Introduction to Insertion of IUCD
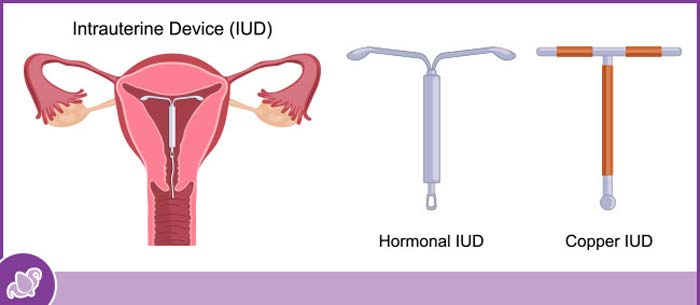
The intrauterine contraceptive device (IUCD) is a small, typically T-shaped device placed inside the uterus to provide long-acting, reversible contraception. The insertion of an IUCD is a common procedure in gynecological practice that offers women a low-maintenance, highly effective birth control option. Modern IUCDs can be either non-hormonal (such as copper-bearing devices) or hormonal (releasing progestin), and they may also serve additional purposes such as managing heavy menstrual bleeding or providing contraception immediately postpartum.
IUCD insertion involves placing the device through the cervical canal into the uterine cavity under sterile conditions. The aim is to position the device correctly at the uterine fundus so that it remains effective and causes minimal discomfort or complications. Because of its high effectiveness and convenience, the IUCD has become one of the most trusted methods of long-acting reversible contraception (LARC) worldwide.
In this article you will learn: what leads to IUCD insertion, the risks and suitability criteria, the clinical symptoms or scenarios prompting insertion, how the procedure is assessed and performed, the range of treatment options and device types, how to manage and minimise risks, what complications may occur, and how women live and adapt with an IUCD in place.
Causes and Risk Factors for IUCD Insertion
The main causes and risk factors for complications with IUCD (intrauterine contraceptive device) insertion center on infection risk, uterine perforation, expulsion, and potential pregnancy-related issues. Most serious complications are rare, but awareness of these risk factors is important for safe placement and continued use.
A. Causes or Reasons for IUCD Use
-
Long-Term Reversible Contraception:
Ideal for women who desire a long-term contraceptive option without the daily attention that pills or condoms require. -
Postpartum Family Planning:
IUCDs can be inserted immediately after childbirth (within 10 minutes to 48 hours post-delivery) or after 6 weeks, offering effective spacing between pregnancies. -
Non-Hormonal Contraception Preference:
Copper IUCDs are suitable for women who prefer to avoid hormonal contraception. -
Medical Indications:
Hormonal IUCDs can manage gynecological conditions like:-
Heavy menstrual bleeding (menorrhagia)
-
Endometrial hyperplasia
-
Adenomyosis
-
Endometriosis-related pain
-
-
Emergency Contraception:
When inserted within 5 days of unprotected sex, a copper IUCD is the most effective emergency contraceptive method available.
B. Risk Factors or Contraindications
IUCDs are safe for most women, but certain conditions may increase risks:
-
Active pelvic inflammatory disease (PID) or sexually transmitted infections (STIs)
-
Undiagnosed vaginal or uterine bleeding
-
Severe uterine distortion (e.g., due to fibroids or congenital anomalies)
-
Recent septic abortion or postpartum infection
-
Copper allergy or Wilson's disease (for copper IUCDs)
-
Current pregnancy or suspicion of pregnancy
A thorough pre-insertion screening ensures that IUCD placement is safe and appropriate for each individual.
Symptoms and Signs Related to IUCD
Symptoms and signs related to IUCD (intrauterine contraceptive device, or IUD) commonly involve changes in menstrual cycles, pelvic discomfort, and certain warning features that may indicate complications or device problems. The specific symptoms can differ depending on whether a hormonal or copper IUD is used.
A. Normal Symptoms After Insertion
-
Mild cramping or abdominal discomfort lasting a few hours to 1-2 days.
-
Light spotting or bleeding immediately after insertion.
-
Slight back pain due to uterine contractions.
-
Altered menstrual flow:
-
Copper IUCDs may increase bleeding or cramps during periods.
-
Hormonal IUCDs often cause lighter periods or even amenorrhea (absence of menstruation) over time.
-
B. Warning Signs (When to See a Doctor)
While uncommon, certain symptoms may indicate complications:
-
Severe pelvic pain or persistent cramps.
-
Heavy vaginal bleeding or foul-smelling discharge.
-
Fever or chills (possible infection).
-
Missing or shortened IUCD strings.
-
Signs of pregnancy or fainting spells.
Recognizing these early warning signs helps prevent more serious complications such as infection or device displacement.
Diagnosis and Evaluation Before IUCD Insertion
Diagnosis and evaluation before IUCD (IUD) insertion involve a comprehensive assessment to confirm that the patient is an appropriate candidate and to minimize the risk of complications such as infection, expulsion, or perforation. The process focuses on history, physical examination, screening for contraindications, and patient counseling.
A. Pre-Insertion Assessment
-
Detailed Medical and Sexual History:
To rule out infections, allergies, or contraindications. -
Physical and Pelvic Examination:
-
Assesses the size, shape, and position of the uterus.
-
Checks for pelvic tenderness or cervical infection.
-
-
Pregnancy Test:
Ensures that the woman is not pregnant at the time of insertion. -
Screening for STIs:
Tests for gonorrhea, chlamydia, or other infections to prevent post-insertion complications. -
Pap Smear (if indicated):
Helps identify cervical pathology before device insertion. -
Ultrasound (Optional):
Used in special cases to confirm uterine structure or to guide placement in women with anatomical challenges.
B. Timing of Insertion
-
During menstruation: The cervix is naturally softer and slightly open, making insertion easier and ensuring the patient is not pregnant.
-
Postpartum: Can be inserted immediately or after 6 weeks.
-
Post-abortion: Safely inserted once infection has been ruled out.
Proper diagnosis and preparation minimize complications and ensure optimal placement.
Treatment Options and IUCD Insertion Procedure
The main treatment option for people seeking long-term, reversible contraception is IUCD (intrauterine contraceptive device) insertion. This quick in-office procedure, performed by a trained healthcare provider, is highly effective for both copper and hormonal IUDs. The process uses sterile technique and careful steps to minimize discomfort and complications.
A. The IUCD Insertion Process
-
Preparation:
The patient lies in a lithotomy position (on the back, knees bent), and the vagina and cervix are cleaned with an antiseptic solution. -
Cervical Stabilization:
A speculum is used to visualize the cervix, which is gently held with a tenaculum for stabilization. -
Measurement:
The healthcare provider measures the uterine depth using a uterine sound to ensure correct IUCD placement. -
Insertion:
The IUCD, loaded into an inserter, is passed through the cervical canal into the uterine cavity. The arms of the device open into a T-shape, and the inserter is removed. -
String Trimming:
The attached threads are trimmed to 2-3 cm length, allowing future verification and removal.
The entire process takes about 5-10 minutes. Mild cramping is expected during and after insertion.
B. Post-Insertion Care
-
Rest for a few hours after the procedure.
-
Mild analgesics may be prescribed for cramping.
-
Avoid sexual intercourse and tampon use for 48-72 hours.
-
A follow-up visit after 4-6 weeks confirms correct placement through examination or ultrasound.
C. IUCD Removal
Removal is simple and quick - the provider gently pulls the strings using forceps, and the device slides out. Fertility returns immediately after removal.
Prevention and Management After IUCD Insertion
Prevention and management after IUCD (IUD) insertion focus on reducing the risk of infection, managing expected side effects, ensuring device retention, and recognizing warning signs requiring medical attention. Most patients can return to normal activities quickly, but careful self-care and monitoring in the first days and weeks are important.
A. Preventive Care
-
Practice safe sex to prevent pelvic infections.
-
Schedule regular checkups every 6-12 months.
-
Check IUCD strings monthly after menstruation to ensure proper position.
-
Maintain personal hygiene, especially during menstruation.
B. Management of Side Effects
-
Cramping: Managed with nonsteroidal anti-inflammatory drugs (NSAIDs).
-
Heavy Bleeding: Hormonal IUCDs or short-term medication can help regulate flow.
-
Infection: Prompt antibiotic therapy is necessary if symptoms arise.
-
Expulsion: If the IUCD partially comes out, it must be reinserted or replaced.
Proper management ensures the IUCD remains effective and comfortable for long-term use.
Complications of IUCD Insertion
IUCD (IUD) insertion is generally safe, but some complications can occur-most are rare, but awareness and prompt attention to warning signs are crucial. Complications may arise during the procedure, in the days to weeks following insertion, or later while the device is in place.
A. Immediate Complications
-
Pain and fainting: Due to vagal response during insertion.
-
Bleeding: Minor spotting is normal; excessive bleeding requires evaluation.
-
Perforation: Rarely, the IUCD may puncture the uterine wall during insertion.
B. Delayed Complications
-
Expulsion: Occurs in 2-10% of users, especially within the first 6 months.
-
Infection or PID: Often associated with pre-existing STIs.
-
Menstrual changes: Heavier or irregular bleeding with copper IUCD; lighter periods with hormonal IUCD.
-
Pregnancy or Ectopic Pregnancy: Extremely rare, but if pregnancy occurs, it may be ectopic.
Early detection and treatment prevent long-term issues and preserve fertility.
Living with the Condition of Insertion of IUCD
Living with an IUCD (intrauterine contraceptive device, IUD) is generally straightforward and convenient, offering long-term, highly effective birth control with minimal daily attention. Most people quickly adapt, though there are some adjustments and self-care tips to consider.
A. Adjusting to Life After Insertion
Most women adapt easily after the first month. Normal activities, including exercise, travel, and sexual intercourse, can be resumed once the doctor confirms proper positioning.
B. Fertility and Menstrual Patterns
-
Copper IUCDs may cause heavier periods initially but normalize over time.
-
Hormonal IUCDs often lead to lighter or absent menstruation after 6-12 months.
-
Fertility returns to normal immediately upon removal, making it an excellent reversible option.
C. Emotional and Lifestyle Benefits
-
No daily reminders or maintenance required.
-
Freedom from hormonal side effects (for copper IUCD users).
-
Reduced anxiety about unintended pregnancy.
-
Long-term cost-effectiveness compared to short-term contraceptives.
D. When to Consult a Doctor
-
You cannot feel the IUCD strings.
-
Severe pain, unusual discharge, or missed periods.
-
Desire for removal or switching to another contraceptive method.
Top 10 Frequently Asked Questions about Insertion of IUCD
1. What is an IUCD?
An IUCD (Intrauterine Contraceptive Device) is a small, T-shaped
device that is inserted into a woman's uterus to prevent
pregnancy.
It is a long-term, reversible, and highly effective method of
contraception that can last from 3 to 10 years, depending on the type
of IUCD used.
There are two main types of IUCDs:
-
Copper IUCD (e.g., Copper-T): Uses copper to prevent sperm from fertilizing the egg.
-
Hormonal IUCD (e.g., Mirena, Kyleena): Releases small amounts of progesterone to prevent ovulation and thicken cervical mucus.
Both types are safe and provide over 99% effectiveness in preventing pregnancy.
2. How Does an IUCD Work?
The IUCD works by creating an environment inside the uterus that prevents conception.
-
Copper IUCDs release copper ions, which are toxic to sperm and prevent fertilization.
-
Hormonal IUCDs release progestin, which thickens cervical mucus to block sperm, thins the uterine lining, and may stop ovulation.
If fertilization does occur, the IUCD prevents the implantation of the fertilized egg in the uterus, ensuring effective contraception.
3. Who Can Use an IUCD?
An IUCD is suitable for most women, including those who:
-
Want long-term, reversible birth control.
-
Have had at least one child (though it's also safe for women who haven't).
-
Cannot or do not wish to use hormonal pills or injections.
-
Are breastfeeding (especially copper IUCDs).
However, IUCDs may not be suitable for women with:
-
Active pelvic infections or sexually transmitted infections (STIs).
-
Unexplained vaginal bleeding.
-
Uterine abnormalities (fibroids or congenital issues).
A gynecologist will evaluate your health to determine if an IUCD is appropriate for you.
4. How is an IUCD Inserted?
The IUCD insertion procedure is simple and takes only a few minutes:
-
The doctor performs a pelvic examination to check the size and position of the uterus.
-
The IUCD is inserted through the cervix into the uterus using a sterile applicator.
-
The device's threads are trimmed so they slightly extend into the vaginal canal for easy future removal.
The procedure can cause mild discomfort or cramping for a few minutes, but anesthesia is generally not required.
Insertion can be done:
-
Right after childbirth (within 48 hours).
-
After 6 weeks postpartum.
-
Immediately after a miscarriage or abortion, if there is no infection.
5. How Effective is the IUCD in Preventing Pregnancy?
IUCDs are one of the most effective forms of reversible birth control, with a success rate of over 99%.
This means that fewer than 1 in 100 women using an IUCD will get
pregnant in a year.
Effectiveness does not depend on daily or monthly user action, making it a
low-maintenance and reliable contraception option.
6. What Are the Benefits of Using an IUCD?
Key benefits include:
-
Highly effective and long-lasting (3-10 years depending on type).
-
Reversible - fertility returns immediately after removal.
-
Low maintenance - no need to remember daily pills or monthly injections.
-
Safe for breastfeeding women.
-
Non-hormonal options (like Copper-T) available for those avoiding hormones.
-
May reduce menstrual pain and bleeding (with hormonal IUCDs).
IUCDs are cost-effective, discreet, and convenient for long-term family planning.
7. What Are the Side Effects or Risks of IUCD Insertion?
Some women may experience mild side effects after insertion, such as:
-
Cramping or back pain for a few days.
-
Irregular spotting or heavier periods (with copper IUCDs).
-
Lighter or shorter periods (with hormonal IUCDs).
-
Mild discomfort during sexual activity (rare).
Serious complications are rare but may include:
-
Expulsion (IUCD falling out).
-
Perforation of the uterine wall during insertion (extremely rare).
-
Infection if inserted in the presence of an untreated STI.
Most side effects subside within a few weeks as the body adjusts to the device.
8. What Should I Expect After IUCD Insertion?
After insertion:
-
You may experience mild cramps or spotting for a few days.
-
Normal activities can usually be resumed within 24 hours.
-
Avoid sexual intercourse or tampon use for 24-48 hours post-insertion to reduce infection risk.
-
The doctor will schedule a follow-up visit after 4-6 weeks to ensure the IUCD is properly positioned.
If you experience severe pain, heavy bleeding, or foul-smelling discharge, contact your doctor immediately.
9. How is the IUCD Removed or Replaced?
IUCD removal is a quick and simple procedure:
-
The doctor gently pulls on the IUCD's strings to remove it.
-
It usually takes less than a minute and causes only mild discomfort.
An IUCD can be replaced immediately with a new one if continued
contraception is desired.
You can also choose to have it removed at any time if you want to
conceive - fertility returns almost immediately after removal.
10. Is IUCD Insertion Painful or Dangerous?
Most women experience only mild cramping or pressure during IUCD
insertion, which lasts for a few seconds.
Doctors may offer pain relief or a local anesthetic if necessary.
The procedure is safe when performed by a qualified healthcare provider,
and serious complications are extremely rare.
For reassurance, your doctor will explain what to expect during and after the insertion.


