Introduction to Limbal Relaxing Incision
Limbal Relaxing Incision (LRI) is a highly refined ophthalmic surgical technique used primarily to correct corneal astigmatism, one of the most common refractive errors affecting the human eye. In astigmatism, the cornea - which should ideally be round and evenly curved - becomes more oval-shaped, leading to blurred or distorted vision at all distances. This uneven curvature prevents light rays from focusing sharply on the retina, causing visual discomfort, strain, and reduced clarity.
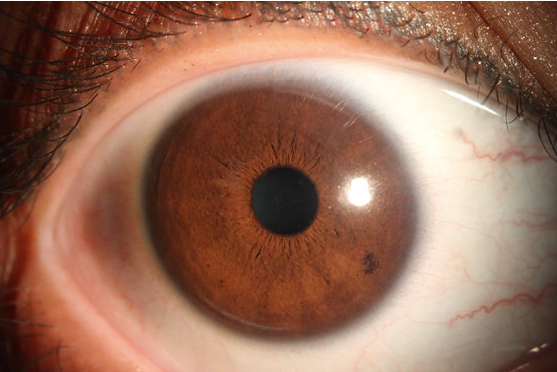
LRI corrects this irregularity by making one or more microscopic arc-shaped incisions at the limbus, which is the junction between the cornea and the sclera (the white part of the eye). These incisions are placed precisely along the steepest meridian of the cornea, which relaxes the corneal curvature in that area and helps it adopt a more regular, spherical shape. As a result, light entering the eye focuses more uniformly, significantly improving vision quality and reducing dependency on glasses or contact lenses.
The procedure is minimally invasive, safe, and quick - typically performed under topical anesthesia in an outpatient setting. It can be done as a standalone surgery to correct mild to moderate astigmatism, or more commonly, it is combined with cataract surgery to address pre-existing astigmatism while replacing the cloudy lens. For patients undergoing cataract surgery, the addition of LRI ensures sharper postoperative vision and can minimize or even eliminate the need for corrective eyewear afterward.
What makes the LRI especially appealing is its customizable precision. Modern ophthalmic advancements, including computer-guided planning and femtosecond laser-assisted techniques, have made it possible to perform LRIs with unmatched accuracy. Every incision can be customized based on corneal topography, thickness, and axis of astigmatism, leading to consistently excellent results and faster recovery.
In essence, the Limbal Relaxing Incision represents a blend of surgical finesse and optical science - a simple yet effective method that enhances visual outcomes while preserving the eye's natural anatomy.
Causes and Risk Factors Necessitating Limbal Relaxing Incision
While Limbal Relaxing Incision is not a treatment for a disease, it addresses astigmatism, which stems from irregularities in the corneal shape. To understand why this surgery is performed, one must understand the causes of astigmatism and the factors that influence surgical planning and risk.
1. Causes of Astigmatism
-
Congenital or Natural Astigmatism:
Most people are born with some degree of astigmatism due to slight variations in corneal curvature. When the curvature difference between the two main meridians of the cornea becomes significant, vision becomes distorted, warranting correction. -
Post-Surgical Astigmatism:
After procedures such as cataract surgery, corneal transplants, or LASIK, the corneal surface may change shape due to healing responses or incision placements, leading to astigmatism. LRI is an excellent corrective measure in these cases. -
Age-Related Changes:
Over time, natural alterations in the cornea's structure may cause or worsen astigmatism, particularly after the age of 40. -
Corneal Trauma or Infection:
Injury or infection can cause scarring or uneven healing, resulting in localized corneal irregularities. -
Lens-Induced Astigmatism:
Sometimes, internal lens changes (as in cataracts) alter the eye's focusing power, contributing to total astigmatism. LRI corrects the corneal component while cataract surgery addresses the lens component.
2. Risk Factors and Surgical Considerations
Although LRI is generally safe and effective, certain factors must be evaluated to ensure the best results and minimize risks:
-
Corneal Thickness and Shape:
A cornea that is too thin or irregularly shaped may not be suitable for LRI. -
Severity of Astigmatism:
LRI is most effective for mild to moderate astigmatism (up to about 3 diopters). Higher degrees might require laser refractive surgery or toric intraocular lenses. -
Healing Response:
Each eye heals differently. Some may experience regression of effect as the cornea remodels naturally over time. -
Dry Eye Disease:
Pre-existing dry eye can worsen temporarily after LRI and should be managed before surgery. -
Surgeon Expertise:
Precision in incision placement, arc length, and depth is critical; errors can lead to under- or over-correction.
When performed with careful preoperative evaluation and surgical precision, LRI has an excellent success rate and very low complication incidence.
Symptoms and Signs Suggesting the Need for Limbal Relaxing Incision
Astigmatism manifests through a wide range of visual symptoms that often interfere with daily activities. The symptoms may appear mild initially but can worsen over time or after eye surgery. The most common indicators that may lead a patient to consider Limbal Relaxing Incision include:
-
Blurry or Distorted Vision:
Vision appears stretched or smeared both at near and distance, making reading and driving difficult. -
Double Vision or “Ghosting”:
Multiple overlapping images of a single object, especially noticeable at night or under dim light. -
Eye Strain and Fatigue:
Because the eyes constantly attempt to compensate for uneven focus, prolonged use leads to discomfort and fatigue. -
Headaches:
Persistent headaches, especially after visual tasks, may result from constant eye strain. -
Difficulty with Night Vision:
Astigmatism causes light to scatter within the eye, producing glare, halos, or starbursts around lights. -
Frustration with Glasses or Contact Lenses:
Some patients find optical correction insufficient or uncomfortable, particularly if astigmatism is irregular.
For cataract patients, the presence of even mild astigmatism can significantly affect post-surgery vision quality. Thus, combining LRI with cataract surgery offers a smoother visual recovery and better clarity without dependence on glasses.
Diagnosis and Preoperative Evaluation Before Limbal Relaxing Incision
Before proceeding with LRI, a comprehensive diagnostic evaluation ensures that the procedure is both safe and appropriately tailored to the individual's eye anatomy. Each eye is unique - even two eyes in the same person may require different incision parameters.
1. Visual Acuity and Refraction Testing
The process begins with measuring the patient's vision with and without correction to assess the degree and type of astigmatism. This helps determine the expected benefit from surgical correction.
2. Corneal Topography and Tomography
Advanced imaging technologies like corneal topography create a detailed, color-coded 3D map of the cornea's shape. It identifies steep and flat meridians, asymmetries, and any irregularities. This data is essential for calculating the exact axis and length of the limbal incisions.
3. Keratometry
Keratometry measures corneal curvature in diopters and provides information about corneal steepness and symmetry.
4. Pachymetry
This test measures corneal thickness - a critical factor that determines incision depth. Adequate thickness ensures structural safety during surgery.
5. Tear Film and Surface Evaluation
A healthy ocular surface promotes proper healing. Patients with dryness or inflammation receive pre-treatment before LRI to optimize surgical results.
6. Biometry and Cataract Planning
For patients combining LRI with cataract surgery, lens measurements are taken to calculate intraocular lens (IOL) power. The surgeon then integrates both treatments into one surgical plan.
7. Personalized Surgical Planning
Based on the collected data, a nomogram (a surgical calculation chart) determines the incision arc, depth, and location. This ensures highly individualized correction.
Modern LRI techniques often use computerized planning systems and laser-guided technology, making every incision precise and reproducible.
Treatment Procedure: How Limbal Relaxing Incision is Performed
LRI is a straightforward and efficient surgical procedure performed under topical anesthesia. It requires no hospitalization and typically takes less than 15 minutes per eye. The steps of the surgery are as follows:
1. Preparation
The patient's eye is numbed using anesthetic eye drops. The eye and surrounding skin are sterilized. The corneal meridian requiring correction is identified and marked.
2. Creating the Incisions
Using a precisely calibrated blade or a femtosecond laser, the surgeon makes one or two arc-shaped incisions at the outer edge of the cornea (the limbus). The incisions typically extend through 80-90% of corneal depth, strategically weakening the steep axis.
3. Relaxation of Corneal Curvature
Once the incisions are made, the cornea's natural elasticity redistributes, flattening the steep curvature and making the corneal shape more symmetrical.
4. Femtosecond Laser-Assisted LRI (FL-LRI)
In modern ophthalmology, the femtosecond laser has replaced manual blades in many centers. The laser allows sub-micrometer precision, ensuring uniform depth, shape, and position of the incisions. This technology minimizes risks such as over-penetration and enhances predictability.
5. Post-Surgical Care
No sutures are needed. The patient receives antibiotic and anti-inflammatory eye drops to prevent infection and reduce inflammation. Vision often begins improving within a few days, stabilizing over 4-6 weeks.
This technique is often combined with cataract or lens replacement surgery, eliminating pre-existing astigmatism and optimizing final vision quality. When performed correctly, patients experience significant improvement in clarity, focus, and contrast sensitivity.
Prevention and Management: Before and After Surgery
Preoperative Measures
Before undergoing LRI, patients should follow these guidelines:
-
Avoid contact lenses for several days before surgery (as advised by the doctor).
-
Maintain clean eyelids and lashes; avoid makeup or lotions before surgery.
-
Treat any eye infections, allergies, or inflammation.
-
Discuss medical history, medications, and supplements with the surgeon.
-
Stay hydrated and avoid eye rubbing before and after surgery.
Postoperative Care
Proper care after surgery ensures rapid recovery and lasting results:
-
Use prescribed antibiotic and steroid drops to prevent infection and inflammation.
-
Apply lubricating drops to relieve dryness or irritation.
-
Avoid rubbing the eyes, swimming, and strenuous activities for at least two weeks.
-
Protect the eyes from dust, wind, and UV light by wearing sunglasses outdoors.
-
Attend all scheduled follow-up appointments for monitoring.
By adhering to these precautions, patients can expect a smooth recovery and stable vision improvement without complications.
Complications of Limbal Relaxing Incision
LRI is one of the safest and most predictable surgical techniques for correcting astigmatism, but like all medical procedures, it carries some potential complications:
-
Under or Over-Correction:
The effect of the incisions may vary slightly; some residual astigmatism may remain or over-flattening may occur. -
Regression:
Mild regression of the effect can happen as the cornea heals and remodels naturally. -
Infection or Inflammation:
Rare, but when it occurs, it can be easily managed with antibiotics and corticosteroids. -
Irregular Astigmatism:
Uneven healing may lead to irregular vision, though this is very uncommon. -
Dry Eye or Discomfort:
Transient dryness or irritation may occur during the initial healing period. -
Glare or Light Sensitivity:
Some patients experience glare under bright lights for a few weeks after surgery.
Despite these rare risks, LRI's overall success rate is extremely high, and severe complications are almost unheard of with current techniques.
Living After Limbal Relaxing Incision
After the recovery period, most patients experience significantly improved visual clarity and comfort. Many report that tasks like reading, computer work, and driving - especially at night - become noticeably easier.
LRI offers a long-lasting solution for astigmatism correction, although subtle changes in corneal shape may continue over time due to aging. The majority of patients remain free from glasses for distance vision and may only require mild correction for reading as they age.
Patients who underwent LRI along with cataract surgery enjoy the greatest benefit - not only improved clarity but also the ability to live largely free of glasses or contact lenses.
Maintaining a healthy eye lifestyle post-surgery is important. Using lubricating drops as needed, wearing sunglasses in bright sunlight, and scheduling regular eye check-ups ensure that the results remain stable and the eyes stay healthy for years.
Top 10 Frequently Asked Questions about Limbal Relaxing Incision
1. What is a Limbal Relaxing Incision (LRI)?
Limbal Relaxing Incisions are small, partial-thickness cuts made at or near the limbus (the border of the cornea and the white of the eye) to reduce or correct corneal astigmatism. These incisions “relax” the steeper curvatures of the cornea so that the overall shape becomes more regular, which improves vision by reducing the corneal cylinder (astigmatism).
2. Why is an LRI performed?
This procedure is typically done when a patient has mild to moderate astigmatism (often less than about 3 diopters) and wants to reduce dependence on glasses or contacts, or is undergoing cataract surgery and wishes to correct astigmatism at the same time. The goal is improved uncorrected vision and better refractive outcomes by making the cornea more regular.
3. How is an LRI performed?
-
Using topical anesthetic drops, the surgeon marks the steep corneal axis where the incision should be placed.
-
A guarded blade or laser is used to create the arcuate or limbal incision(s) at the outer corneal edge.
-
The depth, length, and location of the incision are determined based on the patient's astigmatism, corneal shape, age, and nomograms.
-
The incision helps flatten the steep meridian and somewhat steepen the opposite meridian (coupling effect), thereby reducing astigmatism.
-
The procedure may be done stand-alone or in conjunction with cataract surgery or IOL implantation.
4. What are the benefits of LRI compared to other astigmatism-correction options?
-
It is simpler, less expensive and less technology-intensive than some alternatives like toric intraocular lenses (IOLs) or laser-based astigmatism correction.
-
It is relatively safe with fewer risks of high irregularity since the incisions are peripheral.
-
It tends to stabilize more quickly and is less dependent on exact corneal thickness (pachymetry) compared with some central corneal incisional techniques.
-
It works well for mild to moderate astigmatism in appropriate patients.
5. What are the risks or limitations of LRI?
-
The amount of astigmatism correction is modest; it is less effective for higher amounts of astigmatism (greater than ~3 diopters) where toric IOLs or laser ablation may be superior.
-
There is a possibility of undercorrection or overcorrection, which might leave residual astigmatism.
-
The incisions may induce some mild irregularities in corneal shape or higher-order aberrations in rare cases.
-
Not suitable for patients with corneal diseases, keratoconus, prior corneal surgery, unstable corneas or peripheral corneal degenerations.
6. How long is the recovery, and when are results seen?
-
Recovery is usually rapid. Many patients notice improved vision within the first day or two after the incision(s).
-
Vision may continue to stabilize over the following weeks as the corneal shape adapts and the incisions heal.
-
Most normal daily activities can be resumed shortly, but you may be asked to avoid rubbing the eyes and follow post-operative instructions.
-
Long-term studies show the effect remains stable for years, though individual results vary.
7. Is LRI appropriate for everyone?
No-suitability depends on:
-
Amount and type of astigmatism (regular versus irregular)
-
Corneal health and thickness
-
Absence of certain corneal conditions such as keratoconus or significant peripheral corneal disease
-
The patient's overall ocular and systemic health
The ophthalmologist will assess these factors and recommend whether LRI is a good option or whether alternative methods (toric IOL, laser ablation) are better.
8. What should I expect after the procedure in terms of care?
-
You may receive antibiotic and anti-inflammatory eye drops after surgery.
-
Avoid rubbing the eye, swimming, heavy eye makeup, or dusty environments for a short period.
-
Attend follow-up visits so your surgeon can monitor healing, corneal shape, and refractive outcome.
-
If you are also having a cataract/IOL surgery with LRI, follow the combined post-operative care protocol.
-
Any discomfort is usually minimal; you may experience mild light sensitivity, tearing or eyelid awareness for a short time.
9. Are the results of LRI permanent?
The structural changes to the cornea created by the incision are long-lasting. In many cases, the reduction in astigmatism remains stable for years. However, changes to vision may still occur over time due to aging, lens changes (cataract), or other ocular conditions. If significant vision change happens later, additional correction may still be needed.
10. What questions should I ask my eye surgeon before having LRI?
-
Am I a good candidate for LRI given my astigmatism and corneal condition?
-
How much astigmatism do you expect the LRI to correct in my case?
-
What are the risks of under-correction or over-correction?
-
Will this be done alone, or alongside cataract surgery or IOL implantation?
-
What recovery timeline should I expect, and what activities should I avoid?
-
What could happen if the astigmatism changes later-can I still have other corrective procedures?
-
How experienced is the surgeon with LRI, and what outcome rates do they have?


