Introduction to Laryngectomy
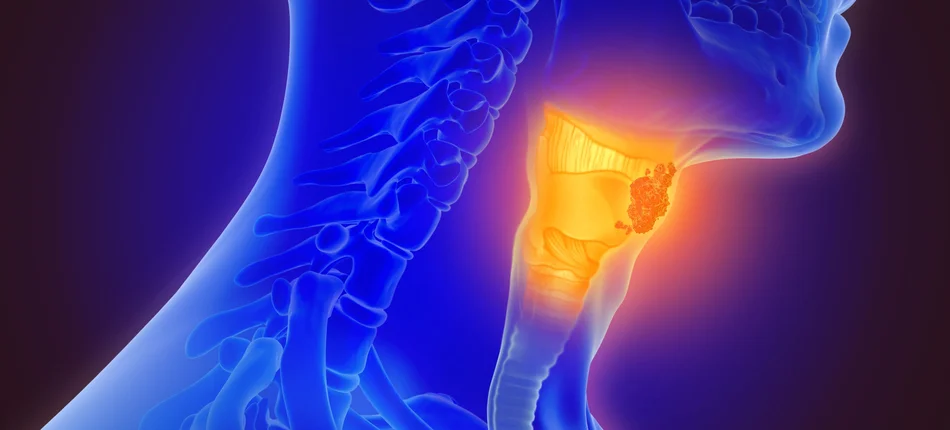
A laryngectomy is a major surgical procedure in which part or all of the larynx (voice box) is removed. The larynx, located in the neck just above the trachea (windpipe), plays a vital role in breathing, swallowing, and producing speech. It houses the vocal cords, which vibrate to create sound when air passes through. When diseases such as advanced laryngeal cancer, severe trauma, or chronic infection damage the larynx beyond repair, surgical removal becomes necessary to save the patient's life and prevent further complications.
In a total laryngectomy, the entire larynx is removed, resulting in a permanent separation between the airway and the mouth, nose, and esophagus. A stoma (permanent breathing hole) is created at the base of the neck to allow direct passage of air into the lungs. In contrast, a partial laryngectomy removes only part of the larynx, preserving some voice function and natural airway continuity. Advances in modern surgical techniques and postoperative rehabilitation have made this life-saving surgery safer and more manageable than ever before.
Laryngectomy is not merely a surgical procedure; it is a transformational process that demands physical, emotional, and psychological adaptation. Patients undergo profound changes in speech, breathing, and swallowing. However, with comprehensive medical care, speech therapy, and emotional support, individuals can regain communication, maintain a good quality of life, and return to normal social functioning.
Causes and Risk Factors of Laryngectomy
The primary reason for performing a laryngectomy is laryngeal cancer, which typically develops from the mucous membranes lining the larynx. Prolonged exposure to irritants and toxins leads to cellular mutations, resulting in malignant growths that obstruct the airway or invade deeper tissues. When radiation therapy, chemotherapy, or partial surgery cannot control the disease, a total laryngectomy becomes the best option for survival.
Common Causes Include:
-
Laryngeal or Hypopharyngeal Cancer: The most common cause, often in the advanced stage, where the tumor has spread to nearby tissues or recurred after previous treatments.
-
Severe Trauma: Penetrating or blunt injuries to the neck that destroy the larynx and compromise breathing.
-
Chronic Infections or Radiation Damage: Rarely, infections or previous cancer treatments may cause irreversible tissue damage, necessitating surgical removal.
-
Extensive Laryngeal Stenosis: Severe narrowing of the airway unresponsive to other treatments.
Major Risk Factors for Laryngeal Cancer:
-
Tobacco Use: The single biggest risk factor. Both smoking and chewing tobacco significantly increase the risk of cancer in the throat and larynx.
-
Alcohol Consumption: Heavy drinking, especially combined with smoking, multiplies the risk.
-
Occupational Exposures: Long-term exposure to asbestos, wood dust, paint fumes, and certain chemicals can cause chronic irritation of the larynx.
-
Viral Infections: Human papillomavirus (HPV) has been linked to some throat cancers.
-
Poor Nutrition and Reflux Disease: Deficiency of essential vitamins, particularly vitamin A, and untreated gastroesophageal reflux disease (GERD) may contribute to chronic irritation.
-
Age and Gender: Men over the age of 55 are most commonly affected.
Understanding these causes and risk factors is key in prevention and early intervention - steps that can often help avoid the need for such a radical surgery.
Symptoms and Signs Leading to Laryngectomy
Laryngeal cancer and other serious laryngeal diseases progress gradually, and early signs are often mistaken for minor throat conditions. Recognizing these symptoms early can allow for timely treatment before surgery becomes necessary.
Common Symptoms Include:
-
Persistent Hoarseness or Voice Change: The earliest and most frequent symptom of laryngeal cancer.
-
Throat Pain or Soreness: Pain that doesn't improve with standard medication.
-
Difficulty Swallowing (Dysphagia): A feeling of food sticking in the throat or pain during swallowing.
-
Chronic Cough: Especially when accompanied by blood (hemoptysis).
-
Lump in the Neck: Enlarged lymph nodes often indicate cancer spread.
-
Breathing Difficulty (Stridor): Wheezing or noisy breathing due to airway narrowing.
-
Unexplained Weight Loss or Fatigue: A sign of advanced disease or systemic cancer spread.
If these symptoms persist for more than two weeks, especially in people with smoking or alcohol history, medical evaluation is urgent. Failure to treat early-stage laryngeal cancer may lead to tumor expansion, airway blockage, and the eventual need for a total laryngectomy.
Diagnosis and Preoperative Evaluation
Diagnosing laryngeal disease involves a series of detailed evaluations by an ENT (Ear, Nose, and Throat) specialist, oncologist, and radiologist. The goal is to confirm the presence, type, and stage of the disease and assess whether organ-preserving treatment is possible.
Diagnostic Steps Include:
-
Physical Examination: A doctor examines the neck and throat for visible lesions or palpable masses.
-
Laryngoscopy: A thin, flexible camera called a laryngoscope is inserted through the nose or mouth to directly visualize the vocal cords and surrounding structures.
-
Biopsy: A tissue sample from the lesion is taken during laryngoscopy and sent for histopathological analysis to confirm cancer and determine its type.
-
Imaging Studies:
-
CT (Computed Tomography) or MRI (Magnetic Resonance Imaging) scans evaluate the size and spread of the tumor.
-
PET (Positron Emission Tomography) scans detect metastasis to distant organs.
-
-
Staging: Based on the tumor size (T), lymph node involvement (N), and metastasis (M).
-
Preoperative Evaluation: Includes cardiopulmonary testing, nutritional assessment, and anesthetic clearance.
-
Speech and Psychological Assessment: Patients receive counseling regarding expected changes in speech and breathing.
A thorough diagnostic process ensures that surgery is planned with precision, minimizing complications and optimizing recovery outcomes.
Treatment Options for Laryngectomy
Treatment options for laryngectomy-most commonly performed for laryngeal cancer, but also for severe injury, paralysis, or necrosis-are tailored according to tumor size, location, and preservation of function. The mainstay is surgery, with several types of laryngectomy and adjunct approaches available.
Non-Surgical Treatments:
In early-stage laryngeal cancer, radiation therapy or chemoradiation may be curative. Minimally invasive endoscopic or laser surgeries can also remove smaller tumors while preserving voice. However, when the cancer is extensive, recurrent, or unresponsive to other treatments, total laryngectomy remains the definitive life-saving option.
Surgical Procedure:
A total laryngectomy involves the removal of the entire larynx, along with nearby lymph nodes if cancer has spread. The trachea (windpipe) is then brought forward and connected to a permanent opening (stoma) in the neck for breathing. The pharynx is reconstructed to allow swallowing, and the wound is closed meticulously to prevent leaks or infection. The surgery typically lasts 4-6 hours under general anesthesia.
Rehabilitation and Recovery:
Post-surgery, patients are cared for in an intensive or high-dependency unit. Initially, feeding occurs through a nasogastric or PEG tube to allow healing. Once stable, speech and swallowing rehabilitation begins. Speech therapy focuses on teaching alternative ways to speak using an electrolarynx, esophageal speech, or a tracheoesophageal puncture (TEP) with a voice prosthesis. These modern rehabilitation tools enable patients to regain near-normal speech.
Prevention and Management of Laryngectomy
Prevention and management for laryngectomy focus on thorough patient preparation, meticulous surgical and wound care, infection prevention, airway (stoma) management, and multidisciplinary rehabilitation. The goal is a safe recovery and optimal long-term function.
Prevention:
The most effective prevention strategies focus on reducing risk factors and promoting early detection.
-
Quit Smoking: Eliminating tobacco is the most powerful preventive step.
-
Limit Alcohol Consumption: Especially when combined with smoking, alcohol greatly increases cancer risk.
-
Healthy Diet: A diet rich in fruits and vegetables strengthens immunity and mucosal health.
-
Protective Measures at Work: Use of masks and avoidance of chemical inhalants.
-
Regular ENT Check-ups: Particularly for individuals with persistent voice changes or throat discomfort.
Management Before and After Surgery:
Preoperative Management includes nutritional optimization, airway evaluation, and psychological preparation. Patients and their families are educated about living with a stoma and the upcoming lifestyle adjustments.
Postoperative Management focuses on recovery and adaptation:
-
Maintaining stoma hygiene and preventing infection.
-
Ensuring adequate hydration and humidification of inhaled air.
-
Gradually reintroducing oral feeding.
-
Regular physiotherapy and speech training.
-
Lifelong follow-up to detect recurrence or complications early.
Complications of Laryngectomy
Despite significant advancements, laryngectomy remains a complex surgery with potential complications that require careful management.
Early (Postoperative) Complications:
-
Bleeding or Hematoma Formation: Controlled through surgical drainage.
-
Infection: Prevented with antibiotics and wound care.
-
Pharyngocutaneous Fistula: Leakage of saliva from the reconstructed pharynx through the neck wound; usually managed conservatively.
-
Swelling and Airway Obstruction: Immediate medical attention required.
Late (Long-term) Complications:
-
Loss of Natural Voice: Permanent, but alternatives like voice prostheses are available.
-
Swallowing Difficulties: Managed with swallowing therapy.
-
Altered Sense of Smell and Taste: Due to separation of the airway from the nasal passages.
-
Stoma Issues: Narrowing, crusting, or infection; prevented with proper care.
-
Psychological Challenges: Anxiety, depression, or social withdrawal are common and require counseling.
Most patients recover well and adapt effectively with consistent rehabilitation and support from a multidisciplinary medical team.
Living with the Condition After Laryngectomy
Life after laryngectomy requires adjustment, but with the right support and training, patients can live full, independent, and meaningful lives.
Breathing and Stoma Care:
The neck stoma becomes the permanent breathing passage. Patients learn to clean it regularly, use stoma filters or humidifiers to moisten inhaled air, and protect it from dust, water, and infection.
Speech and Communication:
Modern rehabilitation allows patients to speak again using:
-
Electrolarynx: A handheld device that creates vibrations, producing a mechanical voice.
-
Esophageal Speech: Using the upper esophagus to create sound.
-
Tracheoesophageal Puncture (TEP): A surgically created valve between the trachea and esophagus, allowing speech that sounds more natural.
Swallowing and Nutrition:
Most patients can return to a normal diet after healing, though they must eat slowly and avoid very dry or crumbly foods. Nutritional guidance ensures proper weight and energy maintenance.
Emotional and Social Life:
Counseling and support groups play a key role in helping patients rebuild confidence and reintegrate socially. Many patients return to work, travel, and resume normal activities within months of surgery.
With ongoing medical follow-up, speech therapy, and emotional resilience, individuals who undergo laryngectomy can thrive and continue to lead productive, fulfilling lives.
Top 10 Frequently Asked Questions about Laryngectomy
1. What is a laryngectomy?
A laryngectomy is a surgical procedure in which the larynx (voice box) is partially or completely removed. It is most commonly performed to treat laryngeal cancer or severe trauma affecting the larynx. After a total laryngectomy, the airway is permanently diverted through a stoma (an opening in the neck), allowing breathing but preventing normal voice production.
2. Why is laryngectomy performed?
Laryngectomy is indicated for patients who have:
-
Laryngeal cancer that cannot be treated with radiation or chemotherapy alone.
-
Severe trauma or injury to the larynx.
-
Persistent airway obstruction or dysfunction of the larynx.
The goal is to remove the diseased or damaged tissue, restore breathing, and, if possible, preserve or restore communication through speech rehabilitation.
3. What are the types of laryngectomy?
-
Total laryngectomy: Complete removal of the larynx, including vocal cords, leaving the patient to breathe through a permanent stoma.
-
Partial laryngectomy: Only part of the larynx is removed, potentially preserving some natural voice and airway function.
-
Supraglottic laryngectomy: Removal of structures above the vocal cords, often used for smaller tumors.
The type depends on tumor size, location, and the patient's overall health.
4. How is the surgery performed?
-
The patient is placed under general anesthesia.
-
The surgeon makes an incision in the neck and carefully removes the affected portion of the larynx.
-
For total laryngectomy, a stoma is created for permanent breathing.
-
Surrounding tissues, lymph nodes, and affected areas may also be removed to ensure complete treatment of cancer.
-
Reconstruction may involve tissue flaps or prosthetic devices to assist swallowing or speech.
The procedure typically lasts 3-6 hours, depending on complexity and extent of disease.
5. How will breathing and speaking change after laryngectomy?
-
Breathing will occur through the stoma in the neck instead of the mouth and nose.
-
Normal speech using the vocal cords is no longer possible after total laryngectomy.
-
Voice can be restored through speech rehabilitation, including:
-
Esophageal speech: Producing sound by swallowing air into the esophagus.
-
Electrolarynx: A handheld device that generates vibrations to produce artificial speech.
-
Tracheoesophageal puncture (TEP) and voice prosthesis: A device inserted between the trachea and esophagus to allow voice production.
-
6. What are the risks and complications?
Laryngectomy is a major surgery with potential risks, including:
-
Infection at the surgical site.
-
Bleeding or hematoma formation.
-
Difficulty swallowing or aspiration during recovery.
-
Stoma-related complications, such as narrowing or infection.
-
Fistula formation (abnormal connection between trachea and esophagus).
-
Changes in smell, taste, and sense of airflow through the nose.
-
Permanent loss of natural voice in total laryngectomy.
7. How long is the recovery period?
-
Hospital stay is usually 1-2 weeks, depending on healing and any complications.
-
Patients learn to care for the stoma, manage breathing, and use temporary feeding methods if needed.
-
Full recovery, including adaptation to voice rehabilitation and stoma care, may take several weeks to months.
-
Regular follow-up is critical to monitor for cancer recurrence and manage rehabilitation.
8. What lifestyle changes are necessary after laryngectomy?
-
Stoma care: Cleaning, humidifying, and protecting the stoma is essential to prevent infections.
-
Avoid swimming and dusty or smoky environments without protection.
-
Nutrition may need modification initially, especially if swallowing is affected.
-
Smoking cessation is strongly recommended to prevent recurrence of cancer.
-
Psychological support may be needed to adjust to changes in breathing, speech, and appearance.
9. What rehabilitation options are available?
-
Speech therapy: Training in esophageal speech or use of an electrolarynx.
-
Voice prosthesis (TEP): Allows near-natural speech by directing airflow from the trachea to the esophagus.
-
Physical therapy: Helps maintain neck mobility and posture.
-
Psychological support: Coping with body image, communication changes, and social interactions.
10. What questions should I ask my surgeon before undergoing laryngectomy?
-
What type of laryngectomy is recommended in my case, and why?
-
What changes in breathing and speech should I expect?
-
How long will the hospital stay and recovery period be?
-
What are the potential risks and complications for my situation?
-
How will my speech be rehabilitated?
-
What lifestyle modifications will I need post-surgery?
-
Will I need additional treatments, such as chemotherapy or radiation?
-
How often will I need follow-up after surgery?


