Introduction to Optical Internal Urethrotomy (OTU) - Endoscopic Surgery
Optical Internal Urethrotomy (OTU) is a minimally invasive endoscopic procedure used to treat urethral strictures. Urethral strictures are narrowing of the urethra due to scar tissue formation, which can cause difficulty in urination, urinary retention, infections, and other complications. OTU involves the insertion of a specialized endoscopic instrument called a urethrotome into the urethra to directly visualize the stricture and incise it to restore normal urine flow. This procedure is considered less invasive than open urethral surgery, offering shorter recovery times, reduced postoperative pain, and minimal external scarring.
The procedure is primarily indicated for short, non-complex urethral strictures and is often performed under regional or general anesthesia. It allows urologists to precisely target the stricture under direct visualization, reducing the risk of damage to surrounding tissues. Patients benefit from rapid relief of urinary obstruction, improved quality of life, and the possibility of performing the surgery on an outpatient basis. Modern advances in endoscopic technology have made OTU a safe, effective, and widely accepted treatment option for select cases of urethral stricture.
Causes and Risk Factors of Urethral Strictures Requiring OTU
Urethral strictures can develop due to a variety of causes, and understanding these underlying factors helps guide treatment planning.
Causes of Urethral Strictures
-
Trauma: Injury to the urethra, including pelvic fractures or blunt trauma to the perineum, can trigger scar formation leading to narrowing.
-
Infections: Chronic urinary tract infections, especially untreated sexually transmitted infections like gonorrhea, can result in fibrosis and stricture formation.
-
Iatrogenic Causes: Medical interventions such as catheterization, previous urethral surgeries, or endoscopic procedures can cause urethral trauma and subsequent scarring.
-
Inflammatory Conditions: Chronic inflammatory disorders like lichen sclerosus or balanitis can contribute to stricture development.
-
Congenital Anomalies: Rarely, some patients may have congenital narrowing or malformations of the urethra that necessitate surgical intervention.
Risk Factors
-
History of recurrent urinary tract infections.
-
Prior instrumentation or catheterization of the urethra.
-
Trauma to the pelvis or urethra.
-
Chronic inflammatory conditions affecting the genital area.
-
Age-related changes leading to tissue fibrosis.
Understanding these causes and risk factors allows physicians to predict the likelihood of recurrence and determine whether OTU is suitable or if alternative treatments should be considered.
Symptoms and Signs Indicating OTU
Patients with urethral strictures often present with both functional and anatomical symptoms that interfere with normal urination.
Common Symptoms
-
Difficulty initiating urination (hesitancy).
-
Weak or slow urine stream.
-
Incomplete bladder emptying.
-
Increased frequency or urgency of urination.
-
Painful urination (dysuria) or urinary tract infections.
-
Straining during urination or prolonged voiding time.
Clinical Signs
-
Palpable bladder distension in chronic cases due to urinary retention.
-
Narrowed urinary stream observed during micturition.
-
Post-void residual urine detected on imaging or catheterization.
-
Signs of chronic infection or irritation, such as suprapubic discomfort or hematuria.
Timely recognition of these symptoms is critical for preventing complications like recurrent infections, bladder damage, or kidney impairment, and helps identify patients who are candidates for OTU.
Diagnosis of Urethral Strictures for OTU
Accurate diagnosis of urethral strictures is essential to plan OTU effectively.
Medical History and Physical Examination
-
Assess patient history for trauma, infections, catheterization, previous surgeries, and urinary symptoms.
-
Conduct a genital and perineal examination to identify potential stricture sites, scarring, or palpable abnormalities.
Diagnostic Tests
-
Uroflowmetry: Measures urine flow rate to detect obstruction.
-
Retrograde Urethrogram (RUG): Imaging study where contrast is injected to visualize stricture location and length.
-
Voiding Cystourethrogram (VCUG): Evaluates bladder function and urethral passage during urination.
-
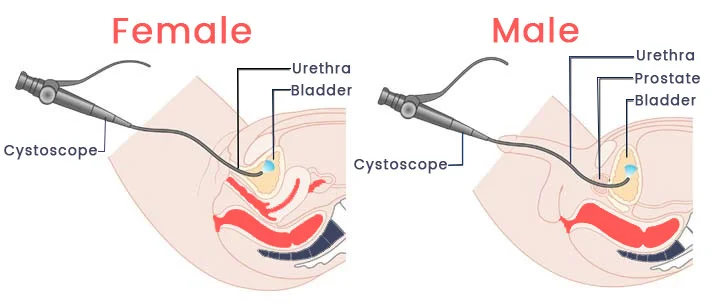
Cystoscopy: Endoscopic visualization of the urethra to confirm stricture and assess severity.
-
Ultrasound or MRI: May be used in complex cases to evaluate surrounding tissue or post-traumatic strictures.
Correct diagnosis allows the surgeon to choose the appropriate approach, anticipate technical challenges, and counsel the patient on potential outcomes and risks.
Treatment Options of Optical Internal Urethrotomy (OTU)
Optical Internal Urethrotomy (OTU)
-
Procedure: OTU involves inserting a urethrotome through the urethra to visualize the stricture directly. A precise incision is made to release the scar tissue and widen the urethral lumen.
-
Anesthesia: The procedure is typically performed under general or regional anesthesia.
-
Duration: Usually performed within 30-60 minutes for simple strictures.
-
Advantages: Minimally invasive, reduced hospital stay, faster recovery, low external scarring, and improved immediate urinary flow.
Adjunctive Treatments
-
Catheterization: A urinary catheter may be placed post-operatively to maintain urethral patency during healing.
-
Dilation Therapy: In some cases, gradual urethral dilation may complement OTU to prevent recurrence.
Alternative Treatments
-
Open Urethroplasty: Considered for long, complex, or recurrent strictures where OTU is less effective.
-
Laser Urethrotomy: Uses laser energy to incise the stricture, offering precise control and reduced bleeding.
-
Endoscopic Balloon Dilation: Occasionally used for short strictures, though recurrence rates are higher than OTU.
The choice of treatment depends on stricture length, location, prior interventions, and patient-specific factors.
Prevention and Management of Urethral Strictures
Prevention
-
Avoid unnecessary or prolonged catheterization.
-
Promptly treat urinary tract infections to reduce scarring.
-
Use proper techniques during instrumentation to minimize trauma.
-
Manage chronic inflammatory conditions such as balanitis or lichen sclerosus.
Post-Operative Management
-
Maintain catheter for recommended duration post-OTU to allow healing.
-
Follow up with regular uroflowmetry or imaging to detect early recurrence.
-
Avoid activities that may traumatize the urethra until fully healed.
-
Hydration and infection prevention measures are important to reduce the risk of recurrence.
Effective prevention and management reduce recurrence rates, improve long-term urinary function, and maintain patient quality of life.
Complications of Optical Internal Urethrotomy (OTU)
While OTU is considered safe and minimally invasive, complications can occur:
-
Immediate Complications: Bleeding, infection, catheter-related issues, or urinary retention.
-
Intermediate Complications: Urethral irritation, dysuria, hematuria, or discomfort during urination.
-
Long-Term Complications: Recurrence of the stricture (common in some patients), urethral scarring, and in rare cases, fistula formation.
Proper surgical technique, patient selection, and post-operative care are critical to minimizing these risks. Patients should be counseled about recurrence rates and the possibility of additional interventions if strictures recur.
Living with the Condition of Optical Internal Urethrotomy (OTU)
Patients undergoing OTU experience significant improvement in urinary symptoms, quality of life, and comfort. Recovery is generally rapid, with most patients resuming normal activities within a few days to weeks, depending on post-operative catheterization and healing.
Lifestyle Considerations
-
Avoid trauma or activities that may injure the urethra during recovery.
-
Maintain adequate hydration to reduce infection risk and promote smooth urinary flow.
-
Follow-up evaluations are essential to detect early recurrence and ensure long-term success.
Psychological and Social Impact
Chronic urinary obstruction can cause stress, anxiety, and social embarrassment. Successful OTU restores urinary function, alleviates discomfort, and improves patient confidence. Patients report enhanced quality of life and increased satisfaction with daily activities post-procedure.
Long-Term Outlook
Most patients experience sustained improvement after OTU, though recurrence is possible, especially for longer strictures or in patients with ongoing risk factors. Long-term monitoring, preventive care, and lifestyle modifications contribute to maintaining urethral health and minimizing complications.
Top 10 Frequently Asked Questions about Optical Internal Urethrotomy (OTU) - Endoscopic Surgery
1. What is Optical Internal Urethrotomy (OTU)?
Optical Internal Urethrotomy (OTU) is a minimally invasive endoscopic procedure used to treat urethral strictures-narrowing of the urethra that obstructs urine flow. During the procedure, a specialized instrument called a urethrotome is inserted into the urethra through the urinary opening to cut or incise the stricture, widening the passage and restoring normal urine flow. OTU avoids external incisions and provides a faster recovery compared to open surgery.
2. Why is OTU performed?
OTU is indicated for patients who experience:
-
Difficulty or pain while urinating
-
Weak urinary stream or straining to pass urine
-
Recurrent urinary tract infections due to obstruction
-
Retention of urine or incomplete bladder emptying
-
Strictures caused by trauma, infection, surgery, or inflammation
The procedure helps relieve obstruction, improve urinary flow, prevent complications, and enhance the patient’s quality of life.
3. Who is a candidate for OTU?
Ideal candidates are patients with:
-
Short urethral strictures (usually less than 2 cm in length)
-
Strictures located in the bulbar or penile urethra
-
No severe fibrosis or long segment narrowing, which may require open urethroplasty
-
Good overall health to undergo anesthesia and endoscopic surgery
A thorough evaluation, including uroflowmetry, retrograde urethrogram, and cystoscopy, helps determine suitability.
4. How is Optical Internal Urethrotomy performed?
The procedure is done under general or spinal anesthesia. Steps include:
-
Insertion of a cystoscope or urethrotome through the urinary opening into the urethra.
-
Visualization of the stricture using endoscopic camera guidance.
-
Incision or incision of the narrowed urethral segment with a cold knife or laser.
-
Placement of a temporary catheter to keep the urethra open during healing.
The procedure usually takes 30-60 minutes and is typically performed on an outpatient basis or with a short hospital stay.
5. What are the benefits of OTU?
-
Minimally invasive with no external incisions
-
Rapid recovery and short hospital stay
-
Relief from urinary obstruction and improved urine flow
-
Reduced pain compared to open urethral surgery
-
Option to repeat the procedure if the stricture recurs
OTU can significantly improve urinary function and overall quality of life for patients with urethral strictures.
6. Is OTU painful?
Patients are under anesthesia during the procedure, so no pain is felt during surgery. Post-operative discomfort is generally mild and may include:
-
Burning or irritation while urinating
-
Mild pain around the urinary opening or perineal area
-
Temporary urinary frequency or urgency
Pain is usually managed with oral pain medications and typically subsides within a few days.
7. What are the risks and complications of OTU?
While OTU is generally safe, potential risks include:
-
Bleeding from the incision site
-
Infection or urinary tract infection
-
Recurrence of the urethral stricture (common, especially in longer strictures)
-
Rare injury to surrounding urethral tissue
-
Difficulty in passing urine immediately after catheter removal
Following post-operative care and catheter management instructions reduces the likelihood of complications.
8. What is the recovery process after OTU?
Recovery is relatively quick:
-
Catheter duration: A catheter is usually kept in place for 5-7 days to support healing.
-
Activity: Light activities can usually be resumed immediately, but heavy lifting or strenuous activity should be avoided for 1-2 weeks.
-
Hydration: Adequate fluid intake helps flush the urinary system.
-
Follow-up: Regular follow-up visits and uroflowmetry tests monitor healing and detect recurrence early.
Most patients notice improved urine flow immediately after catheter removal, with complete healing within a few weeks.
9. Can urethral strictures recur after OTU?
Yes, recurrence is a known limitation of OTU, especially in patients with longer or more fibrotic strictures. Short bulbar strictures have a higher success rate. Recurrence may require:
-
Repeat OTU
-
Self-dilation or intermittent catheterization
-
Open urethroplasty (for recurrent or long strictures)
Regular follow-up is essential to monitor for early signs of stricture recurrence.
10. How much does OTU cost, and is it covered by insurance?
The cost of OTU depends on factors such as hospital, surgeon expertise, anesthesia, and post-operative care. Many health insurance plans cover OTU when it is medically necessary to treat urethral obstruction or prevent urinary complications. Patients should confirm coverage, co-pays, and out-of-pocket expenses with their insurance provider before scheduling the procedure.


