Introduction to Laparoscopic Splenectomy
Laparoscopic Splenectomy is a modern, minimally invasive surgical technique used to remove the spleen - an organ located in the upper left abdomen, just below the rib cage. The spleen plays a vital role in the body's immune system. It filters and removes old or damaged blood cells, stores platelets, and helps fight certain bacterial infections. However, in some medical conditions, the spleen may become diseased, enlarged, or overactive, leading to serious health problems that can only be resolved through its surgical removal.
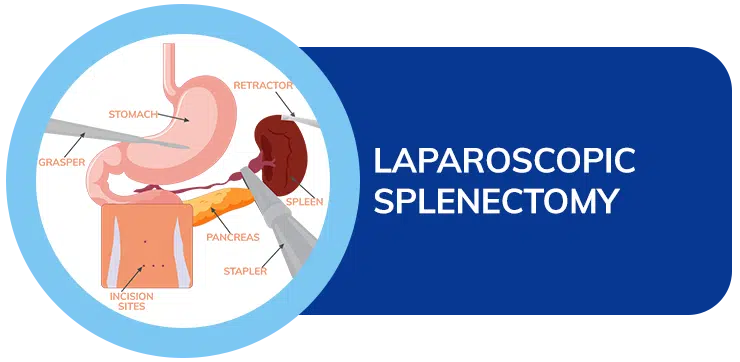
In laparoscopic splenectomy, instead of making one large incision, surgeons make a few small cuts through which a camera (laparoscope) and specialized instruments are inserted. The laparoscope transmits a high-definition image to a monitor, enabling the surgeon to perform precise and delicate maneuvers to detach and remove the spleen. The minimally invasive approach offers significant advantages over traditional open surgery, including less postoperative pain, shorter hospital stays, faster recovery, smaller scars, and lower risk of infection or hernias.
This procedure has now become the preferred approach for most elective splenectomy cases, particularly for benign hematological diseases, immune disorders, and certain cases of splenic cysts or trauma. However, in cases of massive splenomegaly (greatly enlarged spleen) or emergency trauma with active bleeding, an open splenectomy may still be necessary. Overall, laparoscopic splenectomy has revolutionized spleen surgery by combining safety, precision, and faster recovery.
Causes and Risk Factors Leading to Laparoscopic Splenectomy
There are several reasons why a patient may require splenectomy, ranging from blood-related disorders to traumatic injuries. The spleen can become overactive, damaged, infected, or enlarged due to various medical conditions. When it begins to harm the body rather than help it - for example, by destroying healthy blood cells - surgical removal becomes the best option.
Common causes for splenectomy include:
-
Hematological Disorders:
Conditions such as Idiopathic Thrombocytopenic Purpura (ITP), Hereditary Spherocytosis, and Autoimmune Hemolytic Anemia cause the spleen to mistakenly destroy blood cells, resulting in anemia and low platelet counts. Removing the spleen can normalize blood counts and prevent complications. -
Splenic Rupture or Trauma:
The spleen is delicate and can rupture due to accidents, sports injuries, or abdominal trauma, leading to life-threatening internal bleeding. In severe cases, splenectomy becomes necessary. -
Splenic Cysts and Abscesses:
Large cysts, infections, or abscesses that do not respond to antibiotics or drainage may require surgical removal. -
Hypersplenism:
This is a condition where the spleen becomes overactive and starts destroying normal blood cells excessively, causing anemia, leukopenia (low white blood cells), and thrombocytopenia (low platelets). -
Cancers and Tumors:
Cancers such as lymphoma, leukemia, or metastases (spread of other cancers to the spleen) sometimes necessitate splenectomy either for treatment or for diagnostic biopsy. -
Portal Hypertension and Liver Disease:
In conditions like cirrhosis, the spleen enlarges due to increased pressure in the portal vein, leading to hypersplenism.
Risk Factors That May Lead to Splenectomy:
-
Family history of blood or immune disorders.
-
Chronic infections or inflammatory diseases.
-
Prior abdominal injury or surgery.
-
Obesity, smoking, or alcohol abuse (which compromise immunity and healing).
-
Certain medications or autoimmune diseases that affect spleen function.
While splenectomy treats these underlying problems, it also removes part of the body's immune defense. Therefore, vaccination and infection prevention become critical components of long-term management.
Symptoms and Signs Indicating the Need for Splenectomy
Symptoms vary depending on the condition affecting the spleen, but many arise from splenomegaly - the abnormal enlargement of the spleen. When the spleen becomes enlarged, it presses on nearby organs, causes pain, and often leads to blood-related symptoms.
Common symptoms include:
-
Abdominal Pain or Fullness:
A dull ache or sharp pain in the upper left abdomen, sometimes radiating to the left shoulder or back. The discomfort may worsen after eating due to pressure on the stomach. -
Early Satiety and Loss of Appetite:
A large spleen compresses the stomach, causing a feeling of fullness even after small meals. -
Fatigue and Weakness:
Excessive destruction of red blood cells leads to anemia, resulting in tiredness and shortness of breath. -
Frequent Infections:
A malfunctioning spleen impairs immune function, making the patient more prone to bacterial infections. -
Easy Bruising or Bleeding:
Low platelet counts can cause prolonged bleeding from minor cuts or unexplained bruising. -
Fever and Malaise:
These can occur due to infections or splenic abscesses.
On physical examination, doctors may feel an enlarged spleen under the left rib cage or note signs of anemia and jaundice. Persistent or worsening symptoms, coupled with abnormal blood test results, are key indicators that surgical removal may be necessary.
Diagnosis Before Laparoscopic Splenectomy
A careful diagnostic evaluation is essential to determine the cause of spleen enlargement or dysfunction and to ensure the patient is fit for surgery. The diagnosis involves a combination of clinical examination, laboratory tests, and imaging studies.
Key diagnostic steps include:
-
Comprehensive Medical History:
Understanding the duration of symptoms, prior infections, blood disorders, family history, or recent injuries. -
Physical Examination:
The doctor checks for abdominal tenderness, spleen size, and signs of anemia, bleeding, or liver disease. -
Blood Tests:
-
Complete blood count (CBC) to assess red and white blood cells and platelets.
-
Peripheral blood smear to look for abnormal cell shapes (spherocytes, schistocytes).
-
Liver function tests to check for associated liver disease.
-
Clotting tests to ensure normal blood coagulation before surgery.
-
-
Imaging Tests:
-
Ultrasound of the abdomen to assess spleen size and structure.
-
CT or MRI scans for detailed evaluation and to check for cysts, tumors, abscesses, or rupture.
-
Nuclear medicine scans to assess splenic function and locate accessory spleens.
-
-
Vaccination Status Check:
Before surgery, the patient should be immunized against pneumococcus, meningococcus, and Haemophilus influenzae to prevent infections post-splenectomy. -
Preoperative Evaluation:
Includes cardiac and pulmonary assessment, anesthesia review, and optimization of chronic diseases such as diabetes or hypertension.
A complete diagnostic workup ensures that laparoscopic splenectomy is both necessary and safe for the patient.
Treatment Options and Surgical Approach
Non-Surgical Treatments (When Possible):
In early stages or mild cases, doctors may try medications like corticosteroids or immunosuppressants, especially for immune-related blood disorders. Antibiotics are used for infections or abscesses. However, when these treatments fail, or when there is severe splenic enlargement or rupture, splenectomy becomes unavoidable.
Laparoscopic Splenectomy Procedure:
-
The procedure is performed under general anesthesia.
-
The patient is positioned on their right side to provide clear access to the spleen in the upper left abdomen.
-
Three to four small incisions are made to insert the laparoscope (camera) and surgical instruments.
-
The surgeon carefully detaches the spleen from surrounding structures - including the diaphragm, pancreas, and stomach - while controlling the splenic artery and vein to prevent bleeding.
-
Once freed, the spleen is placed in a sterile retrieval bag and removed through one of the incisions.
-
The small incisions are then closed with sutures or medical glue.
Advantages of the Laparoscopic Technique:
-
Minimal postoperative pain and faster recovery.
-
Smaller scars and better cosmetic results.
-
Lower blood loss and reduced infection risk.
-
Shorter hospital stay (typically 2-3 days).
-
Quicker return to normal activities.
In some complex cases, the surgeon may use a hand-assisted laparoscopic technique or convert to open surgery for safety reasons, especially if the spleen is very large or bleeding is excessive.
Prevention and Management Before and After Surgery
Preoperative Preparation:
Proper preparation significantly improves surgical outcomes.
-
Vaccinations should be completed at least 2 weeks before surgery to protect against infection.
-
The patient should stop smoking and limit alcohol consumption to improve lung function and healing.
-
Medications that thin the blood (like aspirin or warfarin) are discontinued as advised.
-
Patients are encouraged to maintain a nutritious diet to strengthen immunity and promote recovery.
-
In emergency splenectomy cases, vaccines are administered after surgery.
Postoperative Care:
-
Hospital stay is generally short - about 1 to 3 days for laparoscopic procedures.
-
Pain is usually mild and managed with oral medications.
-
Early movement and walking are encouraged to prevent blood clots.
-
The patient can gradually resume normal eating and light activity within a few days.
-
Avoid strenuous activities and heavy lifting for at least 4-6 weeks.
-
Regular follow-up visits ensure proper healing and monitor blood counts.
Long-Term Management:
Since the spleen contributes to the immune system, patients need lifelong infection prevention.
-
Regular booster vaccinations as recommended.
-
Immediate medical care for any fever or infection.
-
Some may require preventive antibiotics, especially children and those with immune conditions.
-
Carrying a medical alert card or bracelet indicating “No Spleen” is recommended for emergencies.
Proper prevention and management before and after surgery ensure long-term success and protection against complications.
Complications of Laparoscopic Splenectomy
Although laparoscopic splenectomy is a safe and reliable procedure, it carries certain risks, as with any surgery.
Possible complications include:
-
Bleeding: Controlled using clips or cautery, but may occasionally require blood transfusion.
-
Injury to Adjacent Organs: The stomach, pancreas, or colon may be accidentally injured during surgery.
-
Infection: Reduced immune function can increase susceptibility to bacterial infections.
-
Anesthesia-related issues: Nausea, vomiting, or breathing difficulties, usually short-term.
-
Subphrenic Abscess: Rare fluid collection under the diaphragm, treated with antibiotics or drainage.
-
Deep Vein Thrombosis (DVT): Prevented through early movement and medication.
-
Overwhelming Post-Splenectomy Infection (OPSI): A rare but serious infection that can develop years after surgery; vaccination and awareness are key to prevention.
Most complications are rare and preventable through careful surgical technique, proper preparation, and adherence to postoperative care instructions.
Living Without a Spleen: Life After Splenectomy
Living without a spleen is entirely possible, but it requires a proactive approach to maintaining health. The body adapts by using other organs, such as the liver and lymph nodes, to compensate for some of the spleen's functions.
Life after Surgery:
-
Most patients feel stronger and healthier once the underlying condition is resolved.
-
Normal daily activities can resume within 2-4 weeks for laparoscopic patients.
-
Diet should include balanced nutrients to boost immunity.
-
Avoid contact sports or trauma to the abdomen for several months.
-
Regular medical check-ups and blood tests are essential.
Long-Term Precautions:
-
Always seek immediate medical attention for fevers, chills, or unexplained illness.
-
Keep up with vaccination schedules and boosters.
-
Maintain good hygiene and avoid exposure to contagious diseases.
-
Carry an emergency medical identification indicating splenectomy status.
With these precautions, patients can lead a healthy, active, and fulfilling life after spleen removal.
Top 10 Frequently Asked Questions about Laparoscopic Splenectomy
1. What is a Laparoscopic Splenectomy?
A laparoscopic splenectomy is a minimally invasive surgery in which the spleen is removed using a laparoscope (a small camera) and specialized instruments inserted through tiny abdominal incisions. It replaces the traditional open approach, offering smaller scars, less pain, and faster recovery.
2. Why is a Laparoscopic Splenectomy performed?
This surgery is recommended when the spleen becomes diseased, enlarged, or damaged. Common reasons include:
-
Idiopathic Thrombocytopenic Purpura (ITP)
-
Hereditary Spherocytosis
-
Autoimmune Hemolytic Anemia
-
Hypersplenism (overactive spleen)
-
Splenic cysts, abscesses, or tumors
-
Splenic rupture due to trauma (in selected cases)
3. How is the procedure performed?
Under general anesthesia, several small incisions are made in the abdomen. A camera provides magnified images while the surgeon carefully detaches the spleen from surrounding tissues and blood vessels. The spleen is then placed in a retrieval bag and removed through one of the small openings. The operation typically takes 1.5-3 hours.
4. What are the benefits of laparoscopic splenectomy compared to open surgery?
-
Smaller incisions and less visible scarring
-
Reduced postoperative pain and blood loss
-
Faster recovery and shorter hospital stay (2-4 days)
-
Quicker return to normal activities
-
Lower risk of wound infection or hernia formation
5. What are the possible risks or complications?
Although laparoscopic splenectomy is considered safe, potential complications include:
-
Bleeding or injury to nearby organs (stomach, pancreas, colon)
-
Infection or abscess formation
-
Blood clots (deep vein thrombosis or pulmonary embolism)
-
Conversion to open surgery if bleeding or technical difficulty occurs
-
Rarely, overwhelming post-splenectomy infection (OPSI) if vaccinations are missed
6. Do I need any vaccinations before or after the surgery?
Yes. The spleen helps fight infections, so vaccines are crucial to prevent serious illnesses. Typically, vaccines are given 2 weeks before elective surgery or after recovery if the surgery is urgent. Recommended vaccines include:
-
Pneumococcal vaccine
-
Meningococcal vaccine
-
Haemophilus influenzae type b (Hib) vaccine
Booster doses may be needed later as advised by your doctor.
7. How long is the recovery period after a laparoscopic splenectomy?
Most patients stay in the hospital for 2-4 days. You can usually resume light activity within 1-2 weeks and return to full activity in 4-6 weeks. You may experience mild shoulder or abdominal discomfort for a few days. Avoid heavy lifting or strenuous exercise until your surgeon clears you.
8. How will my life change after my spleen is removed?
You can lead a normal life without a spleen, but your immune system becomes slightly weaker. You'll need to:
-
Stay updated on all vaccinations
-
Seek prompt medical help for fever or infection
-
Possibly take preventive antibiotics if advised (especially children or those with weak immunity)
With proper precautions, most people live healthy, active lives post-splenectomy.
9. Are there any long-term precautions after spleen removal?
Yes. Lifelong infection precautions are important:
-
Always inform doctors and dentists that you've had a splenectomy
-
Carry a medical ID stating “No Spleen”
-
Get medical attention immediately for fever above 38°C (100.4°F)
-
Avoid travel to malaria-prone areas or take preventive medication if necessary
10. What are the long-term outcomes of laparoscopic splenectomy?
Laparoscopic splenectomy has an excellent success rate. Most patients experience complete relief of symptoms related to their blood or splenic disorders. With proper vaccination, infection prevention, and regular follow-ups, long-term health and quality of life remain excellent.


