Introduction to Intraocular Lens Implant Surgery
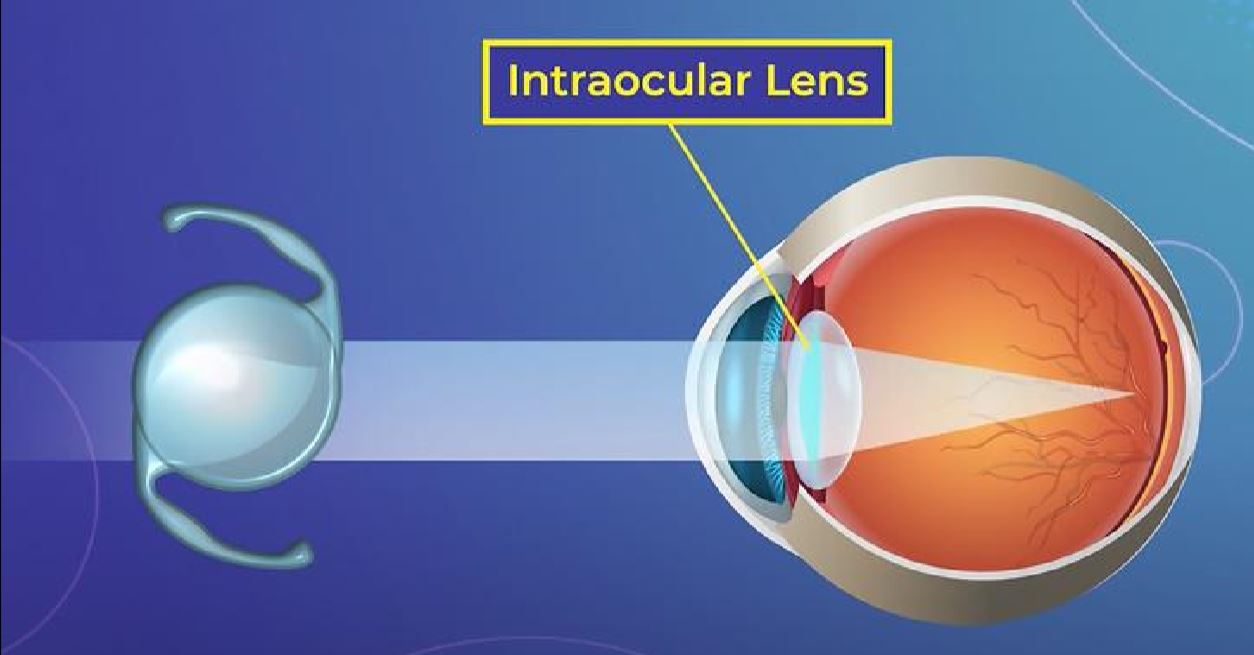
Intraocular Lens Implant Surgery (IOL Surgery) is a highly advanced and effective ophthalmic procedure designed to replace the eye's natural lens when it becomes clouded, damaged, or less effective due to age or disease. The artificial lens, called an intraocular lens (IOL), restores clear vision by focusing light correctly onto the retina, allowing patients to regain sharp, natural sight.
The surgery is most commonly performed as part of cataract removal-one of the world's most frequently performed and successful surgical procedures. During cataract surgery, the clouded natural lens is removed and replaced with a transparent artificial IOL. However, IOL implantation can also be used independently to correct severe refractive errors such as myopia (nearsightedness), hyperopia (farsightedness), and presbyopia, offering patients freedom from glasses or contact lenses.
Modern intraocular lenses are made from biocompatible materials such as acrylic, silicone, or polymethylmethacrylate (PMMA). These lenses are designed to last a lifetime, providing clarity and comfort without the need for maintenance. The surgery itself is minimally invasive, quick, and painless, usually performed under local anesthesia, with most patients returning home within hours.
With ongoing innovations such as multifocal, accommodating, and toric lenses, IOL surgery has evolved beyond just cataract correction - it now offers customized vision enhancement suited to each patient's lifestyle and visual needs. For millions worldwide, intraocular lens implantation is not just a medical procedure; it is the gateway to restored independence, confidence, and quality of life.
Causes and Risk Factors Leading to Intraocular Lens Implant Surgery
Intraocular lens implantation becomes necessary when the eye's natural lens loses its transparency or ability to focus light properly, leading to blurred vision, glare, or even blindness in advanced cases.
A. Common Causes
-
Cataracts:
The most frequent cause for IOL implantation. Cataracts occur when the natural lens becomes cloudy due to protein buildup, often linked to aging, diabetes, or UV exposure. -
Refractive Errors:
Patients with severe myopia, hyperopia, or presbyopia who are unsuitable for laser eye surgery (LASIK/PRK) can benefit from phakic IOLs (implanted without removing the natural lens). -
Lens Dislocation or Trauma:
Injuries or congenital conditions like Marfan syndrome can cause lens instability requiring replacement. -
Congenital Cataracts:
Present at birth and may necessitate early surgical intervention to prevent amblyopia (lazy eye). -
Post-Surgical or Drug-Induced Changes:
Previous ocular surgeries or long-term corticosteroid use can accelerate cataract formation.
B. Risk Factors
Certain factors increase the likelihood of developing conditions that may require intraocular lens implantation:
-
Age: Most cataract-related surgeries occur in individuals aged 55 and above.
-
Diabetes Mellitus: Causes faster progression of lens opacification.
-
Excessive Sunlight Exposure (UV rays).
-
Smoking and Alcohol Consumption.
-
Prolonged Corticosteroid Use.
-
Family History of Early-Onset Cataracts or Eye Disorders.
-
Ocular Trauma: Injury or foreign body damage to the lens.
Recognizing and managing these risks early can help delay lens degeneration and maintain visual clarity longer.
Symptoms and Signs Requiring Intraocular Lens Implant Surgery
The symptoms leading to intraocular lens implantation primarily result from clouding or dysfunction of the natural lens. Early recognition is vital to prevent vision deterioration.
A. Visual Symptoms
-
Blurry or Hazy Vision: The hallmark of cataracts or advanced refractive error.
-
Glare and Halos: Especially noticeable around lights at night, causing driving difficulties.
-
Double Vision (Diplopia): In one eye, caused by irregular lens opacity.
-
Fading or Yellowing of Colors: Colors appear dull and less vibrant.
-
Frequent Changes in Prescription: Repeatedly changing glasses without improvement.
-
Difficulty with Reading or Close Work: Caused by presbyopia or cataract-related visual distortion.
B. Functional Symptoms
-
Trouble performing daily activities such as reading, sewing, or driving.
-
Increased sensitivity to bright light or sunlight.
-
Poor night vision leading to anxiety or reduced mobility.
When these symptoms begin to interfere with quality of life, ophthalmologists may recommend intraocular lens implant surgery as a definitive solution.
Diagnosis Before Intraocular Lens Implant Surgery
A thorough ophthalmic evaluation is essential before deciding on IOL implantation. The process ensures the correct diagnosis and helps customize lens selection for optimal outcomes.
A. Diagnostic Tests and Examinations
-
Visual Acuity Test: Measures clarity of vision using an eye chart.
-
Slit Lamp Examination: Allows detailed inspection of the lens, cornea, and anterior chamber to detect cataracts or inflammation.
-
Retinal Examination (Ophthalmoscopy): Ensures the retina and optic nerve are healthy before surgery.
-
Tonometry: Measures intraocular pressure to rule out glaucoma.
-
Biometry (IOL Power Calculation): Uses ultrasound or laser devices to measure eye length and corneal curvature, helping select the most suitable lens power.
-
Corneal Topography: Maps the corneal surface to guide toric IOLs for patients with astigmatism.
-
Dilated Eye Examination: Evaluates the extent and type of cataract or other lens opacities.
B. Pre-Surgical Counseling
Patients receive personalized guidance regarding:
-
Types of IOLs available (monofocal, multifocal, toric, or accommodating).
-
Expected outcomes and limitations.
-
Postoperative care and recovery expectations.
This step ensures informed consent and realistic expectations prior to surgery.
Treatment Options: The Intraocular Lens Implant Surgery Procedure
The treatment for cataract or certain refractive conditions often involves intraocular lens (IOL) implant surgery, which replaces the eye's natural lens with a clear artificial lens. This is a precise, outpatient procedure usually performed under local anesthesia.
A. Overview of the Procedure
Intraocular lens implantation is usually performed as day surgery under local or topical anesthesia. The entire process takes 15 to 30 minutes per eye and involves minimal discomfort.
B. Step-by-Step Procedure
-
Anesthesia: Eye drops or local anesthesia are applied to numb the area.
-
Incision: A micro-incision (2-3 mm) is made in the cornea.
-
Lens Removal: Using a technique called phacoemulsification, the surgeon breaks the cloudy natural lens with ultrasonic waves and removes it.
-
IOL Implantation: The artificial intraocular lens, folded for insertion, is placed into the lens capsule. It unfolds and positions itself securely.
-
Closure: The incision is self-sealing and rarely requires stitches.
The patient is monitored for a short period before discharge, with protective eyewear provided.
C. Types of Intraocular Lenses
-
Monofocal IOLs:
Provide clear vision at one distance (usually far). Reading glasses may still be needed. -
Multifocal IOLs:
Correct both near and far vision, reducing dependence on glasses. -
Toric IOLs:
Specifically designed for patients with astigmatism. -
Accommodating IOLs:
Mimic natural lens movement, allowing focus at multiple distances. -
Phakic IOLs:
Implanted without removing the natural lens to correct high myopia or hyperopia.
Modern technology allows customization of lens selection based on the patient's age, occupation, and lifestyle.
Prevention and Management After Surgery
Prevention and management after intraocular lens (IOL) implant surgery-commonly done for cataract removal-involve infection prevention, careful activity restrictions, and symptom monitoring to ensure optimal healing and vision recovery.
A. Preventive Measures Before Surgery
-
Control underlying conditions like diabetes and hypertension.
-
Stop using contact lenses a few days before biometry testing.
-
Avoid eye makeup or creams on the day of surgery.
-
Discuss all medications with the surgeon to manage anticoagulants or other drugs.
B. Postoperative Management
-
Eye Protection: Wear protective sunglasses and avoid rubbing the eye.
-
Medications: Use antibiotic and anti-inflammatory eye drops as prescribed.
-
Activity Restrictions: Avoid heavy lifting, bending, or swimming for 2-3 weeks.
-
Follow-Up Visits: Regular eye exams ensure proper healing and IOL stability.
Most patients notice dramatic improvement in vision within 24-48 hours, though complete healing takes 4-6 weeks.
Complications of Intraocular Lens Implant Surgery
Although IOL surgery is among the safest procedures in modern medicine, potential complications-though rare-can occur.
A. Early Complications
-
Mild pain, redness, or irritation (resolves with medication).
-
Corneal edema (swelling).
-
Transient increase in intraocular pressure.
-
Infection (Endophthalmitis)-a serious but rare condition requiring immediate treatment.
B. Late Complications
-
Posterior Capsule Opacification (PCO):
A common “after-cataract” condition where residual lens cells cloud the capsule. Easily treated with YAG laser capsulotomy. -
Lens Dislocation:
Rarely, the IOL may shift position, requiring repositioning. -
Retinal Detachment:
Risk is slightly elevated in highly myopic patients. -
Glare and Halos:
May occur with multifocal lenses but usually decrease with time. -
Inflammation or Cystoid Macular Edema:
Controlled with anti-inflammatory eye drops.
With advancements in surgical techniques and sterile practices, serious complications are now exceedingly rare (less than 1-2%).
Living with the Results of Intraocular Lens Implant Surgery
Living with the results of intraocular lens (IOL) implant surgery-usually performed to treat cataracts or severe refractive errors-generally means dramatic improvement in vision, independence from glasses (depending on lens type), and enhanced quality of life. With proper care and periodic monitoring, the benefits are long-lasting and satisfaction rates are extremely high.
A. Recovery Experience
Most patients resume normal activities within a few days. Visual clarity improves rapidly, and dependency on corrective lenses is greatly reduced or eliminated, depending on the IOL type.
B. Lifestyle Benefits
-
Freedom from thick glasses or contact lenses.
-
Enhanced ability to drive, read, and perform daily tasks comfortably.
-
Improved color perception and depth of field.
-
Boosted confidence and independence.
C. Long-Term Care
-
Annual eye checkups to monitor IOL position and retinal health.
-
Protective eyewear to shield against UV damage.
-
Control of systemic diseases like diabetes to prevent ocular complications.
D. Emotional Well-Being
Restoration of vision profoundly impacts mental health - reducing anxiety, promoting independence, and improving overall quality of life.
Top 10 Frequently Asked Questions about Intraocular Lens (IOL) Implant Surgery
1. What is Intraocular Lens (IOL) Implant Surgery?
Intraocular Lens (IOL) Implant Surgery is a procedure in which a
permanent artificial lens is placed inside the eye to replace a
damaged or natural lens that has become cloudy or dysfunctional-most
commonly after cataract removal.
The artificial lens restores clear vision by focusing light properly
onto the retina.
IOL implantation can also be done as a refractive procedure to correct
vision problems like myopia (nearsightedness), hyperopia
(farsightedness), or presbyopia.
2. Why is an IOL Implant Surgery performed?
The surgery is primarily performed for:
-
Cataract treatment: After removal of a cloudy natural lens.
-
Vision correction: As an alternative to glasses, contact lenses, or LASIK surgery.
-
Refractive errors: To improve near, distance, or multifocal vision.
-
Lens replacement: In conditions like lens dislocation or trauma.
It helps patients regain sharp, clear, and bright vision, often reducing dependence on corrective eyewear.
3. What are the types of Intraocular Lenses (IOLs)?
There are several types of IOLs designed to meet different vision needs:
-
Monofocal IOLs: Provide clear vision at one distance (usually far); glasses may be needed for near work.
-
Multifocal IOLs: Offer clear vision at multiple distances - near, intermediate, and far.
-
Toric IOLs: Correct astigmatism and improve overall visual clarity.
-
Accommodating IOLs: Flex slightly within the eye to allow focusing at various distances.
-
Extended Depth of Focus (EDOF) IOLs: Provide a continuous range of vision with fewer visual disturbances.
Your ophthalmologist will help you choose the best IOL type based on your age, lifestyle, and visual needs.
4. How is the IOL Implant Surgery performed?
The surgery is typically an outpatient procedure that takes about
15-30 minutes per eye.
Steps include:
-
Local anesthesia or eye drops are given to numb the eye.
-
A small incision is made in the cornea.
-
The natural lens (usually affected by cataract) is gently removed using ultrasound (phacoemulsification).
-
The artificial intraocular lens is inserted into the same capsule that held the natural lens.
-
The incision is self-sealing - usually no stitches are required.
Patients can go home the same day and resume light activities shortly after.
5. Is IOL Implant Surgery painful?
No, the surgery is virtually painless.
-
Local or topical anesthesia is used to numb the eye completely.
-
You may feel slight pressure or movement, but no pain.
After the procedure, mild discomfort, itching, or watery eyes may occur for a day or two, which subsides quickly with prescribed medications.
6. What are the benefits of IOL Implant Surgery?
Key benefits include:
-
Restores clear and sharp vision after cataract removal.
-
Improves color perception and contrast sensitivity.
-
Reduces dependence on glasses or contact lenses.
-
Permanent solution - IOLs are designed to last a lifetime.
-
Quick recovery and minimal downtime.
-
Enhances overall quality of life with improved visual clarity.
Many patients experience significantly better vision within 24-48 hours after surgery.
7. What are the risks or complications of IOL Implant Surgery?
IOL implantation is highly safe, but like any surgical procedure, it may carry rare risks such as:
-
Infection or inflammation (endophthalmitis)
-
Glare or halos around lights (especially with multifocal lenses)
-
Posterior capsule opacification (PCO) - a common, treatable clouding of the lens capsule
-
Retinal detachment or swelling (rare)
-
Dislocation of the lens implant (rare and correctable)
These complications are rare and can be effectively managed by your ophthalmologist.
8. What is the recovery time after IOL Implant Surgery?
Recovery is usually fast and smooth:
-
First 24 hours: Mild discomfort and blurry vision are common.
-
Within 2-3 days: Most patients notice clear vision improvement.
-
Complete healing: Usually within 4-6 weeks.
Post-surgery care includes:
-
Using prescribed eye drops to prevent infection and inflammation.
-
Avoiding rubbing or pressing the eye.
-
Wearing protective glasses when outdoors.
-
Attending follow-up appointments for monitoring.
Patients can typically return to work within a few days.
9. How long do Intraocular Lenses last?
Intraocular lenses are designed to be permanent.
Unlike natural lenses, they do not age, degrade, or cloud over
time.
However, in some cases, a secondary issue called posterior capsule opacification
(PCO) may occur months or years later - easily treated with a
quick, painless laser procedure (YAG capsulotomy) to restore clear
vision.
10. Who is a good candidate for IOL Implant Surgery?
You may be an ideal candidate if you:
-
Have cataracts affecting your vision.
-
Want to reduce dependence on glasses or contact lenses.
-
Have healthy corneas and retina.
-
Have stable eye health with no active infection or inflammation.
-
Are seeking a long-term vision correction solution.
Your ophthalmologist will conduct a comprehensive eye examination and discuss your medical history to confirm suitability.


