Introduction to Laparoscopic Colposuspension
Laparoscopic colposuspension, often known as Burch colposuspension, is a minimally invasive surgical procedure used to treat stress urinary incontinence (SUI) - a condition in which urine leaks involuntarily during physical activities that increase abdominal pressure, such as coughing, laughing, sneezing, or exercising. The procedure aims to restore the normal anatomical position of the urethra and bladder neck by lifting and securing them to strong pelvic ligaments through a laparoscopic approach.
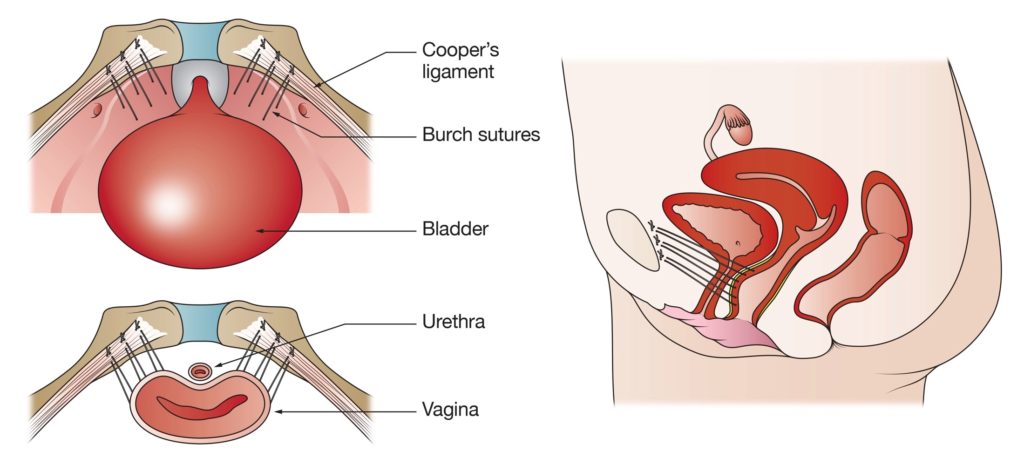
During this surgery, the surgeon uses small keyhole incisions to insert a laparoscope (a thin camera) and specialized instruments into the abdomen. The bladder neck and urethra are then lifted and sutured to the Cooper's ligament (part of the pelvic bone) or surrounding supportive tissue. This elevates and stabilizes the urethra, improving its ability to close properly under pressure.
Laparoscopic colposuspension evolved from the traditional open Burch colposuspension technique, offering the same effectiveness but with less postoperative pain, minimal scarring, shorter hospital stays, and faster recovery times. It is especially beneficial for women who wish to maintain normal bladder function and avoid synthetic mesh slings.
This procedure remains one of the gold standards for surgical correction of stress urinary incontinence, particularly for women who do not respond to conservative or non-surgical treatments.
Causes and Risk Factors Leading to Laparoscopic Colposuspension
The need for laparoscopic colposuspension arises from conditions that weaken the pelvic floor and the support structures around the bladder neck and urethra, leading to stress urinary incontinence (SUI).
Primary causes include:
-
Childbirth Trauma: Vaginal deliveries, particularly multiple or complicated ones, can stretch or damage the muscles and ligaments supporting the bladder and urethra.
-
Aging: As women age, estrogen levels decline, leading to tissue weakening and reduced elasticity of the pelvic floor.
-
Obesity: Increased abdominal pressure from excess body weight can chronically strain the bladder and its supporting structures.
-
Chronic Coughing or Straining: Conditions such as chronic bronchitis, asthma, or constipation repeatedly increase abdominal pressure, weakening pelvic supports over time.
-
Previous Pelvic Surgery: Procedures such as hysterectomy may disturb the pelvic floor architecture, predisposing to stress incontinence.
-
Connective Tissue Disorders: Some women have genetically weaker collagen or connective tissue, increasing the risk of pelvic floor dysfunction.
Risk Factors that Increase Likelihood of Surgery:
-
Persistent stress incontinence despite conservative measures such as pelvic floor exercises, lifestyle changes, and medication.
-
Physical occupations involving heavy lifting or straining.
-
Postmenopausal women due to hormonal changes.
-
Smoking (as it impairs blood flow and tissue healing).
-
Family history of pelvic floor weakness or urinary incontinence.
Understanding these causes and risk factors is vital, as early preventive strategies - such as strengthening pelvic muscles and maintaining a healthy weight - can delay or reduce the need for surgical intervention.
Symptoms and Signs of Stress Urinary Incontinence
Laparoscopic colposuspension is typically performed to address symptoms of stress urinary incontinence (SUI). Recognizing these symptoms early helps patients seek timely medical evaluation and appropriate treatment.
Common symptoms include:
-
Urine leakage during exertion: Loss of urine while coughing, sneezing, laughing, exercising, or lifting heavy objects.
-
Frequent minor leaks: Small but bothersome dribbles of urine that occur several times a day.
-
Reduced bladder control: Difficulty holding urine when changing positions or performing sudden movements.
-
Emotional distress: Embarrassment, social withdrawal, or avoidance of physical activity due to fear of leakage.
-
Hygiene and skin issues: Constant dampness leading to skin irritation or urinary odor.
Signs found on examination:
-
Evidence of pelvic floor laxity or prolapse (bladder, vaginal wall, or uterine descent).
-
Urethral hypermobility, where the urethra moves excessively when abdominal pressure increases.
-
Leakage observed during stress testing (asking the patient to cough or bear down).
-
Normal bladder capacity and sensation (distinguishing it from urge incontinence).
These symptoms and findings confirm stress urinary incontinence as the primary cause and help determine if surgical intervention, such as laparoscopic colposuspension, is warranted.
Diagnosis Before Laparoscopic Colposuspension
A precise diagnosis is essential to ensure that the patient's urinary incontinence results from urethral hypermobility or weakened pelvic supports rather than other causes, such as detrusor overactivity or neurological conditions.
Diagnostic evaluation includes:
-
Detailed Medical History: Understanding the onset, frequency, and severity of urine leakage, past childbirths, surgeries, and medical conditions.
-
Physical and Pelvic Examination: To assess pelvic muscle strength, presence of prolapse, and urethral movement during straining.
-
Urine Tests: To rule out urinary tract infection, which can mimic incontinence symptoms.
-
Urodynamic Studies: Measure bladder pressure, urine flow, and sphincter control to confirm the diagnosis of stress incontinence.
-
Post-Void Residual Measurement: Ensures the bladder empties completely after urination.
-
Cystoscopy (if needed): Allows visualization of the urethra and bladder to rule out structural abnormalities or previous surgical scarring.
Preoperative Assessment:
-
Overall medical fitness evaluation including cardiac and pulmonary function.
-
Review of current medications, allergies, and comorbidities.
-
Counseling about expectations, recovery, and potential complications.
Proper diagnosis ensures that laparoscopic colposuspension is appropriate and increases the likelihood of long-term success.
Treatment Options for Stress Urinary Incontinence
Treatment options for stress urinary incontinence (SUI) include a wide range of conservative, behavioral, medical, and surgical interventions. Most people start with non-surgical measures, but effective surgical options are available for those with persistent symptoms.
Conservative (Non-Surgical) Treatments:
Before surgery, many women benefit from less invasive treatments, including:
-
Pelvic Floor Muscle Training (Kegel Exercises): Strengthening the muscles that support the bladder and urethra can significantly reduce leakage.
-
Lifestyle Modifications: Weight loss, avoiding caffeine and alcohol, managing constipation, and quitting smoking.
-
Bladder Training: Scheduled voiding to improve bladder control.
-
Medication: Hormone replacement therapy (HRT) for postmenopausal women to improve tissue tone.
-
Pessary Devices: Supportive devices placed in the vagina to help reposition the bladder.
Surgical Options:
When conservative therapy fails, surgery offers a long-term solution.
-
Laparoscopic Colposuspension (Burch Procedure):
The surgeon lifts the bladder neck and sutures it to the Cooper's ligament using laparoscopic tools. This restores the natural support of the urethra, preventing leakage.Advantages include:
-
Small incisions and less tissue trauma.
-
Reduced pain and blood loss.
-
Shorter hospitalization (often 1-2 days).
-
Faster return to normal activities.
-
Excellent long-term success rates (70-90% symptom improvement).
-
-
Alternative Surgical Options:
-
Mid-urethral Sling Procedures: Synthetic or biological tape placed under the urethra for support.
-
Urethral Bulking Agents: Injection of material around the urethra to improve closure strength.
-
Open Colposuspension: Traditional method with larger incision, now less common due to longer recovery.
-
The choice of procedure depends on patient anatomy, previous surgeries, surgeon expertise, and patient preference.
Prevention and Management Before and After Surgery
Effective management before and after laparoscopic colposuspension is vital for optimal outcomes and prevention of recurrence.
Preoperative Preparation:
-
Stop smoking and limit alcohol intake several weeks before surgery.
-
Manage any infections or medical conditions.
-
Follow surgeon's instructions for fasting and medications.
-
Perform pelvic floor exercises to strengthen muscles before surgery.
Postoperative Care and Management:
-
Hospital Stay: Most patients are discharged within 24-48 hours.
-
Catheter Care: A urinary catheter may remain for a short time to allow healing.
-
Pain Control: Mild pain managed with oral analgesics.
-
Physical Activity: Avoid heavy lifting or vigorous activity for 4-6 weeks.
-
Diet: Maintain hydration and a fiber-rich diet to prevent constipation.
-
Follow-Up Visits: Regular checkups ensure proper healing and bladder function.
Long-Term Prevention:
-
Continue pelvic floor exercises even after surgery.
-
Maintain a healthy weight to avoid excessive pelvic pressure.
-
Treat chronic cough or constipation promptly.
-
Schedule periodic follow-ups to monitor pelvic floor health.
These measures help sustain surgical success and prevent recurrence of stress incontinence.
Complications of Laparoscopic Colposuspension
Although laparoscopic colposuspension is generally safe and effective, as with all surgical procedures, potential complications may occur.
Possible Complications:
-
Bleeding or Infection: Rare and minimized by laparoscopic techniques.
-
Injury to Surrounding Structures: Such as bladder, urethra, or blood vessels.
-
Voiding Difficulties: Temporary difficulty emptying the bladder due to increased urethral support.
-
Urge Incontinence: Some patients may develop a new urge to urinate frequently, known as mixed incontinence.
-
Mesh or Suture Complications: If synthetic materials are used, rare erosion or irritation may occur.
-
Recurrence of Stress Incontinence: Over time, tissues may relax again, requiring revision surgery.
Risk Factors for Complications:
-
Smoking, obesity, poor wound healing, and previous pelvic surgeries.
-
Chronic conditions like diabetes or connective tissue disorders.
Prevention and Management:
-
Skilled surgical technique and experienced hands reduce complications.
-
Early mobilization and infection control measures.
-
Monitoring for urinary retention or infection during recovery.
Most women recover without major complications and enjoy long-lasting improvement in continence and quality of life.
Living with the Condition Before and After Surgery
Living with the condition requiring lamellar keratoplasty is often marked by significant visual disability and functional impairment before surgery, contrasted with substantial improvement and greater quality of life after successful surgical intervention.
Before Surgery:
Living with stress urinary incontinence can be physically and emotionally exhausting. Women may experience embarrassment, reduced confidence, and social withdrawal due to fear of leakage. Activities like running, sneezing, or laughing can become sources of anxiety. Proper education, pelvic therapy, and supportive care can improve emotional well-being while preparing for surgery.
After Surgery:
Following laparoscopic colposuspension, most women notice a dramatic improvement in continence. Recovery is faster compared to open surgery, with minimal discomfort and scarring. Patients are encouraged to resume light activities within a week and normal routines after 4-6 weeks.
Long-Term Lifestyle Adjustments:
-
Maintain regular pelvic floor exercises.
-
Keep a healthy diet and active lifestyle.
-
Avoid heavy lifting or chronic straining.
-
Stay hydrated and treat respiratory issues that cause coughing.
-
Seek prompt medical advice if new urinary symptoms appear.
Quality of Life:
Most women experience improved confidence, restored independence, and the freedom to engage in physical and social activities without fear. Emotional and psychological well-being also significantly improve following successful surgery.
Top 10 Frequently Asked Questions about Laparoscopic Colposuspension
1. What is Laparoscopic Colposuspension?
Laparoscopic colposuspension is a minimally invasive surgical procedure used to treat stress urinary incontinence in women. It involves lifting and supporting the bladder neck and urethra by attaching supportive tissues to ligaments near the pelvis, restoring normal bladder positioning. This procedure is done using small abdominal incisions and a laparoscope, which reduces pain, scarring, and recovery time compared to traditional open surgery.
2. Who is a candidate for this procedure?
Laparoscopic colposuspension is usually recommended for women who:
-
Experience stress urinary incontinence, which is urine leakage during activities such as coughing, sneezing, or exercise.
-
Have not achieved satisfactory results with non-surgical treatments, such as pelvic floor exercises, medications, or lifestyle modifications.
-
Are medically fit for general anesthesia and laparoscopic surgery.
It is most commonly performed in women whose urinary incontinence is due to bladder neck or urethral mobility issues.
3. How is the surgery performed?
-
The patient is under general anesthesia.
-
Several small incisions are made in the lower abdomen for the laparoscope and instruments.
-
The bladder neck and urethra are exposed, and sutures are placed to lift and secure the bladder neck to the pelvic ligaments.
-
The laparoscopic instruments allow precise placement of sutures with minimal tissue trauma.
-
Incisions are closed and recovery begins, often with minimal scarring.
The entire procedure typically takes 1-2 hours, depending on individual anatomy and complexity.
4. What are the benefits of laparoscopic colposuspension?
-
Minimally invasive: Smaller incisions mean less pain, reduced infection risk, and better cosmetic results.
-
High success rate: Many women achieve significant improvement or complete resolution of stress urinary incontinence.
-
Shorter recovery: Hospital stays are typically shorter than traditional open colposuspension, often 1-2 days.
-
Preserves pelvic anatomy: Laparoscopic techniques allow precise adjustment without extensive disruption of surrounding tissues.
-
Durable results: The procedure can provide long-term support to the bladder neck.
5. What are the risks or complications?
Although generally safe, possible complications include:
-
Infection at incision sites or internally.
-
Bleeding during or after surgery.
-
Urinary retention or difficulty emptying the bladder, which may require temporary catheterization.
-
Injury to nearby organs, such as the bladder, ureters, or bowel (rare).
-
Recurrence of urinary incontinence, although this is less common with proper surgical technique.
-
Pain or discomfort around the incision or pelvic area during recovery.
6. How long is the recovery period?
-
Most women stay in the hospital 1-2 days after surgery.
-
Light activities can often resume within 1-2 weeks.
-
Full recovery, including return to exercise and sexual activity, is typically expected within 4-6 weeks.
-
Patients are encouraged to avoid heavy lifting, straining, or high-impact activities during the initial healing period.
-
Regular follow-up visits monitor healing and assess the success of the procedure.
7. Will I need catheterization after surgery?
-
A urinary catheter is usually placed during surgery to help drain the bladder.
-
After surgery, some women may require temporary catheterization if the bladder does not empty fully.
-
Catheter use is generally short-term, and normal urination typically resumes within a few days.
8. How successful is laparoscopic colposuspension?
-
Success rates are high, with most women experiencing significant improvement or complete resolution of stress urinary incontinence.
-
Long-term studies show durable results, often lasting several years, although lifestyle factors, aging, or other health conditions can affect outcomes over time.
-
Effectiveness may also depend on proper patient selection, surgeon experience, and adherence to post-operative instructions.
9. What lifestyle changes or care are recommended after surgery?
-
Avoid straining or heavy lifting for 4-6 weeks to allow proper healing.
-
Perform pelvic floor exercises as recommended by the surgeon or physiotherapist.
-
Maintain a healthy weight to reduce pressure on the bladder and pelvic floor.
-
Stay hydrated and follow instructions for diet and bowel management to prevent constipation, which can stress the surgical repair.
-
Attend all scheduled follow-ups to monitor recovery and success of the surgery.
10. What questions should I ask my surgeon before undergoing laparoscopic colposuspension?
-
Am I a good candidate for laparoscopic versus open colposuspension?
-
What is the expected success rate in my case?
-
What are the specific risks and possible complications for me?
-
How long will I need to stay in the hospital, and what is the recovery timeline?
-
Will I need temporary catheterization or any special post-operative care?
-
Are there any activities or exercises I should avoid, and when can I safely resume normal activities, including sexual activity?


