Introduction to Macular Translocation
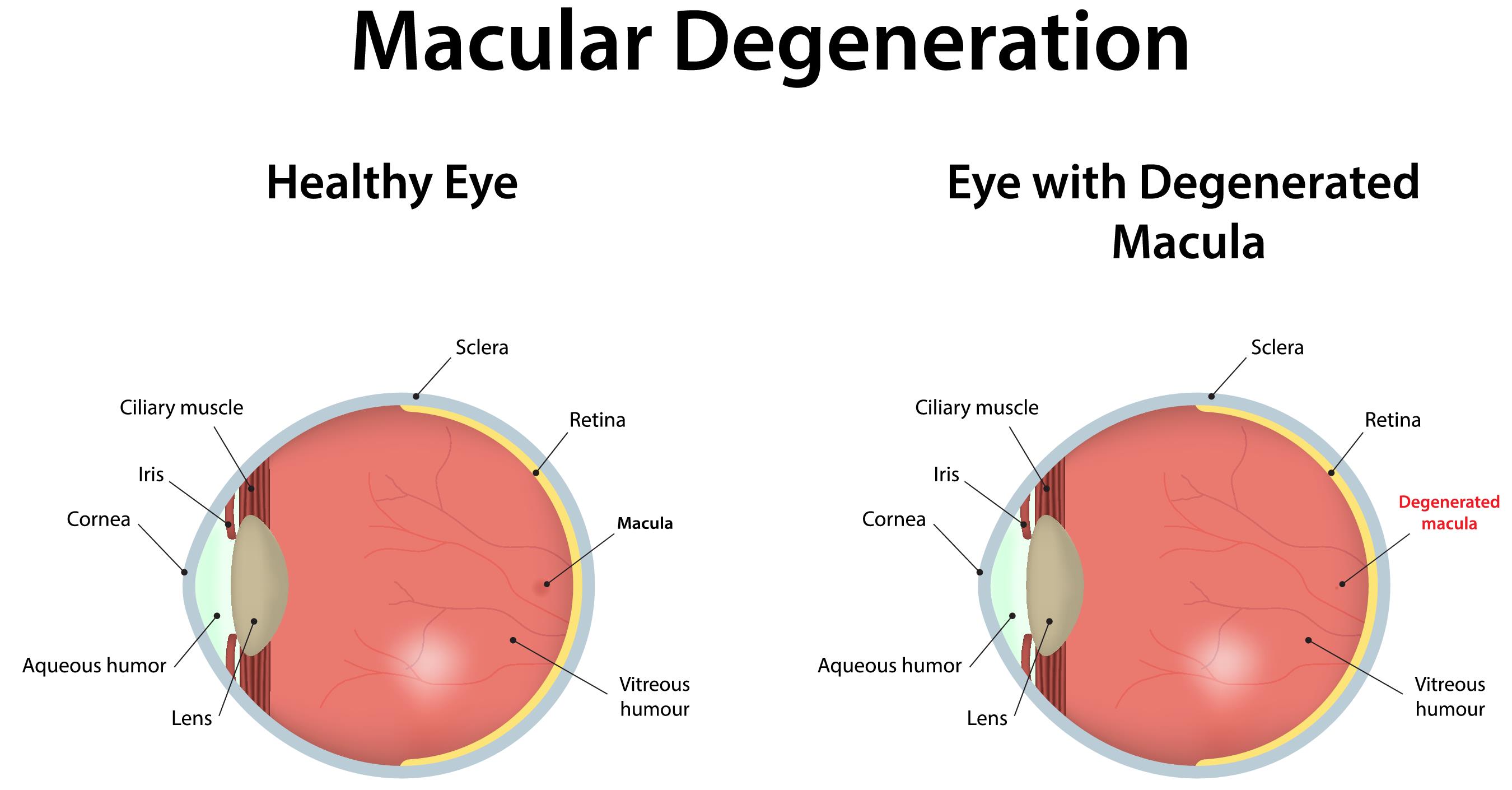
The human eye is a highly complex organ responsible for our sense of vision, and at the very center of this delicate system lies the macula, a small but powerful area on the retina responsible for detailed, sharp, and central vision. The macula allows us to read, recognize faces, and see fine details. Unfortunately, when the macula is damaged - as in wet age-related macular degeneration (AMD) or other severe retinal disorders - it can lead to irreversible loss of central vision. The condition becomes particularly challenging when abnormal blood vessels grow beneath the macula, damaging the supporting tissues (retinal pigment epithelium and choroid).
Macular translocation is a highly specialized surgical procedure designed to relocate the macula - the most sensitive part of the retina - from the diseased or damaged area to a healthier portion of the eye. By doing so, it allows the macula to rest on healthy retinal tissue, where it can function better, potentially restoring or stabilizing vision. The surgery involves delicate manipulation of the retina, often rotating or repositioning it after creating a controlled retinal detachment.
Although modern pharmacologic therapies such as anti-VEGF injections have largely become first-line treatments for macular degeneration, macular translocation remains an important option for patients who do not respond to these therapies or who have advanced disease. It is a complex and technically demanding operation that requires exceptional precision and postoperative care, but for selected individuals, it can offer renewed hope and an improved quality of life.
Causes and Risks Leading to Macular Translocation
Macular translocation is generally considered when the underlying retinal tissue beneath the macula is severely diseased and cannot adequately nourish the photoreceptors responsible for vision.
Common Causes Include:
-
Wet Age-Related Macular Degeneration (AMD): The most frequent cause, where abnormal blood vessels grow beneath the macula (choroidal neovascularization), leaking fluid and blood, damaging the macular cells.
-
Large Disciform Scars: In some advanced cases of AMD, a scar forms under the fovea (the very center of the macula), disrupting central vision.
-
Macular Choroidopathies: Certain rare eye conditions, including idiopathic CNV or myopic maculopathy, may also require such surgery.
-
Failed Conventional Treatments: Patients who have not responded to intravitreal injections, laser photocoagulation, or photodynamic therapy may be candidates for surgical intervention.
Risk Factors:
-
Advancing Age: Macular degeneration primarily affects people over 60 years old.
-
Genetic Predisposition: Family history of AMD or other retinal diseases.
-
Lifestyle and Environmental Factors: Smoking, poor diet, high cholesterol, hypertension, and prolonged exposure to ultraviolet light can accelerate macular damage.
-
Comorbid Ocular Conditions: Prior retinal detachment, diabetic retinopathy, or other retinal diseases that compromise the health of the macula.
In essence, macular translocation is not a first-line treatment but rather a salvage procedure - reserved for patients whose vision is deteriorating despite other interventions, yet who still retain enough viable retinal function to benefit from repositioning.
Symptoms and Signs of Macular Damage Leading to Translocation
Patients requiring macular translocation often present with progressive central vision loss, one of the hallmark signs of macular disease. The visual symptoms are usually more pronounced in the affected eye, though bilateral involvement is common in age-related diseases.
Key Symptoms:
-
Blurring or Distortion of Central Vision: Straight lines appear wavy (metamorphopsia) or letters on a page seem distorted or faded.
-
Dark or Empty Spots (Scotomas): Patients may describe a dark patch or missing area in their central vision.
-
Difficulty Reading or Recognizing Faces: Fine visual tasks become increasingly difficult as central vision fades.
-
Changes in Color Perception: Colors may appear dull or less distinct.
-
Decreased Visual Acuity: Even with corrective lenses, patients find it hard to achieve clear focus.
Signs on Clinical Examination:
-
Retinal examination reveals pigmentary changes, scarring, or hemorrhages under the macula.
-
Optical Coherence Tomography (OCT) scans show damage to the photoreceptor and RPE layers, often with subretinal fluid or neovascular membranes.
-
Fluorescein angiography may confirm abnormal leakage from choroidal neovascularization.
When such symptoms persist and standard treatments no longer provide improvement, surgical options like macular translocation are considered to reposition the macula over healthier retinal tissue and restore visual potential.
Diagnosis and Evaluation Before Macular Translocation
The decision to undergo macular translocation involves a comprehensive diagnostic evaluation to confirm the cause of macular damage, assess disease severity, and determine surgical suitability.
Diagnostic Steps Include:
-
Detailed Patient History: Duration and progression of vision loss, history of AMD, prior treatments (like anti-VEGF injections), and presence of any systemic diseases.
-
Visual Acuity Testing: To quantify the extent of vision loss and determine baseline vision levels.
-
Ocular Imaging Studies:
-
Optical Coherence Tomography (OCT): Provides high-resolution cross-sectional images of the retina, identifying damage to the photoreceptors and RPE.
-
Fluorescein Angiography: Highlights abnormal blood vessels and leakage under the macula.
-
Indocyanine Green Angiography (ICG): Useful for deeper choroidal vessel visualization.
-
-
Fundus Examination: Detects scarring, pigment changes, or hemorrhage.
-
Assessment of Retinal Viability: Determines whether enough healthy retinal tissue exists to benefit from relocation.
-
Overall Health Evaluation: Since macular translocation is a complex procedure, general health status, anesthesia tolerance, and systemic conditions (like cardiovascular or diabetic disease) are assessed.
This thorough evaluation ensures that patients selected for surgery have a reasonable chance of success and can tolerate the demanding post-operative care required for optimal results.
Treatment Options for Macular Translocation
Macular translocation is a sophisticated surgical treatment primarily used for certain patients with wet age-related macular degeneration (AMD) and other macular diseases where conventional therapies (like anti-VEGF injections) are ineffective or not possible. This surgery aims to move the macula (the center of the retina responsible for sharp central vision) to a healthier area of the underlying retinal pigment epithelium (RPE) and choroid, bypassing damaged or scarred tissue.
Macular Translocation Surgery Overview
Macular translocation is a microsurgical procedure involving the delicate repositioning of the retina to shift the macula to a healthier region of the eye. The surgery begins with a pars plana vitrectomy (removal of the vitreous gel), followed by carefully detaching the retina. The retina is then rotated or shifted so that the macula is positioned over an area of healthy retinal pigment epithelium. The retina is reattached using a gas or silicone oil tamponade to hold it in place as it heals.
Depending on the technique used, macular translocation may involve:
-
Full Macular Translocation (360° Rotation): The entire retina is detached and rotated to a new position.
-
Limited Translocation: Only part of the retina is shifted, often by shortening the sclera or partial rotation.
Other Treatment Options (Non-Surgical):
-
Anti-VEGF Therapy: Intravitreal injections (such as ranibizumab, bevacizumab, or aflibercept) to block abnormal blood vessel growth.
-
Photodynamic Therapy: Uses light-activated drugs to seal leaking vessels.
-
Laser Photocoagulation: Destroys abnormal vessels but is suitable only for specific cases.
Macular translocation is usually reserved for those who do not respond to these conservative therapies. It aims not to cure but to preserve or improve remaining vision, allowing patients to regain independence in daily activities.
Prevention and Management of Macular Disease
While macular translocation is a surgical remedy for advanced cases, prevention and early management play a crucial role in reducing the need for such invasive treatment.
Preventive Measures:
-
Quit Smoking: Smoking doubles the risk of macular degeneration progression.
-
Balanced Nutrition: Diets rich in green leafy vegetables, fish oils, and antioxidants (vitamins C, E, lutein, and zeaxanthin) support retinal health.
-
Manage Systemic Conditions: Control hypertension, cholesterol, and diabetes to maintain retinal blood flow.
-
Eye Protection: Use UV-protective eyewear to minimize light-induced retinal damage.
-
Regular Eye Exams: Early detection of macular changes allows prompt initiation of anti-VEGF therapy.
Post-Operative Management After Macular Translocation:
-
Close Monitoring: Frequent follow-up appointments to monitor healing, retinal reattachment, and macular function.
-
Positioning: Patients may need to maintain a specific head position post-surgery to allow proper healing.
-
Visual Rehabilitation: Adaptation training to adjust to the new visual orientation and maximize residual vision.
-
Medication Compliance: Use of prescribed eye drops and medications to prevent infection, inflammation, and complications.
Effective prevention and long-term management are the key to maintaining the benefits of surgery and reducing the risk of further visual decline.
Complications of Macular Translocation
Macular translocation, while potentially beneficial, is one of the most intricate retinal surgeries and carries a significant risk of complications.
Possible Complications Include:
-
Retinal Detachment: A common risk due to extensive retinal manipulation.
-
Proliferative Vitreoretinopathy (PVR): Abnormal scarring that can cause recurrent detachment.
-
Diplopia (Double Vision): Due to the new position of the macula affecting image alignment.
-
Distorted Vision (Tilted Vision): Some patients experience an altered perception of images after the procedure.
-
Cataract Formation: Acceleration of lens opacity following vitrectomy.
-
Infection or Bleeding: Rare but serious surgical risks.
-
Recurrence of Disease: New abnormal vessel growth may occur under the relocated macula.
To minimize these risks, the procedure is performed by highly trained retinal surgeons, and patients are followed up closely to detect and manage complications promptly.
Living with Macular Translocation
Life after macular translocation involves adjustment, rehabilitation, and long-term care. The recovery journey is gradual and requires patience and commitment.
Early Recovery Phase:
Patients may experience blurred vision initially due to retinal swelling and healing. Visual rehabilitation begins soon after surgery to help the brain adapt to the new macular position. Strict adherence to post-operative instructions - including head positioning, use of prescribed medications, and avoiding strenuous activities - is crucial.
Long-Term Adaptation:
-
Vision may improve gradually over several months as the retina stabilizes.
-
Patients may still require glasses, magnifiers, or low-vision aids for optimal function.
-
Regular eye check-ups ensure that any recurrent disease is detected early.
-
Emotional and psychological adaptation is important; support groups and counseling can help patients adjust to their new vision.
While macular translocation does not restore perfect sight, many patients experience significant improvement in daily activities - being able to read, recognize faces, and maintain independence.
Top 10 Frequently Asked Questions about Macular Translocation Surgery
1. What is macular translocation surgery?
Macular translocation surgery is an advanced retinal procedure designed to treat severe macular diseases, particularly age-related macular degeneration (AMD). In this surgery, the macula-the central part of the retina responsible for sharp, detailed vision-is surgically moved to a healthier part of the retina. This allows light to fall on a region with better-functioning retinal cells, potentially restoring or improving central vision in patients with damaged macular tissue.
2. Who is a candidate for macular translocation?
This surgery is typically recommended for patients with advanced macular degeneration or other central retinal diseases who have significant vision loss and for whom conventional treatments, such as laser therapy or anti-VEGF injections, are no longer effective. Ideal candidates:
-
Have severe central vision loss due to macular disease.
-
Retain healthy peripheral retina.
-
Are otherwise healthy and able to tolerate a complex eye surgery.
A comprehensive eye evaluation and retinal imaging are necessary to confirm eligibility.
3. How is macular translocation surgery performed?
The procedure is performed under local or general anesthesia. The surgeon carefully detaches the retina, rotates or moves the macula to a healthier retinal area, and reattaches the retina using a combination of surgical techniques such as vitrectomy and temporary placement of gas or silicone oil. The goal is to align the macula with functioning photoreceptor cells, improving central vision.
4. What are the benefits of macular translocation?
The main benefits of macular translocation surgery include:
-
Potential improvement in central vision in patients with damaged macula.
-
Reduction in the progression of vision loss associated with advanced macular degeneration.
-
Better quality of life through improved ability to read, recognize faces, and perform other tasks requiring detailed vision.
While it may not fully restore normal vision, it can significantly enhance functional vision in selected patients.
5. Is macular translocation surgery painful?
The surgery itself is performed under anesthesia, so patients do not feel pain during the procedure. After surgery, mild discomfort, eye redness, or irritation may occur. Pain is usually manageable with prescribed medications and typically subsides within a few days.
6. What are the risks and complications of macular translocation?
Like any eye surgery, macular translocation carries potential risks, including:
-
Retinal detachment or tears.
-
Bleeding inside the eye.
-
Infection (endophthalmitis).
-
Formation of cataracts.
-
Partial or incomplete visual improvement.
Surgeons carefully evaluate each patient and use advanced techniques to minimize these risks. Regular follow-up is crucial to detect and manage complications early.
7. What is the recovery process like after macular translocation surgery?
Recovery can take several weeks to months. Patients may be required to maintain a specific head position for several days if gas bubbles are used in the eye. Vision may gradually improve over time, but full visual recovery can take months. Follow-up visits with the retina specialist are essential to monitor healing, retinal attachment, and the overall function of the translocated macula.
8. How much improvement in vision can be expected?
Visual outcomes vary depending on the extent of macular damage and the patient’s overall eye health. Some patients experience significant improvement in central vision, while others may see only moderate gains. Peripheral vision usually remains unchanged. Realistic expectations are important, and your surgeon will discuss likely outcomes based on your individual condition.
9. Will I need medications after surgery?
Yes. Post-operative care often includes:
-
Anti-inflammatory eye drops to reduce swelling.
-
Antibiotic eye drops to prevent infection.
-
Sometimes medications to reduce intraocular pressure or control other eye conditions.
Adherence to the prescribed regimen is essential to ensure optimal healing and prevent complications.
10. How much does macular translocation surgery cost, and is it covered by insurance?
The cost of macular translocation depends on factors such as the hospital, surgeon’s expertise, and post-operative care. This is generally considered a specialized procedure and may be expensive. Coverage varies by insurance provider, and some plans may cover the procedure if deemed medically necessary. Patients should consult their insurance company and hospital financial counselors to understand coverage, co-pays, and potential out-of-pocket expenses.


