Introduction to Laparoscopy Repair of Diaphragmatic Hernia
A diaphragmatic hernia is a serious medical condition where the abdominal organs such as the stomach, intestines, liver, or spleen move upward into the chest cavity through an opening or weakness in the diaphragm - the muscular wall that separates the chest from the abdomen and plays an essential role in breathing. This abnormal movement can compress the lungs and heart, leading to breathing difficulties, chest discomfort, and digestive problems. In severe cases, it may even threaten life due to compromised lung function and oxygen supply.
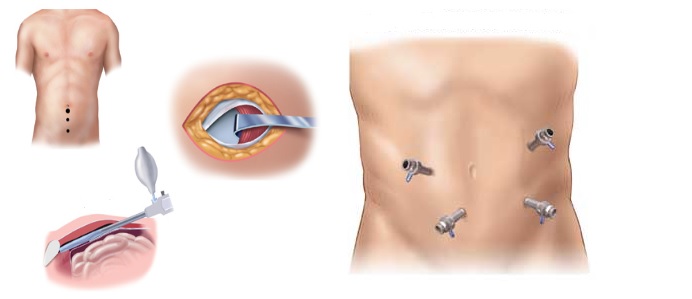
The Laparoscopy Repair of Diaphragmatic Hernia is a minimally invasive surgical procedure developed to correct this defect with precision, minimal trauma, and faster recovery compared to traditional open surgery. The procedure involves inserting a laparoscope (a narrow tube fitted with a light and high-resolution camera) through small incisions in the abdomen. Using specialized instruments, the surgeon gently returns the displaced organs to their normal positions and repairs the defect in the diaphragm using sutures or a surgical mesh to strengthen the weakened area.
This advanced laparoscopic technique has revolutionized the treatment of both congenital diaphragmatic hernias (present at birth) and acquired or traumatic hernias (developed after injury or surgery). Compared to older open surgical methods, laparoscopy offers several significant benefits, including smaller incisions, less postoperative pain, lower infection risk, shorter hospital stays, and quicker return to normal activities. It also allows for a clearer view of the diaphragm and abdominal cavity, enabling a more thorough repair. As surgical technology evolves, laparoscopic repair has become the standard of care for many patients suffering from this potentially life-threatening condition.
Causes and Risk Factors of Diaphragmatic Hernia
Diaphragmatic hernias can develop for a variety of reasons, depending on whether they are congenital (present from birth) or acquired (developed later in life). Understanding these causes and risk factors is crucial in identifying high-risk patients and ensuring early diagnosis and management.
Congenital Diaphragmatic Hernia (CDH):
This type of hernia occurs due to improper development of the diaphragm during fetal growth. A small defect or opening in the diaphragm allows abdominal organs to enter the chest cavity before birth. This condition is usually identified shortly after delivery, as it causes immediate breathing difficulties in newborns. The most common form of CDH is the Bochdalek hernia, located at the back and side of the diaphragm, while the Morgagni hernia occurs near the front.
Acquired or Traumatic Diaphragmatic Hernia:
In adults, diaphragmatic hernias typically develop after trauma or injury. These include:
-
Blunt trauma: Such as from road accidents or falls, which can tear the diaphragm.
-
Penetrating injuries: Caused by stab wounds or gunshots to the chest or abdomen.
-
Post-surgical complications: Especially after upper abdominal or thoracic surgeries.
-
Hiatal hernia: A specific type where part of the stomach pushes upward through the diaphragm's natural opening for the esophagus.
Risk Factors Include:
-
Obesity: Increases intra-abdominal pressure, contributing to herniation.
-
Chronic cough or heavy lifting: Repeated straining can weaken the diaphragm over time.
-
Pregnancy: The growing uterus increases pressure on the diaphragm.
-
Smoking and chronic lung disease: These affect tissue strength and increase pressure during coughing episodes.
-
Age-related muscle weakening: In older adults, tissues lose elasticity, making hernias more likely.
Identifying and managing these risks is vital for both prevention and early treatment, as an untreated diaphragmatic hernia can lead to organ strangulation, reduced lung function, and life-threatening complications.
Symptoms and Signs of Diaphragmatic Hernia
The symptoms of a diaphragmatic hernia vary greatly depending on the size of the hernia, the organs involved, and the speed of onset. In newborns with congenital diaphragmatic hernia, symptoms appear immediately after birth, whereas adults with acquired hernias may experience a gradual or sudden onset of symptoms.
Common Symptoms in Adults:
-
Difficulty Breathing: One of the earliest and most common signs, caused by compression of the lungs as abdominal organs press into the chest cavity.
-
Chest Pain or Discomfort: Often mistaken for cardiac pain, but typically worsens when bending or lying down.
-
Shortness of Breath: Especially noticeable after eating or physical exertion.
-
Digestive Symptoms: Including heartburn, bloating, nausea, or vomiting due to displacement of the stomach.
-
Feeling of Fullness: Even after small meals, due to the stomach's abnormal position.
-
Recurrent Respiratory Infections: Caused by reduced lung expansion and aspiration of stomach contents.
In Newborns and Infants:
-
Severe Respiratory Distress: Rapid, labored breathing or cyanosis (bluish skin) due to underdeveloped lungs.
-
Sunken Abdomen and Barrel Chest: As the intestines and stomach move upward.
-
Abnormal Heart Sounds: Due to the heart being pushed to one side.
If left untreated, a diaphragmatic hernia can lead to serious complications, such as bowel obstruction, lung collapse, and sepsis from organ strangulation. Prompt recognition and surgical correction are essential to prevent these outcomes.
Diagnosis of Diaphragmatic Hernia
Diagnosing a diaphragmatic hernia involves a combination of clinical evaluation and advanced imaging techniques. Early and accurate diagnosis is critical for planning the appropriate surgical approach.
Diagnostic Steps Include:
-
Physical Examination:
The physician listens for abnormal chest sounds, such as reduced breath sounds or the presence of bowel sounds in the chest, which suggest herniated organs. -
Chest X-ray:
This is often the first diagnostic test performed. It may show air-filled intestines or the stomach in the chest cavity, indicating a diaphragmatic defect. -
CT (Computed Tomography) Scan:
Provides highly detailed images of the diaphragm, revealing the exact size and location of the hernia. It is the gold standard for diagnosing diaphragmatic hernias in adults. -
MRI (Magnetic Resonance Imaging):
Offers precise soft-tissue detail, useful in complex cases or during pregnancy. -
Ultrasound:
Used especially in newborns or fetuses to detect congenital hernias during prenatal check-ups. -
Barium Swallow Test:
Helps visualize the movement of the stomach and esophagus, confirming hiatal hernias and reflux-related symptoms. -
Blood Tests and Lung Function Tests:
Assess overall health, oxygenation, and readiness for surgery.
Once the diagnosis is confirmed, the surgical team determines whether laparoscopic repair is appropriate, taking into account the patient's overall condition and the size of the hernia.
Treatment Options and Laparoscopic Surgical Procedure
For most diaphragmatic hernias, surgery is the only definitive treatment. Non-surgical options, such as medications or lifestyle adjustments, are only suitable for minor hiatal hernias or patients unfit for surgery.
Laparoscopy Repair of Diaphragmatic Hernia:
This modern technique is performed under general anesthesia and follows several carefully planned steps:
-
Small Incisions:
The surgeon makes 3-5 small keyhole incisions in the abdomen. -
Insertion of Laparoscope and Instruments:
The laparoscope provides a magnified, high-definition view of the diaphragm, chest, and abdominal organs. -
Reduction of Herniated Organs:
The displaced organs (stomach, intestines, liver, etc.) are gently moved back into the abdominal cavity. -
Repair of the Diaphragm:
The defect in the diaphragm is closed using sutures. For larger tears, a biologic or synthetic mesh is placed over the area to reinforce the repair. -
Inspection and Testing:
The surgeon checks for tension or leaks to ensure a secure closure. -
Closure of Incisions:
The small external incisions are closed with absorbable sutures, minimizing scarring.
Advantages of Laparoscopic Repair:
-
Less postoperative pain and discomfort.
-
Minimal blood loss during surgery.
-
Lower risk of wound infections.
-
Shorter hospital stay (typically 2-3 days).
-
Faster return to normal activities.
-
Better cosmetic results.
For complex or very large hernias, open surgery may still be necessary, but in most cases, laparoscopic repair offers excellent results with fewer complications.
Prevention and Management Before and After Surgery
Prevention and management before and after surgery for stress urinary incontinence (SUI)-such as midurethral sling, colposuspension, or bulking agent injection-are critical for minimizing complications and maximizing long-term success. They include medical optimization, infection prevention, patient education, careful post-op monitoring, and gradual return to activity.
Preoperative Management:
Before surgery, patients are carefully evaluated to ensure optimal outcomes. This includes:
-
Stabilizing breathing and oxygen levels in emergency cases.
-
Conducting all necessary imaging and laboratory tests.
-
Stopping blood-thinning medications before surgery.
-
Providing nutritional and respiratory support in infants or severely ill patients.
-
Detailed counseling on what to expect during recovery.
Postoperative Management:
-
Pain Control: Pain is mild and usually managed with oral painkillers.
-
Diet: Initially, patients consume clear liquids and progress to soft foods before returning to a regular diet.
-
Breathing Exercises: Deep breathing and physiotherapy improve lung expansion.
-
Early Mobilization: Walking soon after surgery prevents blood clots and promotes healing.
-
Regular Monitoring: Surgeons check for any signs of infection, fluid buildup, or hernia recurrence.
Prevention Tips for the Future:
-
Maintain a healthy weight to reduce abdominal pressure.
-
Avoid heavy lifting or straining.
-
Stop smoking to improve lung and tissue health.
-
Treat chronic cough or constipation promptly.
Effective perioperative care ensures faster recovery and long-lasting repair strength.
Complications of Laparoscopy Repair of Diaphragmatic Hernia
While laparoscopic repair is safe and effective, potential complications can occasionally occur. However, these are rare when performed by experienced surgeons.
Possible Complications Include:
-
Bleeding or Infection: Minor and typically resolved with medication.
-
Hernia Recurrence: Rare but may occur if the repair weakens over time.
-
Organ Injury: Minimal risk to lungs, liver, or intestines during surgery.
-
Gas-Related Shoulder Pain: Due to carbon dioxide used in the procedure; temporary and resolves within days.
-
Respiratory Complications: Particularly in patients with pre-existing lung disease.
-
Mesh Reactions: In rare cases, mild inflammation around synthetic mesh may occur.
Most complications are mild and easily managed, and the overall success rate of laparoscopic diaphragmatic hernia repair is over 95%.
Living with the Condition After Surgery
After successful laparoscopic repair, patients typically experience significant improvement in breathing, digestion, and overall well-being. The lungs re-expand, the heart returns to its normal position, and gastrointestinal symptoms subside.
Recovery and Lifestyle:
-
Most patients return to normal activities within 2-4 weeks.
-
Light exercise such as walking or stretching helps regain stamina.
-
A healthy, balanced diet supports recovery and prevents reflux.
-
Avoiding strenuous activities and heavy lifting for at least six weeks is recommended.
-
Long-term follow-up with the surgeon ensures proper healing.
Quality of Life:
Patients report dramatic relief from symptoms such as shortness of breath, heartburn, and chest discomfort. Infants with congenital repairs often show normal growth and development after surgery. With good surgical outcomes and appropriate lifestyle habits, recurrence is rare, and most patients lead a normal, active, and unrestricted life.
Top 10 Frequently Asked Questions about Laparoscopy Repair Of Diaphragmatic Hernia
1. What is a diaphragmatic hernia?
A diaphragmatic hernia occurs when there is a defect or weakness in the diaphragm, the muscle that separates the chest and abdominal cavities, allowing abdominal organs such as the stomach, intestines, or liver to move into the chest. This can cause breathing difficulties, chest discomfort, or digestive symptoms. Diaphragmatic hernias can be congenital (present at birth) or acquired, often due to trauma or increased abdominal pressure.
2. What is laparoscopic repair of a diaphragmatic hernia?
Laparoscopic repair is a minimally invasive surgical procedure to fix a diaphragmatic hernia. Small incisions are made in the abdomen to insert a camera (laparoscope) and instruments. The surgeon pushes the displaced organs back into the abdominal cavity and repairs the diaphragmatic defect, often using sutures or a mesh patch for reinforcement. This approach reduces recovery time, post-operative pain, and visible scarring compared to open surgery.
3. Who is a candidate for this surgery?
Laparoscopic diaphragmatic hernia repair is recommended for patients who:
-
Have symptomatic hernias causing pain, digestive problems, or breathing difficulties.
-
Are medically stable and fit for general anesthesia.
-
Have hernias that are suitable for laparoscopic access, typically not extremely large or complex.
Patients with very large hernias, severe adhesions from prior surgeries, or unstable conditions may require open surgery instead.
4. How is the procedure performed?
-
The patient is placed under general anesthesia.
-
Several small incisions are made in the abdomen for a laparoscope and surgical instruments.
-
The abdominal cavity is inflated with carbon dioxide gas for better visualization.
-
Displaced organs are carefully repositioned into the abdominal cavity.
-
The diaphragmatic defect is closed using sutures or reinforced with a surgical mesh if needed.
-
The surgical area is checked for bleeding or other complications, and the small incisions are closed.
The procedure typically lasts 1-3 hours depending on hernia size and complexity.
5. What are the benefits of laparoscopic repair?
-
Minimally invasive: smaller incisions, less post-operative pain, and quicker recovery.
-
Reduced hospital stay compared to open surgery.
-
Faster return to normal activities and work.
-
Better cosmetic outcome due to minimal scarring.
-
Improved visualization of the hernia and surrounding structures during surgery.
-
Lower risk of wound complications, such as infections or hernias at incision sites.
6. What are the risks or complications?
While generally safe, risks include:
-
Bleeding or injury to surrounding organs (stomach, intestines, liver, lungs).
-
Infection at the incision sites or internally.
-
Recurrence of the hernia if the repair is not strong or if risk factors persist.
-
Post-operative pain, bloating, or difficulty breathing.
-
Anesthesia-related complications.
-
Rarely, complications related to mesh (if used), such as infection or erosion.
7. How long is the recovery period?
-
Hospital stay is usually 2-5 days, depending on the complexity of the hernia and patient condition.
-
Light activity and walking are encouraged soon after surgery.
-
Patients may resume normal activities in 3-6 weeks.
-
Diet usually progresses from liquids to soft foods to a regular diet as tolerated.
-
Heavy lifting and strenuous exercise should be avoided for several weeks to ensure proper healing.
8. Will I need any lifestyle changes after surgery?
-
Maintain a healthy weight to reduce abdominal pressure and prevent recurrence.
-
Avoid activities that involve heavy lifting or straining during the recovery period.
-
Follow dietary recommendations to prevent bloating or constipation.
-
Stop smoking if applicable, as it can affect healing and lung function.
-
Attend follow-up appointments to monitor recovery and detect any recurrence early.
9. How effective is laparoscopic repair?
-
Most patients experience significant symptom relief, including improved breathing and reduced gastrointestinal discomfort.
-
Recurrence rates are low when the repair is properly performed and reinforced, especially with mesh.
-
Long-term outcomes are excellent, with the majority of patients returning to normal daily activities without limitations.
10. What questions should I ask my surgeon before surgery?
-
Is laparoscopic repair suitable for my type and size of hernia?
-
What is the likelihood of hernia recurrence in my case?
-
Will a mesh be used for reinforcement, and what are the associated risks?
-
How long will I stay in the hospital, and what is the expected recovery timeline?
-
What dietary or activity restrictions will I need after surgery?
-
What complications should I watch for after discharge?
-
Are there alternative treatment options if laparoscopic repair is not feasible?


