Introduction to Laparoscopy Duodenal Perforation Closure
A duodenal perforation is a serious, life-threatening condition in which a hole develops in the wall of the duodenum - the first part of the small intestine that connects to the stomach. This allows gastric contents, bile, and digestive juices to leak into the abdominal cavity, leading to severe infection and peritonitis. Traditionally, the condition required an open abdominal surgery, but with advances in minimally invasive technology, laparoscopy-assisted duodenal perforation closure has become a safe, effective, and preferred approach for many patients.
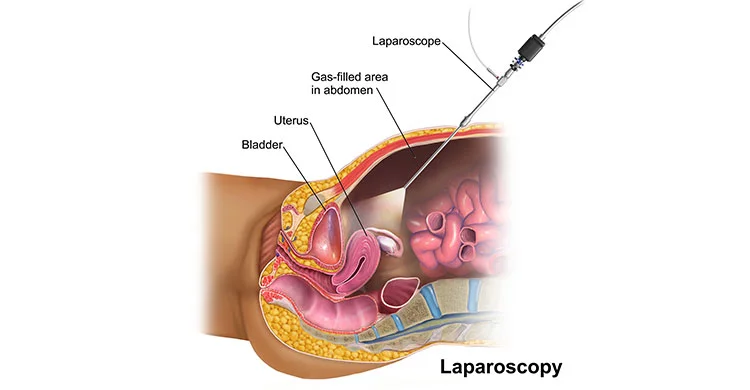
Laparoscopic closure involves inserting a laparoscope - a slender, tube-like instrument fitted with a camera - through small incisions in the abdomen. This enables the surgeon to visualize the perforation on a monitor and close it using specialized instruments, often with an omental patch (a piece of fatty tissue from the abdomen) to reinforce the repair. The laparoscopic technique allows for thorough cleaning (peritoneal lavage) of the abdomen, precise suturing, and minimal tissue trauma.
The major advantages of laparoscopic duodenal perforation closure include smaller incisions, less postoperative pain, reduced infection risk, shorter hospital stay, faster recovery, and improved cosmetic outcomes. This procedure has become a cornerstone in managing duodenal perforations caused by ulcers, trauma, or iatrogenic injuries, especially when patients are stable and present early after perforation.
Causes and Risk Factors of Duodenal Perforation
Duodenal perforation can arise from several causes, most commonly linked to peptic ulcer disease. It is a surgical emergency that requires immediate intervention to prevent severe infection, sepsis, and organ failure.
Common Causes Include:
-
Peptic Ulcer Disease (PUD): The most frequent cause, responsible for more than 80% of cases. Chronic ulcers erode the duodenal wall due to acid and pepsin exposure, often associated with Helicobacter pylori infection or long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs).
-
Trauma: Blunt or penetrating injuries to the abdomen can rupture the duodenal wall.
-
Iatrogenic Perforation: Occurs accidentally during medical procedures like endoscopy, ERCP (Endoscopic Retrograde Cholangiopancreatography), or surgery.
-
Foreign Body Ingestion: Sharp objects can pierce the gastrointestinal wall.
-
Ischemia: Reduced blood flow due to vascular compromise can cause tissue necrosis and perforation.
-
Malignancy: In rare cases, duodenal tumors or cancers may perforate spontaneously.
Risk Factors:
-
Chronic NSAID or steroid use.
-
H. pylori infection.
-
Smoking and excessive alcohol consumption.
-
Stress and irregular eating habits.
-
Advanced age and chronic diseases such as diabetes.
-
Previous history of peptic ulcers.
-
Delayed treatment of ulcer-related pain or bleeding.
Understanding these causes and risk factors is essential for early prevention, diagnosis, and timely surgical intervention.
Symptoms and Signs of Duodenal Perforation
Duodenal perforation presents with sudden, severe, and sharp abdominal pain - a classic symptom that often begins in the upper abdomen and spreads rapidly across the abdomen as peritonitis develops. The onset is abrupt and often described by patients as “the worst pain ever experienced.”
Common Symptoms:
-
Severe Abdominal Pain: Typically starts in the epigastric (upper central) region and spreads to the entire abdomen within hours.
-
Abdominal Tenderness and Rigidity: The abdomen becomes hard like a board due to inflammation of the peritoneum.
-
Nausea and Vomiting: Caused by irritation and infection.
-
Fever and Chills: Develop as the infection spreads.
-
Difficulty Breathing: Due to abdominal distension and diaphragmatic irritation.
-
Cessation of Bowel Movement: Paralytic ileus can occur, leading to bloating and inability to pass gas or stool.
-
Signs of Shock: In late cases, low blood pressure, rapid pulse, and confusion indicate sepsis or hypovolemia.
Physical Examination Findings:
-
Rebound tenderness and guarding.
-
Reduced or absent bowel sounds.
-
Pain aggravated by movement or coughing.
-
Signs of dehydration due to vomiting and infection.
Duodenal perforation is a surgical emergency, and immediate diagnosis and intervention are critical to prevent complications such as peritonitis, septicemia, and death.
Diagnosis of Duodenal Perforation
Prompt and accurate diagnosis of a duodenal perforation is vital for survival. The condition is primarily diagnosed through clinical examination and imaging studies.
Key Diagnostic Tools:
-
Clinical Assessment: A detailed medical history focusing on the onset of pain, medication use (especially NSAIDs), and previous ulcer symptoms. Physical examination usually reveals peritoneal signs and rigidity.
-
Laboratory Tests:
-
Elevated white blood cell count (WBC) indicating infection.
-
Abnormal liver or kidney function if sepsis has developed.
-
Electrolyte imbalances due to dehydration.
-
-
Radiological Imaging:
-
X-ray of the Abdomen/Chest: Often shows free air under the diaphragm, indicating perforation.
-
CT Scan of the Abdomen: The most accurate imaging tool; detects even small perforations, free gas, and fluid levels.
-
Ultrasound: May show free fluid but is less specific.
-
-
Diagnostic Laparoscopy: Sometimes, laparoscopy itself is used to confirm diagnosis when imaging is inconclusive and simultaneously repair the perforation.
Preoperative Evaluation:
Once diagnosed, patients undergo stabilization with fluids, antibiotics, and nasogastric decompression before surgery. Evaluating overall health and ensuring fitness for anesthesia are critical before proceeding with laparoscopic repair.
Treatment Options and the Laparoscopic Procedure
For stress urinary incontinence, laparoscopic colposuspension is an established minimally invasive surgical treatment alongside options like midurethral slings and bulking agents. Laparoscopic colposuspension lifts and supports the neck of the bladder and urethra using sutures placed via small abdominal incisions, offering long-term symptom relief with quicker recovery than open surgery.
Non-Surgical Management:
In very select cases with small, sealed perforations and minimal symptoms, non-surgical treatment (the Taylor method) may be attempted - involving IV fluids, antibiotics, nasogastric suction, and close monitoring. However, this approach carries a risk of recurrence or sepsis and is reserved for medically unfit patients.
Laparoscopy Duodenal Perforation Closure Procedure:
-
Anesthesia and Positioning: The procedure is performed under general anesthesia. The patient is positioned supine (lying flat), and small incisions are made to insert a laparoscope and surgical instruments.
-
Visualization and Exploration: The abdominal cavity is examined to locate the perforation and assess contamination.
-
Peritoneal Lavage: The surgeon irrigates (washes) the abdomen with sterile saline to remove infected fluid and debris.
-
Closure of Perforation: The perforation is closed using fine sutures (stitches), usually in two layers.
-
Omental Patch (Graham Patch): A piece of the omentum - a fatty tissue layer covering abdominal organs - is used to reinforce the repair.
-
Drain Placement: Drains may be left to remove residual fluid and prevent abscess formation.
-
Final Inspection and Closure: After confirming no leakage, instruments are removed, and small incisions are closed with absorbable sutures.
Benefits of the Laparoscopic Approach:
-
Minimal surgical trauma and faster recovery.
-
Reduced postoperative pain.
-
Lower risk of wound infection and hernias.
-
Early mobilization and return to work.
-
Shorter hospital stays and improved patient satisfaction.
In certain complex or late cases (large perforations or extensive contamination), conversion to open surgery may be necessary for safety.
Prevention and Management Before and After Surgery
Prevention and management before and after laparoscopic surgery for stress urinary incontinence-such as laparoscopic colposuspension-require careful patient preparation, infection prevention, vigilant post-op monitoring, and structured recovery plans to maximize outcomes and minimize complications.
Preoperative Management:
-
Fluid and Electrolyte Resuscitation: To correct dehydration and shock.
-
Nasogastric Decompression: To remove gastric contents and reduce leakage.
-
Broad-Spectrum Antibiotics: Started immediately to prevent infection.
-
Pain Relief and Proton Pump Inhibitors: To decrease stomach acid and reduce further damage.
-
Monitoring Vital Signs: Continuous monitoring ensures early detection of instability.
Postoperative Management:
-
Hospital Stay: Patients are monitored for signs of infection, leakage, or abscess formation.
-
Diet: Initially, patients are kept nil-by-mouth. Gradually, clear fluids are introduced, followed by soft foods.
-
Pain Management: Controlled with oral or IV analgesics.
-
Antibiotics and Acid Suppression: Continued to prevent infection and ulcer recurrence.
-
Early Ambulation: Encouraged to prevent clots and promote bowel function.
Prevention of Recurrence:
-
Eradicate H. pylori infection with a full antibiotic course.
-
Avoid NSAIDs, smoking, and alcohol.
-
Eat balanced, non-spicy meals and maintain a healthy weight.
-
Regular follow-up with endoscopy if ulcers were previously diagnosed.
Complications of Laparoscopy Duodenal Perforation Closure
Though the laparoscopic approach reduces risks, complications can still occur - especially in patients presenting late or with severe infection.
Possible Complications Include:
-
Anastomotic Leak: Leakage from the repaired site can cause peritonitis or abscess formation.
-
Infection: Wound infection or intra-abdominal abscess despite lavage.
-
Bleeding: From suture sites or damaged blood vessels.
-
Ileus: Temporary bowel paralysis causing bloating and nausea.
-
Sepsis: Due to residual infection or delayed treatment.
-
Pulmonary Complications: Pneumonia from prolonged bed rest or aspiration.
-
Conversion to Open Surgery: Required if the perforation is large or difficult to access laparoscopically.
Prevention: Skilled surgical technique, early diagnosis, and adherence to post-surgical care significantly reduce these risks.
Living with the Condition After Surgery
Living with the condition after laparoscopic surgery for stress urinary incontinence-especially after procedures like laparoscopic colposuspension-typically means substantial improvement in bladder control, daily confidence, and quality of life. Nonetheless, long-term success depends on healing, adherence to aftercare, monitoring for recurrence, and resuming activities sensibly.
Recovery Phase:
After surgery, most patients experience rapid recovery due to the minimally invasive nature of the procedure. They can often resume normal activities within 2-3 weeks, depending on their overall health and healing progress. A gradual increase in activity and a well-balanced diet are encouraged.
Diet and Lifestyle Changes:
-
Eat smaller, frequent meals to ease digestion.
-
Avoid spicy, fried, or highly acidic foods.
-
Stop smoking and alcohol consumption completely.
-
Limit caffeine intake.
-
Continue prescribed acid-suppressive medications (PPIs).
-
Stay hydrated and maintain a regular eating schedule.
Long-Term Outlook:
Patients who undergo successful laparoscopic repair typically regain full health. Preventing recurrence through H. pylori eradication, medication compliance, and lifestyle modification is key. Regular check-ups and endoscopy (if advised) help monitor healing and detect ulcers early. With proper care, the chances of re-perforation are minimal, and most patients lead normal, active, and pain-free lives.
Top 10 Frequently Asked Questions about Laparoscopic Duodenal Perforation Closure
1. What is a duodenal perforation?
A duodenal perforation is a hole or tear in the wall of the duodenum, which is the first part of the small intestine immediately after the stomach. It is often caused by conditions such as peptic ulcers, trauma, or rarely tumors. A perforation is a medical emergency because it can lead to leakage of stomach and intestinal contents into the abdominal cavity, causing infection (peritonitis).
2. What is laparoscopic duodenal perforation closure?
Laparoscopic duodenal perforation closure is a minimally invasive surgery performed to repair a hole in the duodenum. Using small abdominal incisions, a laparoscope (camera) and specialized instruments are inserted to locate the perforation, clean the surrounding area, and suture the hole closed. Sometimes a patch of tissue (such as omentum) is used to reinforce the repair.
This approach avoids a large open incision, leading to faster recovery, less post-operative pain, and shorter hospital stay.
3. Who is a candidate for laparoscopic closure?
Laparoscopic repair is typically recommended for patients who:
-
Present early (within 24 hours of perforation onset).
-
Are medically stable and can tolerate general anesthesia.
-
Do not have extensive contamination or severe infection that would necessitate open surgery.
Patients with delayed presentation, large perforations, or unstable condition may require traditional open surgery.
4. How is the surgery performed?
-
The patient is placed under general anesthesia.
-
Several small incisions are made in the abdomen. Carbon dioxide gas is used to inflate the abdominal cavity for better visualization.
-
A laparoscope and surgical instruments are inserted.
-
The perforation site is identified, cleaned of gastric and intestinal contents, and sutured closed.
-
Sometimes a patch of omentum (a fatty tissue layer) is placed over the repair for reinforcement.
-
The abdominal cavity is thoroughly washed (peritoneal lavage) to reduce infection risk, and incisions are closed.
5. What are the benefits of laparoscopic repair compared to open surgery?
-
Smaller incisions → less post-operative pain and quicker recovery.
-
Reduced hospital stay and faster return to normal diet and activity.
-
Better cosmetic outcome due to minimal scarring.
-
Enhanced visualization of the abdominal cavity, allowing thorough cleaning and assessment.
-
Reduced risk of wound-related complications such as infection or hernia.
6. What are the risks or potential complications?
Even though minimally invasive, laparoscopic repair carries some risks:
-
Leakage from the repair site, potentially requiring additional surgery.
-
Infection inside the abdominal cavity or at incision sites.
-
Bleeding from the repair site or surrounding tissues.
-
Injury to nearby organs, such as the stomach, pancreas, or intestines.
-
Conversion to open surgery if the perforation is large, contaminated, or difficult to access.
-
Post-operative ileus (temporary slowing of bowel function).
7. How long is the recovery period?
Recovery depends on patient condition, perforation size, and presence of infection:
-
Hospital stay is typically 3-7 days, sometimes longer if infection is severe.
-
Patients often start walking within a day after surgery.
-
Diet is gradually advanced from liquids to soft foods to normal diet as bowel function returns.
-
Full return to daily activities may take 4-6 weeks.
-
Post-operative antibiotics are usually prescribed to prevent or treat infection.
8. How is the risk of infection managed?
-
The abdominal cavity is washed thoroughly during surgery.
-
Broad-spectrum antibiotics are given before and after surgery.
-
Drainage tubes may be placed temporarily if there is significant contamination.
-
Close monitoring in hospital ensures early detection of any post-operative infections.
9. What lifestyle or dietary changes are recommended after surgery?
-
Begin with a liquid diet, then gradually progress to soft and
regular foods as tolerated.
-
Avoid heavy lifting or strenuous activity for several weeks to allow abdominal
healing.
-
Avoid smoking, alcohol, and NSAIDs, as these can increase the risk of ulcer
recurrence.
-
Maintain follow-up appointments to monitor healing and detect any complications
early.
10. What questions should I ask my surgeon before surgery?
-
Is laparoscopic repair the best approach for my perforation?
-
What is the expected success rate and complication risk in my case?
-
Will I need drainage tubes or post-operative ICU care?
-
How long will I stay in the hospital, and what is the expected recovery timeline?
-
Are there any dietary restrictions or lifestyle modifications I should follow
after surgery?
-
What signs or symptoms should I watch for after surgery to ensure proper healing?
Begin with a liquid diet, then gradually progress to soft and regular foods as tolerated.
Avoid heavy lifting or strenuous activity for several weeks to allow abdominal healing.
Avoid smoking, alcohol, and NSAIDs, as these can increase the risk of ulcer recurrence.
Maintain follow-up appointments to monitor healing and detect any complications early.
Is laparoscopic repair the best approach for my perforation?
What is the expected success rate and complication risk in my case?
Will I need drainage tubes or post-operative ICU care?
How long will I stay in the hospital, and what is the expected recovery timeline?
Are there any dietary restrictions or lifestyle modifications I should follow after surgery?
What signs or symptoms should I watch for after surgery to ensure proper healing?


