Introduction to Lumbar Fusion
The lumbar spine, located in the lower back, is one of the most important structures of the human body. It provides support for the upper body, enables movement, and protects the spinal cord and nerves. Over time, or as a result of trauma or disease, the structures that make up the spine—including the vertebrae, intervertebral discs, ligaments, and joints—can become unstable or degenerated. When this instability or degeneration leads to chronic pain, nerve compression, or significant loss of function that cannot be relieved by non-surgical methods, a procedure known as lumbar fusion may be considered.
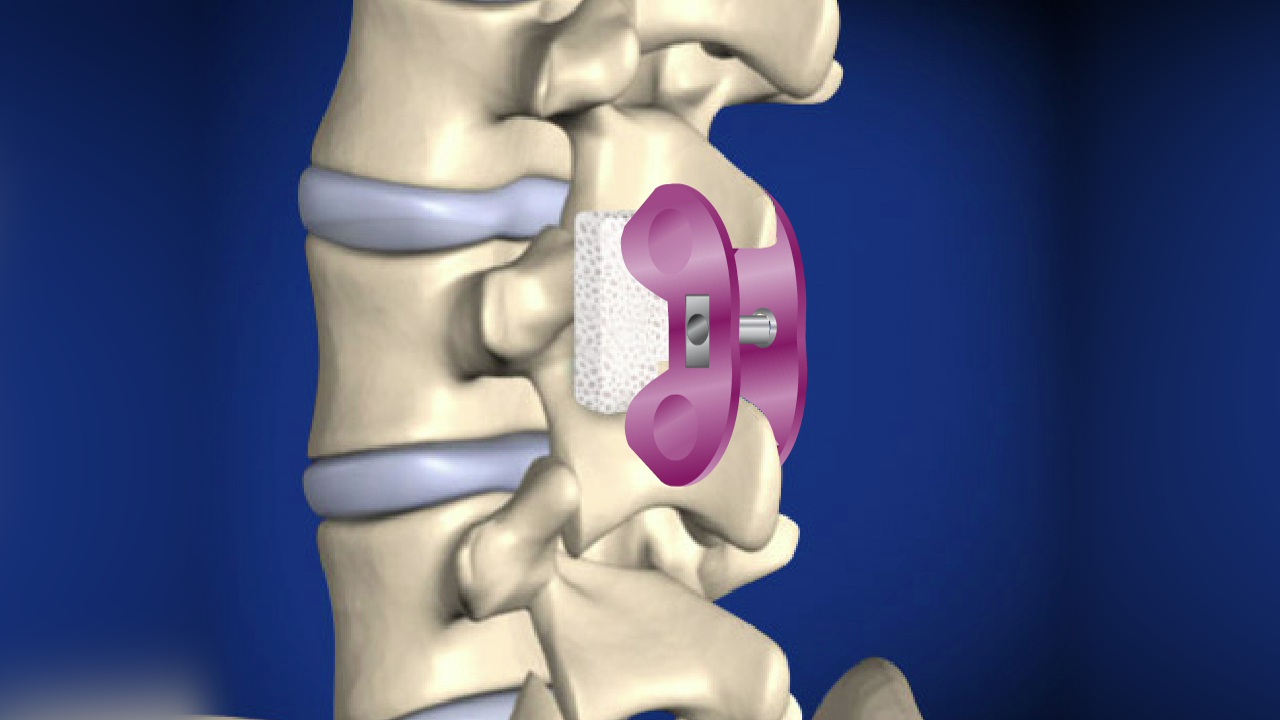
Lumbar fusion (also called spinal fusion) is a surgical procedure that permanently joins two or more vertebrae together, eliminating motion between them. By doing so, it stabilizes the spine and reduces pain caused by movement of the affected vertebrae. Bone grafts and metal implants (such as screws, rods, or plates) are often used to help the bones heal into a single solid unit over time. The purpose of lumbar fusion is not only to relieve pain but also to restore spinal stability, correct deformities, and protect the nerves from compression.
This procedure is commonly recommended for patients suffering from severe degenerative disc disease, spondylolisthesis, spinal instability, fractures, or deformities like scoliosis. Over the years, lumbar fusion techniques have advanced significantly, with minimally invasive approaches, biologic grafts, and improved fixation systems enhancing success rates and reducing recovery time. However, it is essential for patients to understand that lumbar fusion is a major surgery—it limits motion at the fused level, requires rehabilitation, and demands long-term commitment to spine health for the best outcomes.
Causes and Risk Factors of Lumbar Fusion
Lumbar fusion is typically considered when spinal instability, degeneration, or deformity causes persistent pain and neurological symptoms that fail to improve with conservative treatments.
Common Causes:
-
Degenerative Disc Disease: As people age, intervertebral discs lose hydration and elasticity, leading to disc height reduction and abnormal motion between vertebrae. This degeneration often results in chronic lower back pain.
-
Spondylolisthesis: This condition occurs when one vertebra slips forward over the one below it, leading to nerve compression, instability, and pain.
-
Spinal Stenosis: Narrowing of the spinal canal can put pressure on nerves, often requiring fusion to stabilize the spine after decompression surgery.
-
Recurrent Disc Herniation: When disc herniation occurs repeatedly despite previous surgeries, fusion may be needed to provide stability.
-
Traumatic Injuries: Fractures or dislocations from accidents or falls can disrupt spinal alignment and stability, requiring fusion to restore structure.
-
Spinal Tumors or Infections: Surgical removal of tumors or infection-damaged vertebrae sometimes necessitates fusion to rebuild the spinal column.
Risk Factors:
Certain conditions increase the likelihood of spinal degeneration or the need for fusion surgery:
-
Aging: Natural wear and tear weaken discs and joints over time.
-
Smoking: Nicotine reduces blood flow to the spine, impairing disc nutrition and bone healing.
-
Obesity: Excess body weight places continuous stress on the lumbar spine.
-
Occupational Hazards: Heavy lifting, repetitive bending, or prolonged sitting can accelerate disc degeneration.
-
Genetic Predisposition: Family history of disc problems or spinal deformities increases susceptibility.
-
Previous Spine Surgery: Patients who've undergone prior spine procedures may experience adjacent segment degeneration, sometimes requiring fusion.
Understanding these causes and risk factors is vital for prevention and early intervention, helping patients and physicians identify when conservative management might suffice and when surgical stabilization becomes necessary.
Symptoms and Signs of Lumbar Spine Conditions Requiring Fusion
Patients who are candidates for lumbar fusion often experience a wide range of symptoms caused by instability, nerve compression, or degenerative changes in the spine.
Common Symptoms Include:
-
Chronic Low Back Pain: Persistent aching or stiffness that worsens with motion, bending, lifting, or prolonged standing.
-
Radicular Pain (Sciatica): Sharp, shooting pain radiating from the lower back into the buttocks, thighs, or legs, often due to nerve compression.
-
Numbness or Tingling: Sensations in the legs or feet caused by compressed nerves.
-
Weakness in Legs: Difficulty standing, walking, or climbing stairs due to nerve-related muscle weakness.
-
Loss of Mobility: Reduced ability to bend, twist, or perform normal movements.
-
Deformity or Instability: Abnormal spinal curvature or slippage visible on imaging or physical examination.
Physical Examination Findings:
During a clinical assessment, doctors may observe:
-
Tenderness in the lower back muscles.
-
Reduced lumbar range of motion.
-
Muscle weakness in one or both legs.
-
Altered reflexes, indicating nerve involvement.
-
Positive straight-leg raise test (reproducing leg pain).
Symptoms vary depending on the severity of degeneration and which nerves are affected. When pain and dysfunction persist despite medication, physiotherapy, and injections, spinal fusion is often considered to provide stability and long-term pain relief.
Diagnosis of Acupressure Therapy
Acupressure therapy is typically not diagnosed in the conventional sense, as it is a holistic, alternative treatment method rather than a medical condition. However, it is important to assess whether acupressure therapy is appropriate for an individual based on their symptoms or condition. Here's how acupressure therapy is usually approached from a diagnostic perspective:
Traditional Chinese Medicine Diagnosis
In Traditional Chinese Medicine, the diagnosis process for acupressure is rooted in holistic principles. Practitioners take a comprehensive approach to understanding the body's health. This process often involves:
-
Pulse Diagnosis:
-
Pulse diagnosis involves assessing the quality of the pulse at various points on the body. This helps the practitioner gauge the strength and flow of qi and determine which acupoints need stimulation.
-
-
Tongue Diagnosis:
-
In TCM, tongue examination is an important diagnostic tool. The tongue's color, shape, and coating can reveal important information about the condition of internal organs and energy imbalances.
-
-
Physical and Symptom Evaluation:
-
The acupressure practitioner will assess pain areas, muscle tension, mental state, and other physical symptoms before deciding which acupoints to target.
-
-
Diagnosis of Underlying Conditions:
-
Acupressure is often used as a complementary treatment for symptoms and diseases, so practitioners may use acupressure in conjunction with Western diagnostic tools to develop a comprehensive treatment plan.
-
Consultation with Acupressure Practitioners
Though many people practice acupressure at home, consulting a licensed acupuncturist or acupressure therapist is recommended for serious or chronic conditions. Practitioners can assess symptoms and create a customized acupressure plan based on individual health needs.
Treatment Options for Acupressure
Acupressure is a traditional healing practice that involves applying physical pressure to specific points on the body, known as acupoints, to relieve pain and promote overall wellness. It's often used as a complementary therapy for various conditions. Here are some common treatment options and approaches for acupressure:
Acupressure Techniques and Methods
Acupressure is a manual therapy, meaning it involves the application of physical pressure to the acupoints. The common techniques include:
-
Pressing:
-
The practitioner applies steady, firm pressure to acupoints, typically using their thumbs, fingers, or elbows. The pressure is applied for a set duration, usually 30 seconds to 2 minutes per point.
-
-
Circular Motions:
-
Acupressure can be applied using gentle circular motions to stimulate the flow of energy and enhance the therapeutic effects on the acupoints.
-
-
Tapping:
-
Light, rhythmic tapping on acupoints can also be used to activate energy flow, improve circulation, and relieve tension.
-
-
Vibration:
-
Vibrational pressure or pulsing can be applied to certain points to promote the release of tension and induce relaxation.
-
Self-Acupressure Techniques
For individuals practicing acupressure at home, the following techniques are commonly used:
-
LI4 (Hegu): Located between the thumb and index finger, this point is commonly used for general pain relief, headache relief, and stress management.
-
P6 (Neiguan): Located on the inner forearm, approximately two inches from the wrist crease, this point is effective for nausea and anxiety relief.
-
ST36 (Zusanli): Located about four fingers below the kneecap, this point is known for its ability to boost energy and support digestive health.
Professional Acupressure Sessions
For chronic conditions or more complex cases, individuals may seek professional acupressure treatments from certified practitioners. Sessions typically last anywhere from 30 minutes to 1 hour, and the practitioner may combine acupressure with other therapies such as acupuncture or herbal remedies.
Prevention and Management of Acupressure
Acupressure, a traditional therapy based on applying pressure to specific points on the body, is generally safe when practiced correctly. However, there are certain precautions and management practices that can help prevent any adverse effects or complications.
Preventing Illness with Acupressure
-
Regular Use of Acupressure:
-
Regular practice of acupressure can help maintain a balanced energy flow, promote general health, and prevent the development of chronic ailments.
-
-
Stress Prevention:
-
Using acupressure to reduce stress before it becomes overwhelming helps prevent mental health conditions like anxiety and depression.
-
-
Improving Sleep:
-
Regular acupressure sessions, especially before bedtime, can enhance sleep quality and reduce insomnia and restlessness.
-
Managing Existing Conditions
-
Chronic Pain:
-
Acupressure is widely used as a complementary treatment for chronic pain. Regular sessions can reduce reliance on medication and improve quality of life for those with arthritis, fibromyalgia, or musculoskeletal issues.
-
-
Digestive Disorders:
-
People with chronic digestive issues such as IBS or acid reflux can use acupressure to stimulate the digestive system and alleviate symptoms.
-
Complications of Acupressure
Prevention and Management of Acupressure involves practices that ensure safe and effective application while minimizing the risks. Below are the key points for its prevention and management:
Possible Side Effects
Acupressure is generally safe, but there are some risks and side effects to be aware of:
-
Bruising: Applying too much pressure to a point may cause minor bruising or soreness.
-
Dizziness or Nausea: Occasionally, individuals may feel light-headed or nauseous after a session, especially if the pressure is applied too forcefully.
-
Temporary Discomfort: Some individuals may experience mild muscle soreness or tenderness at the acupoint areas after a treatment session.
When Acupressure Should Be Avoided
-
Pregnancy: Certain acupressure points should be avoided during pregnancy, especially those that may induce labor.
-
Skin Conditions: Acupressure should not be performed on broken or inflamed skin, such as wounds, rashes, or open sores.
-
Severe Health Conditions: Individuals with severe cardiovascular issues, blood clotting disorders, or autoimmune conditions should consult a healthcare provider before attempting acupressure.
Living with the Condition of Acupressure
Living with acupressure as a form of therapy can have a profound impact on a person's well-being, especially when used regularly for managing stress, pain, or various health issues. Here's an overview of what living with acupressure treatment might look like:
Integrating Acupressure into Your Lifestyle
For individuals suffering from chronic conditions, acupressure can be an ongoing part of their self-care routine. Here's how it can fit into daily life:
-
Self-Management: Acupressure can be done at home, allowing individuals to manage stress, pain, and fatigue between visits to healthcare providers.
-
Emotional and Mental Wellness: Acupressure techniques can help maintain emotional balance, reduce anxiety, and improve overall mood.
-
Holistic Health: When used regularly, acupressure can contribute to overall well-being, improving circulation, promoting relaxation, and stimulating detoxification processes.
Top 10 Frequently Asked Questions about Lumbar Fusion Surgery
1. What is lumbar fusion surgery?
Lumbar fusion surgery is a procedure designed to permanently join two or more vertebrae in the lower back (lumbar spine) to eliminate motion between them. The goal is to reduce pain caused by unstable or damaged spinal segments, degenerative disc disease, spondylolisthesis, spinal deformities, or fractures. During the surgery, bone grafts (either from the patient, donor, or synthetic material) are placed between the vertebrae, and metal screws, rods, or plates are often used to stabilize the spine until fusion occurs.
2. Who is a candidate for lumbar fusion surgery?
Ideal candidates are patients who experience chronic lower back pain that has not improved with non-surgical treatments such as physical therapy, medications, or injections. Lumbar fusion is typically recommended for individuals with:
-
Spinal instability or vertebral slippage (spondylolisthesis).
-
Severe degenerative disc disease affecting one or more discs.
-
Recurrent spinal fractures or deformities.
-
Chronic pain caused by failed previous back surgeries.
A thorough evaluation by a spinal surgeon, including imaging studies like MRI or CT scans, is required to determine suitability.
3. How is lumbar fusion different from lumbar disc replacement?
Lumbar fusion eliminates movement at the affected spinal segment to stabilize the spine, whereas lumbar disc replacement replaces a damaged disc with an artificial implant while preserving motion. Fusion may provide stronger stability but can increase stress on adjacent spinal segments, potentially leading to further degeneration. Disc replacement is often considered in patients with preserved facet joints and no spinal instability.
4. How is the surgery performed?
Lumbar fusion can be performed through various approaches, including posterior (back), anterior (front), or lateral (side) approaches, depending on the patient's anatomy and the surgeon's preference. During the procedure, damaged discs are removed, and bone grafts are inserted between the vertebrae. Screws, rods, or cages are used to stabilize the spine while the bone graft fuses over time. Surgery usually lasts 2-5 hours, depending on the number of vertebrae being fused and complexity of the case.
5. What are the benefits of lumbar fusion surgery?
Lumbar fusion can provide several significant benefits:
-
Reduction or elimination of chronic back pain caused by spinal instability.
-
Correction of spinal deformities or abnormal curvatures.
-
Prevention of further vertebral slippage.
-
Improved quality of life and the ability to perform daily activities with less discomfort.
While fusion reduces motion at the affected segment, it stabilizes the spine and often provides long-term pain relief when non-surgical treatments fail.
6. What are the risks and complications of lumbar fusion?
As with any major surgery, lumbar fusion carries risks. Potential complications include:
-
Infection or bleeding.
-
Nerve injury causing numbness, weakness, or pain in the legs.
-
Failure of the vertebrae to fuse (non-union), which may require revision surgery.
-
Blood clots, anesthesia complications, or hardware issues.
-
Pain at the site where bone grafts are taken (if autograft is used).
Choosing an experienced spine surgeon and following post-operative instructions significantly reduces these risks.
7. What is the recovery process like?
Recovery after lumbar fusion varies depending on the number of vertebrae fused, surgical approach, and patient health. Typically, patients stay in the hospital for 3-5 days after surgery. Light activity such as walking is encouraged soon after surgery to improve circulation. Full recovery, including complete fusion of the vertebrae, usually takes 3-6 months, during which patients may gradually resume work and daily activities. Physical therapy is often recommended to strengthen core muscles, improve flexibility, and support long-term spinal health.
8. Will lumbar fusion limit my mobility?
Lumbar fusion eliminates motion at the fused segment(s), which can slightly reduce flexibility in the lower back. However, most patients regain the ability to perform daily activities without significant limitations. Maintaining overall spinal health, practicing core strengthening exercises, and avoiding high-impact activities are essential to minimize strain on adjacent spinal segments and preserve long-term mobility.
9. How long do the results of lumbar fusion last?
Lumbar fusion is intended to provide permanent stabilization of the affected spinal segment. Most patients experience long-term relief from pain and improved spinal stability. However, adjacent segments may experience increased stress over time, potentially leading to degenerative changes or pain in other areas of the spine. Regular follow-ups with your spinal surgeon help monitor spine health and prevent complications.
10. How much does lumbar fusion surgery cost, and is it covered by insurance?
The cost of lumbar fusion surgery depends on factors such as the hospital, surgeon's expertise, number of vertebrae fused, and post-operative care required. Generally, it is a major surgical procedure with costs ranging from several thousand to tens of thousands of dollars. Most health insurance plans cover lumbar fusion surgery if it is deemed medically necessary, including hospital stay, surgery, and some post-operative care. Patients should consult both their surgeon and insurance provider to understand coverage, out-of-pocket expenses, and financing options.


