Introduction to Liver Transplant
A liver transplant is a complex surgical procedure in which a failing or diseased liver is replaced with a healthy liver from a donor. This donor liver can be obtained from a deceased individual or a living donor who gives a portion of their liver. One of the unique features of the liver is its remarkable ability to regenerate, allowing both the recipient and living donor's liver to grow and restore full functionality over time. Liver transplantation is primarily indicated for patients with end-stage liver disease, acute liver failure, metabolic liver disorders, and certain liver cancers. Over the past few decades, advances in surgical techniques, anesthesia, post-operative care, and immunosuppressive therapy have transformed liver transplantation from a high-risk procedure into a life-saving treatment with high survival rates. Patients who undergo liver transplantation often experience dramatic improvements in quality of life, returning to normal activities and regaining independence, while also preventing life-threatening complications from progressive liver disease.
Causes and Risk Factors for Liver Transplant
Liver transplantation is required when the liver's vital functions-such as detoxification, bile production, blood clotting, and metabolism-are severely compromised. The causes leading to liver failure and necessitating transplantation can be categorized as chronic, acute, and genetic/metabolic:
-
Chronic Liver Diseases: Cirrhosis caused by hepatitis B or C, long-term alcohol abuse, or non-alcoholic fatty liver disease (NAFLD) progressing to non-alcoholic steatohepatitis (NASH) are among the most common reasons. Chronic damage over years gradually impairs liver function, eventually necessitating transplantation.
-
Acute Liver Failure: This can occur suddenly due to drug-induced liver injury (such as acetaminophen overdose), acute viral hepatitis, or vascular obstruction. In these situations, urgent transplantation may be the only option to prevent death.
-
Genetic and Metabolic Disorders: Conditions such as Wilson's disease, alpha-1 antitrypsin deficiency, and familial hypercholesterolemia can lead to liver failure in children and young adults.
-
Liver Cancers: Early-stage hepatocellular carcinoma in a cirrhotic liver may be treated with transplantation as a curative approach when other surgical options are not feasible.
Risk factors that influence liver transplant outcomes include comorbid conditions such as cardiovascular disease, diabetes, kidney dysfunction, infections, and obesity. Patient age, nutritional status, and psychosocial factors also affect post-transplant recovery. Additionally, waiting for a donor liver carries inherent risk, as disease progression can continue during the waiting period, emphasizing the importance of timely evaluation and listing for transplant.
Symptoms and Signs Indicating the Need for Liver Transplant
Patients who require liver transplantation often display signs of advanced liver disease or acute liver failure, which can be progressive and life-threatening. Key clinical signs and symptoms include:
-
Jaundice: Yellowing of the skin and eyes due to elevated bilirubin levels, indicating impaired liver function.
-
Ascites: Accumulation of fluid in the abdomen caused by portal hypertension and hypoalbuminemia, often leading to abdominal distension and discomfort.
-
Variceal Bleeding: Enlarged veins in the esophagus or stomach may rupture, causing potentially life-threatening bleeding.
-
Hepatic Encephalopathy: Mental status changes such as confusion, disorientation, sleep-wake cycle disturbances, and hand tremors (asterixis) due to the accumulation of toxins like ammonia.
-
Coagulopathy: Easy bruising or bleeding tendencies because the liver produces clotting factors, which are deficient in advanced disease.
-
Muscle Wasting and Weight Loss: Chronic liver disease often results in malnutrition and loss of muscle mass.
-
Acute Deterioration: In cases of fulminant liver failure, patients may rapidly develop multi-organ dysfunction and systemic complications.
When these symptoms persist despite medical management, liver transplantation is considered the definitive treatment to restore liver function and prevent further complications.
Diagnosis and Pre-Transplant Evaluation
Before undergoing liver transplantation, patients undergo a comprehensive evaluation to determine suitability for surgery, ensure optimal outcomes, and reduce postoperative complications. This evaluation typically includes:
-
Detailed Medical History and Physical Examination: Assessment of the underlying liver disease, complications, comorbidities, prior surgeries, and overall physical condition.
-
Laboratory Testing: Liver function tests, renal function tests, coagulation studies, and metabolic panels help assess disease severity and organ function.
-
Imaging Studies: Ultrasound, CT scan, and MRI are used to evaluate liver size, morphology, presence of tumors, portal vein patency, and other anatomical considerations.
-
Disease Severity Scoring: Scores such as MELD (Model for End-Stage Liver Disease) or Child-Pugh are used to quantify liver failure severity and prioritize patients on the transplant waiting list.
-
Cardiopulmonary Assessment: Because transplantation is major surgery, cardiac and respiratory evaluations are critical.
-
Psychosocial and Nutritional Evaluation: Assessment ensures that the patient can adhere to lifelong medication regimens and post-transplant care requirements.
-
Donor Matching Evaluation: Blood type, size, and sometimes HLA compatibility are considered, particularly in living donor transplantation.
This rigorous process ensures that the patient is an appropriate candidate for transplantation and that potential risks are identified and mitigated.
Treatment Options for Liver Transplant
The liver transplant itself is the primary treatment, but there are several approaches and adjuncts:
-
Deceased Donor Liver Transplantation (DDLT): Whole liver or split liver segments from a deceased donor are transplanted into the recipient.
-
Living Donor Liver Transplantation (LDLT): A living donor gives a portion of their liver, typically a lobe, to the recipient. Both donor and recipient livers regenerate over time.
-
Split-Liver Transplantation: One donor liver is divided for two recipients, usually an adult and a child.
-
Combined Transplants: In select cases, a patient may require liver-kidney transplantation if there is concurrent kidney failure.
-
Bridging Treatments Pre-Transplant: Patients may require management of ascites, varices, renal dysfunction, or hepatic encephalopathy while awaiting a donor liver.
-
Postoperative Care: Lifelong immunosuppressive therapy is critical to prevent graft rejection, along with monitoring for infections, metabolic complications, and graft function.
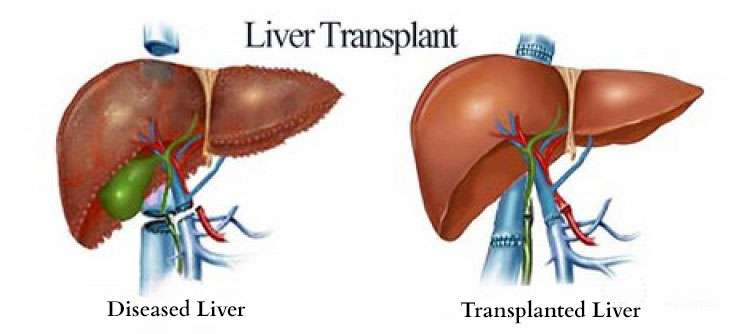
The transplant procedure itself involves removing the diseased liver and attaching the donor liver by connecting the portal vein, hepatic artery, hepatic veins, and bile duct. The surgery is major, requiring careful postoperative management in an intensive care setting.
Prevention and Management of Liver Disease Pre- and Post-Transplant
While transplantation addresses advanced disease, prevention and management strategies aim to delay disease progression and optimize post-transplant outcomes:
-
Lifestyle Modifications: Avoid alcohol, maintain a healthy weight, and manage metabolic syndrome components like diabetes and hypertension.
-
Viral Hepatitis Control: Vaccination, antiviral therapy, and monitoring for hepatitis B and C reduce liver damage and recurrence post-transplant.
-
Surveillance for Complications: Routine monitoring for hepatocellular carcinoma, varices, and renal dysfunction ensures timely intervention.
-
Post-Transplant Management: Lifelong immunosuppressive therapy is mandatory, along with infection prophylaxis, regular lab monitoring, lifestyle adjustments, and adherence to dietary and exercise guidelines.
-
Living Donor Management: In LDLT, donor health is equally critical, requiring rigorous preoperative assessment and follow-up to ensure safe liver regeneration.
Complications of Liver Transplant
Despite advances, liver transplantation carries potential complications:
Early Complications
-
Graft dysfunction or primary non-function
-
Bleeding or vascular thrombosis (hepatic artery, portal vein)
-
Biliary leaks or strictures
-
Infections due to surgery and immunosuppression
-
Acute rejection
Late Complications
-
Chronic rejection or fibrosis of the graft
-
Immunosuppressant-related complications (kidney dysfunction, hypertension, diabetes, infections, cancers)
-
Recurrence of primary disease (e.g., hepatitis C, NAFLD)
-
Biliary complications requiring secondary interventions
Careful monitoring, early detection, and medical intervention are essential to mitigate these complications and optimize long-term survival.
Living with the Condition of Liver Transplant
Patients who undergo liver transplantation experience significant improvement in quality of life, but ongoing care is critical:
-
Medication Adherence: Lifelong immunosuppressants prevent graft rejection. Missing doses can lead to severe complications.
-
Regular Follow-Up: Frequent clinic visits, laboratory tests, and imaging monitor graft function and detect complications early.
-
Healthy Lifestyle: A balanced diet, physical activity, avoidance of alcohol, and protection from hepatotoxic substances are essential.
-
Infection Prevention: Immunosuppression increases susceptibility to infections; vaccinations, hygiene, and avoidance of high-risk exposure are critical.
-
Psychosocial Support: Support groups, counseling, and education about post-transplant life help patients adapt emotionally and mentally.
-
Long-Term Health Maintenance: Patients must monitor for cardiovascular disease, kidney dysfunction, and secondary malignancies, all of which can be exacerbated by immunosuppressive therapy.
With careful adherence to medical guidance and lifestyle recommendations, most liver transplant recipients can live many years with a fully functional graft and enjoy a near-normal life.
Top 10 Frequently Asked Questions about Liver Transplant
1. What is a liver transplant and when is it needed?
A liver transplant is a complex surgical procedure in which a diseased or failing liver is replaced with a healthy liver or a portion of it from a donor. It is typically recommended for patients whose liver is no longer able to function properly due to conditions such as end-stage cirrhosis, acute liver failure, chronic hepatitis, metabolic liver disorders, or primary liver cancer. The procedure restores the liver's ability to filter toxins, produce essential proteins, aid in digestion, and maintain overall metabolic balance. Liver transplantation is usually considered only when other medical or surgical treatments have failed or are not sufficient to sustain liver function.
2. Who is a candidate for a liver transplant?
Candidates for a liver transplant are usually adults or children with irreversible liver damage or liver failure. Key factors for eligibility include: having a severe liver condition that cannot be treated with medication, being healthy enough to withstand major surgery, and not having active infections or uncontrolled medical problems such as heart or lung disease. Patients with a history of alcohol or substance abuse may need to demonstrate a period of abstinence before being considered for transplant. A thorough evaluation by a transplant team-including physical exams, lab tests, imaging studies, and psychosocial assessments-is performed to ensure the patient is suitable for surgery and post-transplant care.
3. What types of donors are available for liver transplant?
There are two main types of donors: deceased donors and living donors. Deceased donor livers are obtained from individuals who have passed away and whose organs are donated for transplantation. Living donor liver transplants involve a healthy individual donating a portion of their liver, which then regenerates over time in both the donor and recipient. The selection of a donor involves careful matching of blood type, body size, and overall compatibility. Allocation of donor livers is typically based on the severity of liver disease and urgency of need, ensuring that patients in critical condition are prioritized.
4. How long is the waiting period for a liver transplant?
The waiting time for a liver transplant can vary widely depending on factors such as availability of donor organs, blood type, size compatibility, geographic location, and the patient's medical urgency. Some patients may wait a few weeks, while others may wait months or even years. Patients with a living donor often experience shorter waiting times, whereas those relying on deceased donor livers must remain on a waiting list and may require ongoing medical care and monitoring to manage their liver disease during this period.
5. What are the risks and complications of liver transplant surgery?
Liver transplant surgery is major and carries risks both during and after the procedure. Surgical risks include bleeding, infection, blood clots, or complications from anesthesia. After the transplant, patients must take immunosuppressive medications to prevent organ rejection, which can increase the risk of infections, kidney problems, high blood pressure, and diabetes. Other possible complications include bile duct problems, recurrence of the original liver disease, and side effects from long-term medications. Despite these risks, liver transplantation is often life-saving for patients with end-stage liver disease, and careful management by the transplant team can minimize complications.
6. What does recovery look like after a liver transplant?
Recovery after a liver transplant is a gradual process that typically begins in the intensive care unit immediately after surgery. Patients usually stay in the hospital for 2 to 3 weeks, during which the medical team monitors liver function, vital signs, and potential complications. Full recovery can take several months. Patients are required to follow a strict medication regimen, attend frequent follow-up visits, and adopt lifestyle measures such as a balanced diet, adequate rest, gentle physical activity, and avoidance of infections. Over time, many patients experience significant improvement in energy, appetite, and overall quality of life.
7. What lifestyle changes are needed after a liver transplant?
After a liver transplant, lifestyle modifications are crucial for the long-term success of the procedure. Patients must take immunosuppressive medications for life to prevent rejection of the new liver. Regular exercise, a balanced diet, and maintaining a healthy weight are essential. Alcohol and smoking should be strictly avoided, and exposure to infections should be minimized. Routine medical check-ups, lab tests, and monitoring of liver function are also necessary to detect any complications early. Adhering to these lifestyle adjustments helps ensure that the transplanted liver functions optimally and lasts for many years.
8. Can the original liver disease come back after transplantation?
In some cases, the original liver disease can recur in the transplanted liver. For example, viral hepatitis, autoimmune liver disease, or certain metabolic conditions may affect the new liver if not carefully managed. Transplant teams implement preventive measures such as antiviral therapy, immunosuppressive adjustments, and lifestyle interventions to reduce the risk of recurrence. Regular monitoring through blood tests, imaging, and liver biopsies helps detect any early signs of disease returning and ensures timely management.
9. What is the success rate and long-term outlook after a liver transplant?
Liver transplantation has a high success rate, particularly in experienced transplant centers. Short-term survival rates are generally above 85-90% within the first year after surgery. Long-term survival depends on factors such as the patient's overall health, adherence to medications, management of complications, and the underlying cause of liver failure. Many patients go on to lead active, fulfilling lives with restored liver function and improved quality of life. With careful medical care and follow-up, a transplanted liver can last many years, often decades.
10. What are the costs and insurance considerations for liver transplant?
Liver transplantation is a costly and complex procedure that includes surgery, hospital stay, medications, and long-term follow-up care. The cost may vary depending on the hospital, country, type of donor, and patient's medical condition. Most health insurance plans cover liver transplants if deemed medically necessary, but coverage for medications, post-transplant care, and complications can vary. Patients and families should consult both the hospital and their insurance provider to understand coverage, out-of-pocket expenses, and financing options. Financial counseling is often provided by transplant centers to help plan for these costs.


