Introduction to Laparoscopic Sterilization
Laparoscopic Sterilization, also known as tubal ligation, is a minimally invasive surgical procedure that provides permanent birth control for women. It involves blocking, sealing, or cutting the fallopian tubes - the structures that carry eggs from the ovaries to the uterus - to prevent fertilization. After sterilization, sperm cannot reach the egg, and pregnancy becomes virtually impossible.
The laparoscopic approach is the most advanced and widely preferred method of female sterilization due to its safety, simplicity, and quick recovery time. Unlike traditional open surgery, laparoscopic sterilization is performed through small keyhole incisions in the abdomen. A laparoscope (a thin tube with a light and camera) is inserted to provide a clear view of the reproductive organs. Using specialized instruments, the surgeon either seals the tubes with clips, rings, or electric cautery or removes a portion of the tubes altogether.
This procedure is usually done under general or local anesthesia and takes about 20-30 minutes. Most women go home the same day and can return to normal activities within a few days. Laparoscopic sterilization is over 99% effective and provides lifelong contraception, making it one of the most reliable and permanent methods available.
Laparoscopic sterilization does not affect hormone levels, menstrual cycles, or sexual desire. It is a safe and effective choice for women who are certain they do not wish to have children in the future.
Causes and Risks Leading to Laparoscopic Sterilization
Laparoscopic sterilization is a voluntary and elective procedure chosen primarily for family planning. Women typically opt for this surgery when they are confident that they do not want to conceive in the future. While it is a preventive measure rather than a treatment for disease, there are various social, medical, and personal factors that contribute to the decision.
Common reasons for choosing laparoscopic sterilization include:
-
Completed Family: Women who already have the desired number of children and wish to avoid further pregnancies.
-
Health Risks with Pregnancy: Certain medical conditions - such as severe heart disease, kidney disorders, diabetes, or hypertension - may make future pregnancies dangerous.
-
Genetic or Hereditary Concerns: Some women opt for sterilization to avoid passing on inherited diseases or disorders.
-
Failed Contraceptive Methods: When temporary contraceptives like pills, intrauterine devices (IUDs), or injections fail or cause side effects.
-
Socioeconomic or Psychological Reasons: Financial limitations, relationship stability, or psychological readiness to end childbearing.
Risk Factors Associated with the Procedure:
Although laparoscopic sterilization is safe, several factors can increase the risks of complications:
-
Obesity: Makes visualization of pelvic organs more challenging.
-
Previous Abdominal Surgery: Scar tissue (adhesions) may make the procedure more complex.
-
Pelvic Infections: Past pelvic inflammatory disease (PID) can distort the fallopian tubes.
-
Anesthesia Reactions: Allergic or adverse reactions to anesthesia are rare but possible.
-
Bleeding or Infection Risks: Minimal but possible at incision or internal sites.
-
Regret: Some women may later desire reversal or future pregnancies, which are difficult or impossible after sterilization.
It's essential for women to receive preoperative counseling to fully understand the permanent nature of the procedure and explore alternative methods before making the final decision.
Symptoms and Signs Related to Laparoscopic Sterilization
Since laparoscopic sterilization is a planned elective surgery rather than a disease treatment, there are no “symptoms” that directly indicate a need for it. However, it is often considered by women who are experiencing issues related to other contraceptive methods or medical concerns that make pregnancy unsafe.
Common signs that may lead a woman to consider sterilization:
-
Repeated contraceptive failures or side effects from hormonal pills or
devices.
-
Concerns about health risks associated with pregnancy.
-
Desire for a long-term, maintenance-free contraceptive method.
-
History of multiple pregnancies and decision not to have more children.
Post-Sterilization Symptoms (Normal Reactions):
Repeated contraceptive failures or side effects from hormonal pills or devices.
Concerns about health risks associated with pregnancy.
Desire for a long-term, maintenance-free contraceptive method.
History of multiple pregnancies and decision not to have more children.
After the procedure, some mild and temporary symptoms may occur:
-
Slight abdominal pain or cramping.
-
Shoulder or neck discomfort from gas used during laparoscopy.
-
Mild nausea or fatigue due to anesthesia.
-
Minor bleeding or discharge from incision sites.
These symptoms are normal and usually resolve within a few days. Persistent pain, fever, or heavy bleeding should be promptly evaluated by the doctor.
Diagnosis and Evaluation Before Laparoscopic Sterilization
Before performing laparoscopic sterilization, a thorough evaluation is conducted to ensure the patient's health and suitability for the procedure. This assessment focuses on medical history, reproductive status, and overall fitness for anesthesia and surgery.
Preoperative evaluation includes:
-
Medical History Review: The doctor discusses past pregnancies, contraceptive use, medical conditions, and medications.
-
Physical and Pelvic Examination: To check for infections, uterine or pelvic abnormalities.
-
Blood and Urine Tests: Evaluate hemoglobin, blood sugar, clotting function, and rule out infections.
-
Pregnancy Test: To ensure the patient is not pregnant at the time of surgery.
-
Imaging (if needed): Ultrasound to assess pelvic anatomy.
-
Counseling Session: Explains the procedure, risks, benefits, and emphasizes the irreversibility of sterilization.
-
Consent: Written informed consent is obtained after explaining all aspects and alternatives.
Laparoscopic sterilization is often scheduled during the follicular phase (within 7-10 days after menstruation) to rule out early pregnancy and ensure the uterus and tubes are clearly visible during surgery.
Treatment Options and Surgical Procedure
Laparoscopic sterilization is performed under general or local anesthesia and typically takes less than 30 minutes. It may be done as a day-care procedure, meaning the patient can go home the same day.
Steps of the Laparoscopic Sterilization Procedure:
-
Anesthesia and Positioning: The patient is given anesthesia, and a small incision is made near the navel.
-
Insertion of the Laparoscope: A thin camera is inserted to visualize the reproductive organs.
-
Gas Insufflation: The abdomen is gently filled with carbon dioxide gas to create space for viewing and movement.
-
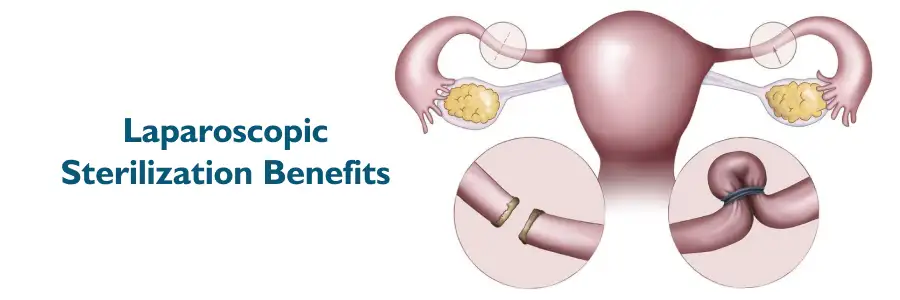
Tubal Occlusion: The surgeon uses one of several techniques to block the fallopian tubes:
-
Filshie Clips or Rings: Tiny clips or silicone bands are applied to close the tubes.
-
Electrocautery (Diathermy): Uses heat to seal and cut the tubes.
-
Tubal Segment Removal: A small section of each tube is removed.
-
-
Inspection and Closure: After confirming proper sealing, the gas is released, and the incisions are closed with absorbable sutures.
Advantages of Laparoscopic Sterilization:
-
Minimally invasive and quick recovery.
-
Very high success rate (99.5-99.8%).
-
Minimal hospital stay.
-
No effect on hormonal balance, sexual function, or menstrual cycle.
-
Suitable for women seeking a permanent solution.
Alternative Sterilization Methods:
-
Mini-laparotomy: A small incision-based method often used after childbirth.
-
Hysteroscopic Sterilization: A non-surgical approach (less common today).
-
Male Sterilization (Vasectomy): A simpler and safer alternative in some families.
The choice of method depends on patient preference, medical condition, and surgeon expertise.
Prevention and Management Before and After Surgery
Preoperative Preparation:
-
Avoid eating or drinking 8 hours before surgery.
-
Take prescribed medications as instructed.
-
Maintain hygiene to reduce infection risk.
-
Arrange for an accompanying person for discharge after surgery.
Postoperative Management:
-
Rest for 24-48 hours and avoid strenuous activity for a few days.
-
Pain is minimal and can be managed with mild analgesics.
-
Avoid sexual intercourse for one week or until advised.
-
Keep incision sites clean and dry; report redness or discharge to your doctor.
-
Resume a normal diet as tolerated.
-
A follow-up visit is recommended within one week.
Long-Term Management:
-
Use temporary contraception until the first menstrual period after surgery (as rare early ovulation-related pregnancies can occur).
-
Continue regular gynecological check-ups.
-
Maintain healthy habits and a balanced diet.
-
Emotional counseling if any feelings of regret or adjustment difficulties arise.
Proper care before and after surgery ensures safe healing and prevents complications.
Complications of Laparoscopic Sterilization
While laparoscopic sterilization is extremely safe, minor complications may occur in a small percentage of cases.
Possible complications include:
-
Bleeding or Infection: At incision sites or internally; managed with antibiotics or minor interventions.
-
Injury to Surrounding Organs: Rare injury to bowel, bladder, or blood vessels may occur.
-
Gas-Related Discomfort: Shoulder pain or bloating due to residual gas; usually temporary.
-
Failed Sterilization: Extremely rare (less than 1%), leading to unintended pregnancy, sometimes ectopic.
-
Anesthesia Complications: Mild nausea or dizziness, generally short-lived.
-
Psychological Impact: Some women may experience regret or mood changes, emphasizing the importance of pre-surgery counseling.
Overall, complication rates are very low when performed by experienced surgeons using proper techniques and sterile precautions.
Living with Laparoscopic Sterilization
Laparoscopic sterilization allows women to live freely without the fear of unplanned pregnancies, offering both physical and emotional relief. Most women report improved quality of life and satisfaction with their decision, especially when well-informed and emotionally prepared before the procedure.
Life After Sterilization:
-
Menstrual cycles remain normal - sterilization does not affect hormones or cause early menopause.
-
Sexual life continues as before; many women report greater satisfaction due to freedom from pregnancy anxiety.
-
No need for daily, monthly, or device-based contraception.
-
Ability to return to normal work or activities within a few days.
-
Continuous protection without the side effects of hormonal methods.
Important Considerations:
-
The procedure is permanent; reversal is difficult, expensive, and not always successful.
-
Emotional adjustment is important - counseling and support can help in cases of regret.
-
Regular gynecological health checks should continue as part of overall well-being.
Laparoscopic sterilization is thus a safe, permanent, and convenient solution for women who wish to end childbearing while maintaining hormonal balance and reproductive health.
Top 10 Frequently Asked Questions about Laparoscopic Sterilization
1. What is laparoscopic sterilization?
Laparoscopic sterilization is a surgical procedure to permanently prevent pregnancy by
blocking or sealing the fallopian tubes. It is done via small key-hole incisions in the
abdomen with a laparoscope (camera) and instruments that allow the surgeon to locate,
access and occlude the tubes.
The aim is to stop sperm from reaching an egg, so fertilization and pregnancy cannot
occur.
2. How is the procedure performed?
Under general (or sometimes regional) anesthesia, the surgeon makes one or more small
incisions in the abdomen (often near the navel and lower abdomen). The abdomen is
inflated with a harmless gas so the organs can be seen clearly, and a laparoscope and
instruments are inserted.
The fallopian tubes are then cut, sealed, clipped or blocked with rings/implants,
depending on the method. Finally, the instruments are removed and the small incisions
are closed.
Because the incisions are small, recovery is typically faster than in older open
procedures.
3. Who is a good candidate for laparoscopic sterilization?
This option is appropriate for a woman who:
-
Clearly does not wish to become pregnant in the future, as the procedure is intended to be permanent.
-
Is medically fit for laparoscopic surgery and anesthesia.
-
Has been fully informed and counselled about the permanence, risks, alternatives and what the procedure involves.
If there is any doubt about wanting future children, other long-acting but reversible methods should be considered first.
4. What are the benefits of this method compared to other sterilization techniques?
Some of the key advantages include:
-
Small incisions, which often mean less pain, less visible scarring and shorter recovery time.
-
Immediate effectiveness: once the tubes are occluded, the chance of pregnancy is very low (although not zero).
-
Because it is laparoscopic, the surgeon may also inspect the pelvic organs for any unexpected findings during surgery.
-
In suitable patients, it may allow same-day or very short hospital stays.
5. What are the risks or complications?
Although generally safe, laparoscopic sterilization carries some risks:
-
Typical surgical risks: infection, bleeding, adverse anesthesia reactions.
-
Possible injury to nearby organs (bowel, bladder, blood vessels) although rare.
-
Risk of failure of the sterilization (i.e., pregnancy still occurs) - this risk is low but non-zero.
-
If pregnancy does occur after sterilization, the risk of an ectopic pregnancy (pregnancy outside the uterus) is higher than in women without sterilization.
-
Because the procedure is permanent, regret can occur - especially if life circumstances change (e.g., loss of child, remarriage).
Counseling beforehand is key.
6. Will this procedure affect my menstrual cycle, sexual life or hormones?
-
In general, laparoscopic sterilization does not affect your hormones or menstrual cycle. You will continue to ovulate and menstruate as before (unless you were already on hormonal methods).
-
It should not negatively impact your sexual desire or function - in fact many women say they feel more relaxed because they no longer fear unintended pregnancy.
-
Any changes in bleeding are likely due to prior contraceptive methods or underlying gynecological issues, not the sterilization itself.
7. How long is the recovery time and what should I expect afterward?
-
Many women can go home the same day or after a short hospital stay, depending on
local protocol and personal recovery.
-
You may experience mild abdominal discomfort, shoulder pain (from gas used in
laparoscopy), bloating, or nausea for a few days.
-
Light activity is usually encouraged early (walking, gentle movement) but
strenuous exercise, heavy lifting and abdominal strain should be avoided for
several weeks.
-
Most women return to normal daily activities within 1 to 2 weeks, though full
recovery (especially of energy and complete comfort) may take a little longer.
8. Is it really permanent? What if I want children later?
Many women can go home the same day or after a short hospital stay, depending on local protocol and personal recovery.
You may experience mild abdominal discomfort, shoulder pain (from gas used in laparoscopy), bloating, or nausea for a few days.
Light activity is usually encouraged early (walking, gentle movement) but strenuous exercise, heavy lifting and abdominal strain should be avoided for several weeks.
Most women return to normal daily activities within 1 to 2 weeks, though full recovery (especially of energy and complete comfort) may take a little longer.
Yes, sterilization by this method is intended to be permanent - it is
not easily reversible. While some reversal surgeries exist, they are
expensive, not always successful, and come with increased risks (including higher risk
of ectopic pregnancy).
Therefore, you should only choose this method if you are sure you don't
want future pregnancy. If you might want children, alternative methods (e.g., IUDs,
implants) should be considered.
9. What are the alternatives to laparoscopic sterilization?
Alternative options include:
-
Long-acting reversible contraception (LARC) such as intrauterine devices (IUDs) or contraceptive implants, which allow fertility to return when removed.
-
A partner's vasectomy (male sterilization), which may be simpler and safer in some cases.
-
Permanent (non-surgical) contraception is still not available, so the only true “permanent” methods are female or male sterilization.
Discussing all options with your healthcare provider helps you choose the best fit for you.
10. What should I ask my doctor before undergoing the procedure?
Important questions to ask include:
-
Why is this method being recommended for me, and am I sure I don't want more children in the future?
-
How will the surgery be performed, and what is the plan for my recovery in my particular case?
-
What are the risks in my situation (based on my age, medical history, weight, previous surgeries)?
-
What is the chance of pregnancy failure after the procedure? What happens if pregnancy does occur?
-
What post-operative instructions will I need (activity, diet, follow-up visits)?
-
What other contraception options did I explore, and why was sterilization chosen?


