the uterine walls. If polyps, fibroids, or scar tissue are found, miniature instruments are inserted through the hysteroscope to remove or correct them. -
Duration:
Diagnostic procedures typically take 10-20 minutes, while operative hysteroscopy can last up to 45-60 minutes. -
Recovery:
The patient is observed for a short time post-surgery and can usually return home the same day.
B. Common Procedures Performed During Hysteroscopy
-
Polypectomy: Removal of uterine polyps.
-
Myomectomy: Resection of small submucosal fibroids.
-
Adhesiolysis: Breaking up intrauterine scar tissue (Asherman's syndrome).
-
Septum Resection: Correcting congenital uterine septum to improve fertility.
-
Endometrial Ablation: Destroying endometrial lining to control heavy bleeding.
-
Biopsy: Sampling of uterine tissue for histopathological examination.
Prevention and Management of Post-Hysteroscopy Recovery
Prevention and management of post-hysteroscopy recovery focus on minimizing complications, managing common symptoms, and supporting rapid return to normal life. Most people recover quickly, but some self-care practices and awareness of warning signs are important.
A. Preventive Measures Before Surgery
-
Treat any pre-existing vaginal or urinary infections.
-
Avoid sexual intercourse, douching, or tampon use 48 hours prior.
-
Stop blood-thinning medications (as advised by the doctor).
-
Eat light meals the day before and fast if general anesthesia is planned.
B. Postoperative Management
After hysteroscopy, most women experience mild cramping, spotting, or watery discharge for 24-48 hours - which is completely normal. Recovery guidelines include:
-
Rest for at least one day; avoid strenuous exercise for 48 hours.
-
Avoid vaginal intercourse and tampon use for 1-2 weeks to reduce infection risk.
-
Drink plenty of fluids and maintain good personal hygiene.
-
Take prescribed antibiotics and pain relief medications as advised.
-
Attend follow-up visits to assess healing and discuss findings or results.
Most women can resume daily activities within 1-2 days and experience complete recovery in a week.
Complications of Hysteroscopy
Although hysteroscopy is a safe and routine procedure, potential risks - while rare - should be understood and monitored.
A. Minor Complications
-
Mild Pain or Cramping: Common and short-lived.
-
Spotting or Light Bleeding: Normal for a few days post-surgery.
-
Nausea or Dizziness: Often due to anesthesia, resolves quickly.
B. Serious but Rare Complications
-
Uterine Perforation:
Accidental puncture of the uterine wall, usually healing spontaneously. -
Infection:
Pelvic or uterine infections can occur if aseptic techniques are not maintained. -
Bleeding:
Excessive bleeding may occur during fibroid removal or ablation. -
Fluid Overload:
When too much distention fluid is absorbed, leading to electrolyte imbalance. -
Adhesion Formation:
Postoperative scar tissue can rarely form, leading to menstrual changes.
When performed by experienced surgeons with modern techniques, complication rates are extremely low (<1%), and patient outcomes are excellent.
Living with the Condition After Hysteroscopy
Hysteroscopy often brings immense relief and improved quality of life, particularly for women who have struggled with heavy bleeding, pain, or infertility.
A. Physical Recovery and Lifestyle
-
Most women return to work and routine activities within 2-3 days.
-
Regular menstruation typically resumes within 4-6 weeks.
-
Fertility outcomes are highly favorable after treatment of uterine abnormalities.
-
Maintain healthy habits - hydration, balanced diet, and stress management - to aid healing.
B. Emotional and Reproductive Benefits
-
Relief from anxiety and distress caused by chronic bleeding or infertility.
-
Increased chances of conception following correction of polyps, fibroids, or adhesions.
-
Restored confidence and emotional well-being as symptoms improve.
C. Long-Term Prognosis
Hysteroscopy provides both immediate and long-term therapeutic benefits. Once underlying issues are resolved, most women enjoy normal menstrual cycles and improved reproductive outcomes for years. Regular follow-up and gynecological screenings ensure lasting health and prevent recurrence of problems.
Top 10 Frequently Asked Questions about Hysteroscopy
1. What is Hysteroscopy?
Hysteroscopy is a minimally invasive diagnostic and surgical
procedure used to examine the inside of the uterus (womb).
It involves inserting a thin, lighted tube called a hysteroscope
through the vagina and cervix into the uterus. This allows the doctor to view
the uterine cavity and detect or treat abnormalities, such
as fibroids, polyps, adhesions, or abnormal bleeding.
Hysteroscopy can be performed for diagnostic or
operative purposes.
2. Why is a Hysteroscopy performed?
Hysteroscopy may be recommended for several gynecological reasons, including:
-
Abnormal uterine bleeding (heavy, prolonged, or irregular periods)
-
Postmenopausal bleeding
-
Fibroids or polyps inside the uterus
-
Infertility evaluation or repeated miscarriages
-
Removal of intrauterine adhesions (scar tissue)
-
Retrieval of an IUD or foreign body from the uterus
-
Examination of uterine abnormalities seen on ultrasound
It helps diagnose problems accurately and sometimes treat them in the same session.
3. What are the types of Hysteroscopy?
There are two main types:
-
Diagnostic Hysteroscopy: Used to inspect the uterine cavity and identify issues causing symptoms.
-
Operative Hysteroscopy: Used to treat or remove abnormalities, such as polyps, fibroids, or adhesions.
Both types can be performed using the same hysteroscope, but operative hysteroscopy may require special instruments and anesthesia.
4. How is Hysteroscopy performed?
The procedure is typically performed in a hospital or outpatient clinic:
-
The patient lies on an exam table similar to a pelvic exam position.
-
A hysteroscope (thin telescope-like device) is inserted through the vagina and cervix into the uterus.
-
A harmless liquid or gas is gently introduced to expand the uterus for better visibility.
-
The doctor examines the uterine cavity and, if necessary, removes abnormal tissue.
It usually takes 10-30 minutes, depending on whether it's diagnostic or operative.
5. Is Hysteroscopy painful?
-
Diagnostic hysteroscopy can be slightly uncomfortable but is often performed under local anesthesia or mild sedation.
-
Operative hysteroscopy is usually done under general or regional anesthesia to ensure no pain.
Patients may experience mild cramping or spotting afterward, which typically resolves within a few days.
Most women return to normal activities within 24-48 hours.
6. What are the benefits of Hysteroscopy?
Hysteroscopy offers several advantages, including:
-
Accurate diagnosis of uterine problems
-
Simultaneous treatment during the same procedure
-
No external incisions (performed through natural openings)
-
Short recovery time
-
Less pain and bleeding compared to open surgery
-
Faster return to normal routine
It's a safe and highly effective method for diagnosing and treating intrauterine conditions.
7. What are the risks or complications of Hysteroscopy?
Hysteroscopy is generally safe, but rare complications may include:
-
Infection
-
Uterine perforation (small tear in the wall of the uterus)
-
Bleeding
-
Damage to the cervix or nearby organs
-
Allergic reaction to anesthesia or distension fluid
Your doctor will discuss these risks before the procedure, and choosing an experienced gynecologist minimizes complications.
8. How should I prepare for a Hysteroscopy?
Preparation includes:
-
Scheduling the procedure after your period but before ovulation for best visibility.
-
Avoiding intercourse, douching, or tampon use for 24 hours before the procedure.
-
Informing your doctor about any medications or allergies.
-
You may be asked to fast for a few hours before surgery (if anesthesia is used).
-
Arrange for someone to accompany you if sedation or anesthesia will be administered.
Your doctor will provide specific pre-procedure instructions tailored to your needs.
9. What should I expect after a Hysteroscopy?
After the procedure:
-
Mild cramping, light bleeding, or watery discharge for a day or two is normal.
-
You can usually go home the same day.
-
Avoid sexual intercourse, swimming, or tampon use for at least 1-2 weeks.
-
You can return to work or daily activities within a day or two (unless advised otherwise).
-
Contact your doctor if you experience heavy bleeding, severe pain, fever, or foul discharge.
Full recovery is typically quick, especially after diagnostic hysteroscopy.
10. How successful is Hysteroscopy?
Hysteroscopy has a high success rate for both diagnosis and treatment:
-
It can accurately identify the cause of abnormal bleeding or infertility.
-
Operative hysteroscopy can treat most uterine problems immediately and effectively.
-
Studies show it significantly improves fertility outcomes for women with uterine abnormalities.
When performed by an experienced gynecologist, hysteroscopy is one of the most effective and low-risk procedures in modern gynecology.


