Introduction to Nasal Polyp Removal
Nasal polyps are soft, painless, benign growths that develop in the lining of the nasal passages and sinus cavities. They arise primarily due to chronic inflammation, often associated with conditions such as chronic sinusitis, allergic rhinitis, asthma, and immune system disorders. Though they are non-cancerous, their presence can have a profound effect on daily life. Individuals with nasal polyps often experience chronic nasal obstruction, difficulty breathing through the nose, loss of smell (anosmia), post-nasal drip, recurrent sinus infections, headaches, and facial pressure. These symptoms can significantly impact sleep quality, sense of taste, and overall wellbeing.
Small polyps may remain unnoticed for years. However, when they enlarge or multiple polyps form, they can obstruct nasal airflow and sinus drainage. At this stage, surgical removal becomes an essential intervention. Nasal polyp removal is typically performed via endoscopic sinus surgery, a minimally invasive procedure conducted through the nostrils using a small camera and specialized surgical instruments. This approach avoids external incisions, allows precise removal, and helps restore normal sinus function.
The main objectives of nasal polyp removal include improving breathing, restoring the sense of smell, reducing chronic infections, enabling effective medication delivery to the sinuses, and enhancing the patient's quality of life. It is important to note that removal addresses the symptom-causing growths but does not cure the underlying chronic inflammation, so ongoing management is necessary to prevent recurrence.
Understanding nasal polyps, their causes, symptoms, treatment options, and post-treatment management is critical for patients and caregivers. This guide will explore all aspects in detail to provide a comprehensive resource on nasal polyp removal.
Causes and Risk Factors of Nasal Polyps
The formation of nasal polyps is primarily driven by chronic inflammation in the nasal and sinus mucosa. While the exact mechanism is not fully understood, persistent inflammation leads to edema (swelling) of the mucosal tissue, eventually forming soft, fluid-filled sac-like growths known as polyps. The risk of polyp development is influenced by several factors, including genetics, immune responses, environmental exposures, and underlying medical conditions.
Medical Conditions That Increase Risk
-
Chronic Rhinosinusitis (CRS): Persistent inflammation of the nasal and sinus lining is the most common contributor to polyp formation. Patients with CRS often have ongoing congestion, infections, and tissue changes that predispose to polyp growth.
-
Allergic Rhinitis: Individuals with allergies experience repeated immune responses in the nasal mucosa, increasing inflammation and swelling that may eventually lead to polyp development.
-
Asthma: Asthma, particularly eosinophilic asthma, is strongly associated with nasal polyps. Inflammation in the airways often extends to the nasal passages, increasing the likelihood of polyp formation.
-
Aspirin-Exacerbated Respiratory Disease (AERD): Patients with this condition, also known as Samter's triad, develop nasal polyps, asthma, and sensitivity to aspirin or other NSAIDs. These individuals tend to develop more aggressive and recurrent polyps.
Anatomical and Structural Factors
-
Deviated Nasal Septum or Narrow Sinus Openings: Structural abnormalities can impair sinus drainage and airflow, creating conditions conducive to chronic inflammation and polyp formation.
-
Previous Sinus Surgery: Scar tissue or altered anatomy may increase the risk of recurrence or new polyp development in some cases.
Environmental and Lifestyle Factors
-
Allergens and Pollutants: Exposure to environmental irritants such as dust, smoke, chemicals, or pollution can aggravate nasal inflammation and contribute to polyp growth.
-
Smoking: Smoking irritates the nasal lining, worsens inflammation, and increases susceptibility to polyp formation.
Genetic and Immune Factors
-
Immune Dysregulation: Certain patients have overactive type 2 immune responses, elevated eosinophils, or high IgE levels, which increase inflammation and polyp risk.
-
Family History: Genetics may play a role, with individuals having family members with nasal polyps being more predisposed.
Recognizing these risk factors is important not only for understanding why polyps develop but also for preventing recurrence after treatment. Management strategies often focus on controlling underlying conditions, reducing exposure to triggers, and maintaining long-term nasal health.
Symptoms and Signs of Nasal Polyps
Symptoms of nasal polyps can range from mild to severe, depending on the size, number, and location of the growths. They often develop slowly and may not be noticed until they interfere with breathing, smell, or quality of life.
Common Symptoms
-
Nasal Congestion or Blockage: Most patients report difficulty breathing through one or both nostrils. Blockage is usually persistent and worsens over time.
-
Reduced Sense of Smell (Hyposmia) or Complete Loss (Anosmia): Obstruction of airflow through the olfactory region leads to decreased smell, which can also reduce taste perception.
-
Runny Nose or Post-Nasal Drip: Impaired sinus drainage leads to excess mucus accumulation and post-nasal drip.
-
Frequent Sneezing or Allergy-Like Symptoms: Particularly in patients with underlying allergic rhinitis.
-
Facial Pressure, Fullness, or Headache: Accumulation of mucus in blocked sinuses can cause discomfort or pain.
-
Sleep Disturbances: Difficulty breathing through the nose may lead to snoring or poor-quality sleep.
Clinical Signs
-
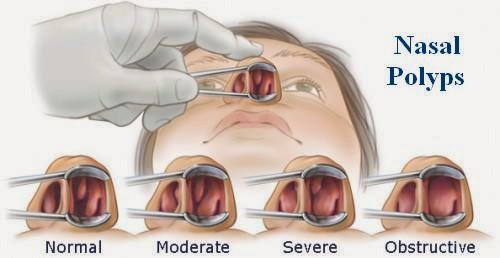
Polyps appear as pale, smooth, grape-like swellings inside the nasal passages.
-
Usually bilateral, but occasionally unilateral polyps may require further investigation to rule out tumors.
-
In severe cases, polyps can completely obstruct sinus openings, leading to recurrent infections.
Early recognition of these symptoms is essential. Patients should consult an ENT specialist if symptoms persist, worsen, or significantly impair quality of life.
Diagnosis of Nasal Polyp Removal
Accurate diagnosis of nasal polyps is a multi-step process involving patient history, physical examination, imaging, and laboratory tests.
Medical History
-
Detailed evaluation of symptoms (nasal congestion, sinus infections, loss of smell, allergies, asthma).
-
Review of prior treatments, medication use, and response to therapy.
-
Assessment of aspirin/NSAID sensitivity or other immune disorders.
Physical Examination and Endoscopy
-
Nasal endoscopy allows direct visualization of polyps, assessment of their size, number, and location.
-
Helps differentiate between nasal polyps and other nasal masses or tumors.
Imaging Studies
-
CT scans of the paranasal sinuses evaluate the extent of polyp involvement, detect anatomical abnormalities, and guide surgical planning.
-
Helps identify blocked sinus pathways, thickened sinus lining, and complications such as bone erosion (rare).
Laboratory and Allergy Testing
-
Blood tests may assess eosinophil levels and inflammatory markers.
-
Allergy testing can identify triggers that exacerbate nasal inflammation.
Assessment of Treatment Response
-
Response to medical therapy (steroids, sprays, biologics) helps determine whether surgical removal is indicated.
-
Patients who fail medical management or have severe obstruction are candidates for polyp removal.
Pre-Surgical Planning
-
ENT surgeons review imaging, history, and endoscopic findings to develop a precise surgical plan.
-
Patient education and discussion of risks, benefits, and expectations are essential.
Treatment Options for Nasal Polyp Removal
Treatment involves both medical management and surgical removal when necessary. Modern approaches emphasize combined therapy for long-term success.
Medical Management
-
Intranasal Corticosteroids: First-line therapy to reduce inflammation and shrink polyps. Daily use is recommended for maintenance.
-
Oral Corticosteroids: Short courses for severe cases; limited by systemic side effects.
-
Saline Irrigations: High-volume nasal rinses improve mucus clearance, reduce inflammation, and enhance drug delivery.
-
Biologic Therapies: Targeted agents like dupilumab or mepolizumab are used in severe, recurrent polyps, particularly in patients with asthma or type 2 inflammation.
-
Management of Comorbidities: Allergies, asthma, and chronic sinus infections must be controlled for optimal outcomes.
Surgical Removal
-
Endoscopic Sinus Surgery (ESS): Standard procedure, performed through the nostrils using a camera and instruments. Removes polyps, restores sinus drainage, and improves airflow.
-
In-Office Polypectomy: For smaller, accessible polyps, minor removal may be performed under local anesthesia.
-
Indications for Surgery: Persistent obstruction, failure of medical therapy, recurrent infections, loss of smell, or quality of life impact.
-
Postoperative Care: Regular saline irrigations, topical corticosteroids, follow-up endoscopy, and long-term monitoring for recurrence.
-
Recurrence Risk: Polyps often recur; combination of surgery and maintenance therapy provides the best long-term control.
Prevention and Management of Nasal Polyp Removal
Even after removal, nasal polyps may recur. Effective long-term strategies include:
-
Controlling Allergies and Asthma: Proper management reduces inflammation and risk of recurrence.
-
Avoiding Irritants: Smoke, pollutants, and allergens can exacerbate mucosal swelling.
-
Daily Nasal Hygiene: Saline irrigations maintain clear nasal passages.
-
Ongoing Use of Topical Steroids: Reduces inflammation and prevents regrowth.
-
Regular Follow-Up: ENT visits and endoscopic evaluations monitor for early recurrence.
-
Lifestyle Modifications: Humidified environments, avoidance of triggers, good sleep hygiene.
-
Patient Education: Understanding the chronic nature of nasal polyps helps set realistic expectations.
Complications of Nasal Polyps and Their Removal
Complications associated with nasal polyps-and their surgical removal-can significantly impact quality of life if not recognized and managed properly. Complications arise both from the presence of untreated polyps and as potential risks following surgical intervention.
Complications of Untreated Polyps
-
Persistent nasal obstruction and congestion
-
Loss of smell and taste
-
Recurrent sinus infections
-
Sleep disturbances
-
Asthma exacerbations
-
Rarely, spread of infection to orbit or brain
Complications of Surgical Removal
-
Bleeding, infection, or crusting
-
Adhesions or scar tissue
-
Injury to surrounding structures (orbit, skull base, optic nerve)
-
Recurrence of polyps, possibly requiring revision surgery
-
Temporary alteration of smell or congestion
Careful surgical planning and postoperative care minimize these risks.
Living with the Condition of Nasal Polyp Removal
Living with nasal polyps requires a proactive approach, both before and after removal.
-
Postoperative Recovery: Mild bleeding, congestion, and crusting are common; regular irrigations and follow-ups are essential.
-
Adherence to Therapy: Topical corticosteroids and saline rinses prevent recurrence.
-
Lifestyle Measures: Avoiding allergens, smoking, and irritants, maintaining good sleep hygiene.
-
Monitoring for Recurrence: Early recognition of symptoms allows timely intervention.
-
Managing Comorbidities: Asthma and allergies must be controlled for optimal outcomes.
-
Psychological Wellbeing: Support for the emotional impact of chronic nasal obstruction and repeated surgeries.
With proper care, most patients experience significant improvement in breathing, smell, sleep quality, and overall quality of life.
Top 10 Frequently Asked Questions about Nasal Polyp Removal
1. What is nasal polyp removal surgery?
Nasal polyp removal, also known as polypectomy, is a surgical procedure to remove benign growths (polyps) from the lining of the nasal passages or sinuses. Nasal polyps can cause obstruction, chronic sinus infections, difficulty breathing, loss of smell, and recurring sinus inflammation. Removal of polyps helps restore normal nasal airflow and improves overall sinus health.
2. Why is nasal polyp removal necessary?
Surgery is recommended when nasal polyps:
-
Cause persistent nasal congestion or blockage
-
Lead to chronic sinus infections
-
Do not respond to medications such as nasal steroids or antibiotics
-
Affect sense of smell or taste
-
Contribute to sleep disturbances, including snoring or sleep apnea
The goal of removal is to relieve symptoms, prevent recurrence of infections, and improve quality of life.
3. Who is a candidate for nasal polyp removal?
Candidates typically include individuals with:
-
Moderate to large nasal polyps causing obstruction
-
Chronic sinusitis unresponsive to medications
-
Frequent sinus infections or nasal congestion affecting daily activities
-
Difficulty breathing through the nose or persistent post-nasal drip
Your ENT specialist will evaluate the size, location, and number of polyps using nasal endoscopy or imaging studies before recommending surgery.
4. How is nasal polyp removal performed?
Nasal polyp removal is usually performed under local or general anesthesia, depending on the extent of polyps and patient preference. There are two common surgical techniques:
-
Endoscopic sinus surgery: A small camera (endoscope) is inserted into the nasal passages to guide instruments and remove polyps. This is minimally invasive and avoids external incisions.
-
Traditional polypectomy: A small instrument or suction device removes polyps directly from the nasal cavity.
The procedure usually takes 30–90 minutes, depending on the number and size of polyps.
5. Is nasal polyp removal painful?
During the procedure, anesthesia ensures the patient feels no pain. Post-operatively, mild discomfort, nasal congestion, and a feeling of pressure are common. Pain is usually managed with over-the-counter or prescribed pain medications, and most patients report relief within a few days. Some minor bleeding or nasal crusting may occur temporarily.
6. What are the risks and complications of nasal polyp removal?
While generally safe, potential risks include:
-
Mild to moderate bleeding from the nasal passages
-
Infection
-
Rare injury to surrounding structures, including the eyes or skull base
-
Recurrence of nasal polyps
-
Persistent nasal congestion or altered sense of smell
Following post-operative instructions and using prescribed medications helps reduce risks and prevent complications.
7. What is the recovery process after nasal polyp removal?
Recovery usually includes:
-
Rest for a few days and avoiding strenuous activities for 1–2 weeks
-
Nasal saline irrigation to clear crusting and promote healing
-
Avoiding nose blowing and exposure to dust or allergens during early recovery
-
Follow-up visits to remove any nasal packing and monitor healing
Most patients experience improved breathing and reduced congestion within a few weeks.
8. Will my nasal polyps return after surgery?
Nasal polyps can recur, especially in patients with chronic sinusitis, allergies, or asthma. Post-operative management, including nasal steroid sprays, allergy control, and regular ENT follow-up, helps minimize recurrence. In some cases, additional surgeries may be needed if polyps grow back.
9. How long does it take for symptoms to improve after surgery?
Many patients notice relief from nasal blockage and improved breathing within a few days to a couple of weeks. Full recovery, including reduction in inflammation and restoration of normal nasal function, may take 4–6 weeks. Improvement in sense of smell may occur gradually over this period.
10. How much does nasal polyp removal cost, and is it covered by insurance?
The cost of nasal polyp removal depends on the hospital, surgeon, type of anesthesia, and post-operative care. Most medically necessary polyp removal procedures are covered by insurance, including hospital fees, surgical fees, and medications. Cosmetic or non-essential procedures may not be covered. Patients should confirm coverage, co-pays, and out-of-pocket expenses with their insurance provider.


