Introduction to Laparoscopic Sigmoid Colectomy
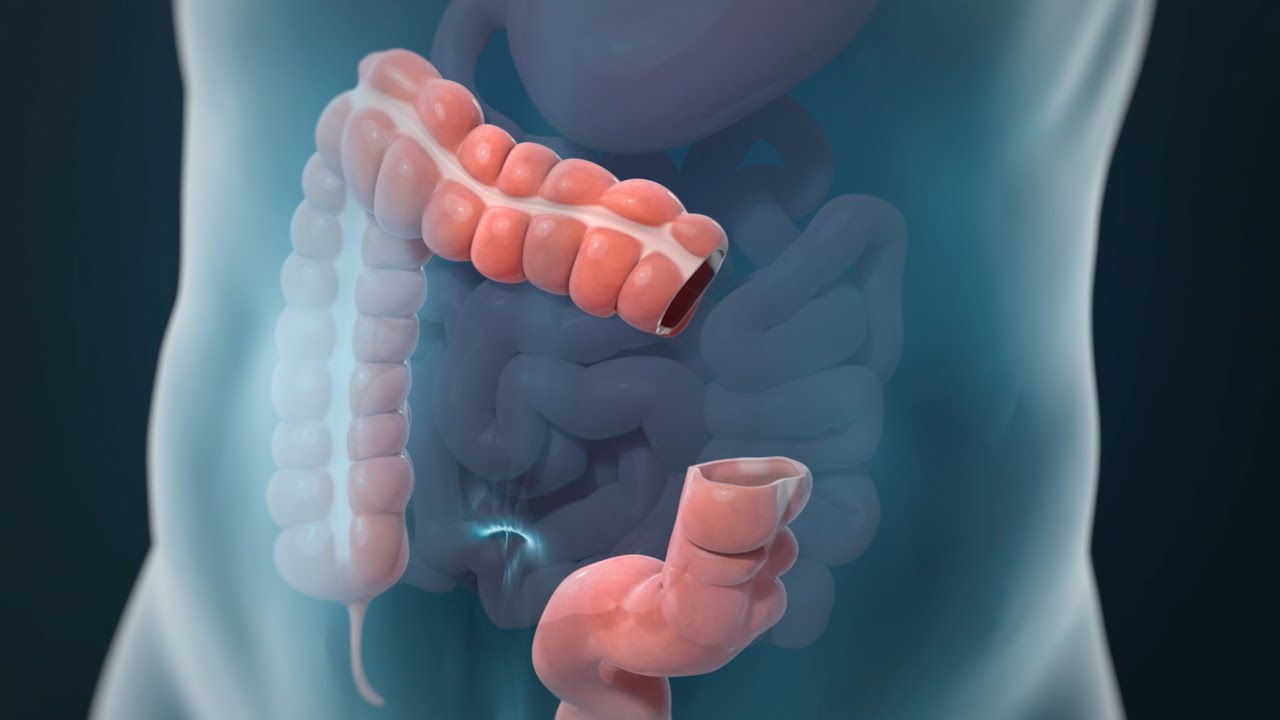
Laparoscopic Sigmoid Colectomy is a minimally invasive surgical procedure performed to remove the sigmoid colon - the S-shaped portion of the large intestine that connects the descending colon to the rectum. This section of the bowel is a frequent site of diseases such as diverticulitis, colorectal cancer, polyps, and chronic inflammatory disorders. The procedure involves the removal of the diseased portion of the sigmoid colon and the reconnection of the remaining healthy segments of the intestine (a process called anastomosis) to restore normal bowel function.
Unlike traditional open surgery, which requires a large abdominal incision, laparoscopic sigmoid colectomy uses several small keyhole incisions. Through these, a camera (laparoscope) and specialized surgical instruments are inserted. The camera provides a magnified, high-definition view of the internal organs, allowing the surgeon to operate with precision and minimal trauma.
This advanced surgical approach offers multiple advantages - smaller scars, reduced postoperative pain, shorter hospital stays, faster recovery, and a quicker return to normal activities. For many patients, laparoscopic surgery also reduces the risk of postoperative complications such as wound infection, hernias, or adhesions. With growing surgical expertise and technological advancements, laparoscopic sigmoid colectomy has become the standard of care for many benign and malignant conditions affecting the sigmoid colon.
Causes and Risk Factors Necessitating Laparoscopic Sigmoid Colectomy
Laparoscopic Sigmoid Colectomy is usually recommended when part of the sigmoid colon becomes diseased or damaged and cannot be managed with medication or non-surgical treatments. Several conditions may lead to the need for surgical resection.
Common causes include:
-
Diverticular Disease: The sigmoid colon is the most common site for diverticulosis, where small pouches form in the colon wall. Repeated inflammation (diverticulitis) can cause abscesses, strictures, or perforations requiring surgical removal of the affected segment.
-
Sigmoid Colon Cancer: Malignant tumors arising in the sigmoid colon are among the leading reasons for this procedure. Removing the affected section prevents cancer spread and restores bowel continuity.
-
Benign Tumors and Polyps: Large polyps or benign growths that cannot be safely removed during colonoscopy may require surgical resection.
-
Inflammatory Bowel Disease (IBD): Conditions like Crohn's disease or ulcerative colitis can cause chronic inflammation and scarring of the sigmoid colon, leading to obstruction or persistent pain.
-
Intestinal Obstruction: Scar tissue (adhesions) or twisting of the sigmoid colon (volvulus) can block bowel movement and necessitate surgery.
-
Ischemic Colitis: Reduced blood flow to the sigmoid colon can cause tissue death, requiring prompt resection.
-
Trauma: Rarely, abdominal injury may damage the sigmoid colon and require surgical repair.
Risk factors associated with sigmoid disease include:
-
Age: Older adults are more prone to diverticulosis and colorectal cancer.
-
Dietary Habits: Low-fiber diets and high intake of processed foods increase the risk of colon disease.
-
Sedentary Lifestyle: Lack of regular exercise can slow bowel movement and increase intraluminal pressure.
-
Obesity: Extra abdominal pressure weakens the bowel wall over time.
-
Smoking and Alcohol: Both have been linked to poor bowel health and delayed healing.
-
Genetic Predisposition: Family history of colon cancer or inflammatory bowel disorders increases susceptibility.
By identifying these risk factors early and managing them through lifestyle changes, regular screenings, and prompt treatment, patients can often delay or prevent progression to the stage where surgery becomes necessary.
Symptoms and Signs of Sigmoid Colon Disease
The symptoms that lead to laparoscopic sigmoid colectomy depend on the underlying condition but usually relate to digestive discomfort and altered bowel function. Recognizing these early helps in timely intervention.
Common symptoms include:
-
Abdominal Pain and Cramping: Typically localized in the lower left side of the abdomen, often worsened after meals or bowel movements.
-
Changes in Bowel Habits: Alternating diarrhea and constipation, or persistent constipation unrelieved by medication.
-
Rectal Bleeding or Blood in Stool: May appear as bright red streaks or dark tarry stools.
-
Bloating and Gas: Frequent abdominal distension due to partial obstruction or poor motility.
-
Mucus in Stool: Seen in inflammatory or infectious conditions of the sigmoid colon.
-
Unexplained Weight Loss and Fatigue: Common in cancer or chronic inflammatory diseases.
-
Fever and Tenderness: Especially during episodes of acute diverticulitis.
Physical examination may reveal tenderness in the lower abdomen, palpable mass (in cases of thickened or inflamed bowel), or distension due to bowel obstruction. In severe cases, signs of peritonitis (abdominal rigidity, fever, nausea, and severe pain) indicate complications like perforation, which require urgent surgical attention.
Diagnosis Before Laparoscopic Sigmoid Colectomy
Before recommending surgery, a thorough diagnostic evaluation is essential to confirm the disease, determine its extent, and assess overall patient health. Diagnosis involves a combination of clinical assessment, laboratory tests, imaging, and endoscopy.
Diagnostic Steps:
-
Medical History and Physical Examination: The doctor reviews the patient's symptoms, duration, previous medical conditions, family history of colon disease, and risk factors such as diet or smoking.
-
Blood Tests: Evaluate for anemia (due to bleeding), infection, inflammation, and nutritional status.
-
Colonoscopy: The gold standard diagnostic tool, it allows direct visualization of the sigmoid colon and removal or biopsy of suspicious lesions.
-
CT Scan of the Abdomen and Pelvis: Determines the extent of disease, identifies abscesses, fistulas, or masses, and helps surgical planning.
-
Barium Enema or CT Colonography: Provides a detailed view of colon structure, especially when colonoscopy is incomplete.
-
Stool Tests: Used to detect occult (hidden) blood or infection.
-
Preoperative Assessments: Include cardiac, pulmonary, and anesthetic evaluations to ensure the patient's fitness for laparoscopic surgery.
Accurate diagnosis helps determine whether laparoscopic surgery is suitable or if open surgery is required. It also helps in mapping the exact location of disease for precise and safe resection.
Treatment Options and Surgical Approach
When medical or conservative treatments fail, or when complications arise, laparoscopic sigmoid colectomy becomes the treatment of choice.
How the Procedure is Performed:
The surgery is performed under general anesthesia. Several small incisions are made in the abdomen through which a laparoscope and specialized instruments are inserted. The surgeon carefully separates the sigmoid colon from surrounding tissues and blood vessels, removes the diseased segment, and reconnects the healthy ends of the colon (anastomosis).
If the procedure is performed for cancer, surrounding lymph nodes are also removed for pathological examination. The small incisions are closed using sutures or surgical glue.
Benefits of the Laparoscopic Approach:
-
Smaller incisions and minimal scarring.
-
Reduced postoperative pain and quicker recovery.
-
Shorter hospital stays (typically 3-5 days).
-
Earlier return of bowel function and mobility.
-
Lower risk of wound infections and hernias.
-
Comparable or better long-term outcomes than open surgery.
Alternative Treatments:
-
Open Sigmoid Colectomy: Used when extensive adhesions, large tumors, or complications make laparoscopy unsafe.
-
Robotic-Assisted Colectomy: Offers enhanced precision and dexterity but is available mainly in specialized centers.
-
Non-Surgical Management: In mild diverticulitis or early inflammatory disease, antibiotics, dietary modifications, and close monitoring may suffice.
The choice of treatment depends on the disease type, severity, patient health, and surgeon expertise.
Prevention and Management Before and After Surgery
Prevention of Sigmoid Colon Disease:
Although not all colon diseases are preventable, lifestyle adjustments play a major role in reducing risk.
-
Eat a fiber-rich diet with plenty of fruits, vegetables, and whole grains to promote bowel movement and reduce intraluminal pressure.
-
Stay hydrated to keep stools soft and prevent constipation.
-
Engage in regular exercise to improve intestinal motility.
-
Avoid smoking and excessive alcohol.
-
Undergo regular colon cancer screening after age 45, or earlier if there is a family history.
Preoperative Preparation:
-
Bowel preparation (using prescribed laxatives) to empty the colon before surgery.
-
Fasting as advised to ensure an empty stomach during anesthesia.
-
Temporary discontinuation of blood-thinning medications, as directed by the doctor.
-
Optimizing chronic conditions like diabetes, hypertension, and heart disease.
Postoperative Care and Recovery:
-
Patients are encouraged to walk within 24 hours to prevent blood clots and stimulate bowel function.
-
Diet is advanced gradually - from clear liquids to soft foods - as bowel movements return.
-
Pain is managed with oral medications.
-
Avoid heavy lifting and strenuous activity for 4-6 weeks.
-
Maintain a high-protein diet to promote tissue healing.
-
Regular follow-ups for wound checks and recovery evaluation.
Proper management before and after surgery ensures smooth healing, prevents complications, and promotes long-term digestive health.
Complications of Laparoscopic Sigmoid Colectomy
Laparoscopic sigmoid colectomy is generally safe, but potential risks should be discussed with every patient.
Possible Complications Include:
-
Bleeding: Minimal due to small incisions, but may occur at surgical sites.
-
Infection: Can develop in incisions or within the abdomen; antibiotics and sterile care reduce this risk.
-
Anastomotic Leak: A rare but serious condition where the bowel connection leaks; requires prompt treatment.
-
Bowel Obstruction: May occur due to adhesions or scarring post-surgery.
-
Ileus: Temporary slowing of bowel movement after surgery, causing bloating and nausea.
-
Blood Clots: Early ambulation and leg exercises help prevent deep vein thrombosis.
-
Conversion to Open Surgery: In rare cases when visibility or anatomy is difficult.
Risk factors for complications include older age, obesity, diabetes, malnutrition, smoking, and emergency surgery situations. However, experienced laparoscopic surgeons and enhanced recovery protocols have significantly reduced these risks.
Living with the Condition Before and After Surgery
Before Surgery:
Patients with sigmoid colon disease often experience discomfort, dietary restrictions, and emotional distress. Recurrent pain, irregular bowel habits, and the fear of cancer or complications can impact both physical and mental well-being. Education, nutritional guidance, and psychological support play vital roles in preparing patients for surgery and recovery.
After Surgery:
Most patients recover rapidly following laparoscopic sigmoid colectomy. Within a few weeks, bowel function stabilizes, energy levels improve, and pain subsides. Patients can usually return to work and regular activities within 4-6 weeks, depending on their health.
Long-Term Lifestyle Tips:
-
Eat a balanced diet with adequate fiber.
-
Avoid processed foods and red meat.
-
Stay physically active.
-
Quit smoking and limit alcohol.
-
Follow up regularly with your doctor, especially if the surgery was for cancer.
-
Stay attentive to changes in bowel habits or abdominal pain and report them early.
Emotional and physical recovery after surgery is equally important. Most patients experience a significant improvement in quality of life, freedom from chronic pain, and peace of mind knowing the disease has been treated effectively.
Top 10 Frequently Asked Questions about Laparoscopic Sigmoid Colectomy
1. What is a laparoscopic sigmoid colectomy?
A laparoscopic sigmoid colectomy is a minimally invasive surgery that removes the diseased segment of the sigmoid colon (the part of the large intestine closest to the rectum) using small abdominal incisions and a camera. After the diseased segment is removed, the healthy ends of the colon are re-connected so normal bowel passage can continue.
2. Why is this surgery recommended?
It is recommended when conditions affecting the sigmoid colon require surgical removal, for example:
-
Recurrent or complicated diverticulitis (inflammation of pouches in the colon)
-
Colon cancer located in the sigmoid colon
-
Benign strictures or narrowing of the sigmoid
-
Bleeding, obstruction or perforation in that region of the bowel
The laparoscopic approach is chosen to shorten recovery, reduce pain and improve patient comfort compared to open surgery.
3. What are the main benefits of the laparoscopic approach?
Key advantages include:
-
Smaller incisions → less pain and faster healing
-
Shorter hospital stay and quicker return to everyday activities
-
Reduced wound-complications (such as large scar, infection)
-
Better cosmetic result due to minimal scars
-
Faster return of bowel function (gas, stool) in many cases
4. Who is a suitable candidate and who might not be?
Suitable patients are generally those who:
-
Are medically fit for general anesthesia
-
Have sigmoid colon disease appropriate for resection
-
Do not have prohibitive abdominal adhesions from previous surgeries
Patients who may not be suitable include those with:
-
Very extensive prior abdominal operations and dense scar tissue
-
Very large tumours or widespread disease making laparoscopic access difficult
-
Emergency situations where rapid access is required and laparoscopic approach may not be feasible
5. How is the procedure performed?
In brief, the surgery involves:
-
Under general anesthesia, several small ports (small incisions) are placed in the abdomen
-
A camera (laparoscope) guides the surgeon as the diseased sigmoid colon segment is mobilised
-
The segment is removed, and the healthy ends of colon are re-connected (anastomosis) or sometimes a temporary stoma is created if needed
-
The small incisions are closed and the patient is moved to recovery
6. What is the typical recovery timeline?
While individual cases vary, typical expectations:
-
Hospital stay may be around 2 to 5 days (for uncomplicated cases)
-
Bowel function (passing gas/stool) may resume within a day or two
-
Light activity may resume within 1-2 weeks
-
Full return to normal activity (work, exercise) may take 4-6 weeks depending on the patient's health and extent of surgery
-
Diet will gradually progress from liquids to soft foods to a normal diet under guidance
7. What are potential risks and complications?
As with any major surgical procedure, risks include:
-
Bleeding or infection at the surgical site or internally
-
Anastomotic leak (leakage at the connection between colon ends) which may require further intervention
-
Injury to adjacent organs (small bowel, bladder, ureter) though rare
-
Conversion to open surgery if laparoscopic access becomes difficult
-
Formation of scar tissue or adhesions after surgery, which may lead to bowel obstruction in future
8. What dietary or lifestyle changes are needed after surgery?
After surgery:
-
A gradual diet progression is used: starting from clear liquids → soft diet → normal diet as tolerated
-
Avoid heavy lifting, strenuous exercise or abdominal strain for several weeks
-
Walking and light activity are encouraged early to support recovery and bowel function
-
Long term: healthy diet (often higher fibre), maintaining healthy weight, avoiding smoking, and regular follow-up with your surgeon or gastroenterologist
9. Will I need a stoma or additional treatment after surgery?
Sometimes yes. A stoma (temporary or permanent) may be required if the surgeon cannot safely reconnect the colon ends at surgery or if the patient's condition requires diversion of stool. Additionally, if surgery is done for cancer, further treatments (such as chemotherapy or radiation) may be necessary depending on pathology results. Your surgeon will discuss this possibility beforehand.
10. What questions should I ask my surgeon before undergoing the procedure?
Important questions to ask include:
-
Which exact segment of my sigmoid colon will be removed and why?
-
Why has laparoscopic approach been chosen for my case, and what is the chance of needing open surgery instead?
-
What is the expected hospital stay and recovery timeline in my case?
-
What are the specific risks in my situation (based on my age, general health, previous surgeries)?
-
Will I need a stoma? If yes, temporary or permanent?
-
What diet, activity, and follow-up care will I need after surgery?
-
What outcomes can I reasonably expect, and what might affect them?


