Introduction to Ossiculoplasty
Ossiculoplasty is a sophisticated surgical procedure designed to restore the ossicular chain in the middle ear, which comprises the malleus, incus, and stapes. These tiny bones play a vital role in transmitting sound vibrations from the eardrum to the inner ear, amplifying and efficiently conducting sound. Disruption of this chain—caused by chronic ear infections, trauma, congenital anomalies, or previous surgeries—leads to conductive hearing loss, significantly affecting communication and quality of life. The primary aim of ossiculoplasty is to re-establish the mechanical continuity and function of the ossicular chain to improve hearing and reduce the air-bone gap, while maintaining the delicate balance of middle ear anatomy.
The procedure can involve mobilizing and repositioning existing ossicles or replacing them entirely with autografts or prosthetic devices, depending on the degree of damage. Modern surgical advancements, including the use of biocompatible materials such as titanium, hydroxyapatite, and cartilage grafts, have significantly improved the predictability and success rates of ossiculoplasty. Beyond hearing restoration, ossiculoplasty seeks to enhance patients' quality of life, enabling normal auditory experiences, better social interaction, and reduced reliance on hearing aids. The success of this procedure is influenced by preoperative evaluation, surgical technique, choice of prosthesis or graft, middle ear status, and postoperative care.
Causes and Risk Factors of Ossiculoplasty
Ossiculoplasty is indicated in patients with ossicular chain discontinuity, erosion, fixation, or absence. Understanding the underlying causes and risk factors is essential for planning treatment and predicting outcomes.
Common Causes
-
Chronic Otitis Media: Persistent middle ear infection can erode the ossicles, especially the long process of the incus, leading to conductive hearing loss. This is the most common indication for ossiculoplasty.
-
Otosclerosis: Abnormal bone remodeling of the stapes footplate causes stapes fixation, which can disrupt sound transmission.
-
Trauma: Blunt force or penetrating injuries can fracture or dislocate the ossicular chain.
-
Previous Ear Surgery: Surgical procedures such as tympanoplasty or mastoidectomy can inadvertently damage the ossicles.
-
Congenital Abnormalities: Developmental malformations may result in absent or malformed ossicles requiring reconstruction.
-
Tympanosclerosis: Calcification of middle ear tissues can immobilize the ossicles, affecting sound conduction.
Risk Factors
The success of ossiculoplasty can be affected by various risk factors, including chronic infection, poor middle ear ventilation, Eustachian tube dysfunction, prior surgeries, mastoid pneumatization deficits, smoking, systemic diseases like diabetes, and poor nutritional status. Extensive ossicular destruction, poor mucosal health, and a hostile middle ear environment increase the risk of prosthesis extrusion, persistent hearing deficits, and need for revision surgery. Identifying these risk factors preoperatively allows the surgeon to optimize outcomes and counsel patients about realistic expectations.
Symptoms and Signs Indicating the Need for Ossiculoplasty
Symptoms and signs indicating the need for ossiculoplasty mainly involve conductive hearing loss resulting from damage or disruption of the middle ear ossicular chain. Patients typically present with hearing difficulties related to chronic ear disease or trauma, where reconstructive surgery can improve sound conduction.
Key Symptoms Indicating Ossiculoplasty
-
Conductive hearing loss:
-
Difficulty hearing sounds clearly, especially in noisy environments, often described as muffled hearing or reduced volume. Hearing tests typically show an air-bone gap on audiometry, indicating middle ear mechanical problem rather than nerve damage.
-
History of chronic ear infections (chronic otitis media):
-
Recurrent or longstanding infections can erode ossicles, causing progressive hearing loss and persistent ear discharge.
-
-
Previous middle ear surgery:
-
Patients with persistent or worsened hearing loss due to scarring or prior ossicular damage post-tympanoplasty or mastoidectomy may require ossiculoplasty revision.
-
-
Traumatic ossicular disruption:
-
Hearing loss following head injury, barotrauma, or temporal bone fracture involving the ossicular chain.
-
-
Cholesteatoma:
-
A destructive skin cyst in the middle ear that erodes and destroys ossicles; surgical removal followed by ossiculoplasty is often necessary.
-
-
Auditory symptoms:
-
Some may experience tinnitus (ringing in ears), ear fullness, or occasional dizziness/imbalance, but the primary indication remains hearing loss.
-
-
No improvement with hearing aids:
-
Patients unable to tolerate or who do not get sufficient benefit from hearing aids due to middle ear structural problems might opt for ossiculoplasty.
-
Diagnosis and Preoperative Evaluation
A thorough diagnostic and preoperative evaluation is critical to maximize the success of ossiculoplasty. Key steps include:
-
Detailed History: Documentation of chronic ear infections, prior surgeries, trauma history, duration and progression of hearing loss, and systemic health issues.
-
Otoscopic and Microscopic Examination: Assessment of the tympanic membrane, middle ear mucosa, ossicular chain visibility, perforations, retraction, cholesteatoma, and tympanosclerosis.
-
Audiometric Testing: Pure-tone audiometry, speech audiometry, and tympanometry assess the air-bone gap, quantify hearing loss, and confirm conductive versus sensorineural components.
-
Imaging: High-resolution CT of the temporal bone evaluates ossicular integrity, mastoid pneumatization, presence of disease (e.g., cholesteatoma), and suitability for prosthesis placement.
-
Risk Assessment: Middle ear risk indices, such as MERI or OOPS, predict the likelihood of successful hearing restoration based on the condition of the ear, ossicular status, prior surgeries, and presence of infection.
-
Patient Counseling: Preoperative discussions address expected hearing outcomes, procedural risks, prosthesis options, rehabilitation requirements, and potential for revision surgery.
Preoperative preparation, including ensuring the ear is infection-free, optimizing middle ear mucosa, and addressing systemic health factors, improves surgical outcomes and reduces complication rates.
Treatment Options of Ossiculoplasty
The treatment options for ossiculoplasty involve a range of surgical techniques for reconstructing or replacing the damaged ossicular chain in the middle ear to improve conductive hearing loss. The exact approach depends on which ossicles are affected, the extent of the damage, and the patient's anatomy.
Ossiculoplasty techniques vary depending on ossicular status and the middle ear environment. The main approaches include:
Surgical Techniques
-
Autograft Ossiculoplasty: Utilizes the patient's own ossicles or cartilage to reconstruct the chain, often preferred when a portion of the ossicles is intact.
-
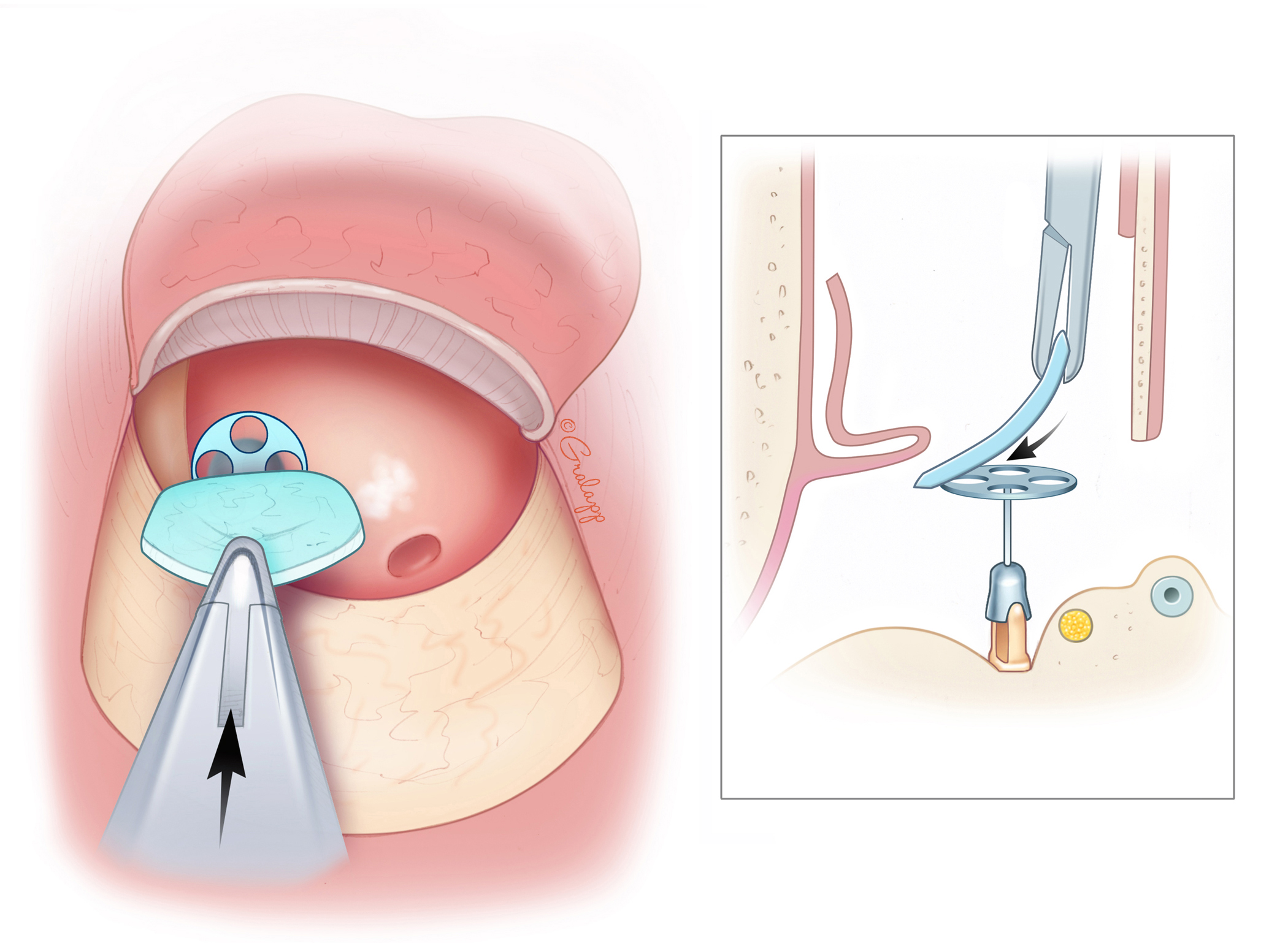
Partial Ossicular Replacement Prosthesis (PORP): Used when the stapes is present and the incus or malleus is damaged.
-
Total Ossicular Replacement Prosthesis (TORP): Indicated when the stapes footplate is the only intact ossicle.
-
Combination Approaches: Mobilization of residual ossicles with prosthetic augmentation to optimize sound transmission.
Materials
-
Titanium Prostheses: Lightweight, biocompatible, and widely used due to low extrusion risk.
-
Hydroxyapatite Prostheses: Offer excellent integration with surrounding tissues.
-
Cartilage or Fascia Grafts: Used to stabilize prostheses or cover them to improve coupling with the tympanic membrane.
Surgical Workflow
-
Access to the middle ear is typically achieved via tympanomeatal flap or endaural approach.
-
Removal of diseased tissue, such as cholesteatoma or granulation tissue, precedes reconstruction.
-
The ossicular chain is assessed; residual ossicles are mobilized if viable.
-
Appropriate prosthesis or graft is placed with precise alignment to restore continuity.
-
The tympanic membrane is closed, and the middle ear is packed as needed.
-
Postoperative monitoring includes audiometric testing and inspection for prosthesis stability and middle ear status.
Successful ossiculoplasty improves hearing thresholds, reduces the air-bone gap, and enhances auditory function. The degree of improvement is influenced by middle ear ventilation, mucosal health, prosthesis positioning, and patient-specific factors.
Prevention and Management After Ossiculoplasty
Prevention and management after ossiculoplasty are essential for a successful recovery, optimal hearing improvement, and minimizing complications such as infection, implant displacement, or sustained hearing loss. The aftercare strategy centers on protecting the surgical repair, careful wound and ear care, activity modification, and vigilant monitoring.
Preoperative Optimization
-
Ensuring the middle ear is dry and free of infection.
-
Managing Eustachian tube dysfunction and optimizing mastoid pneumatization.
-
Addressing systemic health issues and nutritional status.
-
Counseling patients regarding realistic hearing outcomes and potential for adjunctive hearing aids.
Postoperative Care
-
Follow-up visits for packing removal, audiometric assessment, and monitoring prosthesis stability.
-
Protection of the ear from water, trauma, and sudden pressure changes.
-
Prompt management of infection, effusion, or prosthesis displacement.
-
Long-term monitoring for recurrent disease, hearing stability, and prosthesis function.
Ongoing ear care and lifestyle modifications, including avoidance of trauma and control of upper respiratory or sinus infections, are essential for long-term success.
Complications of Ossiculoplasty
While ossiculoplasty is generally safe, complications can occur, including:
-
Prosthesis extrusion or displacement leading to persistent conductive loss.
-
Persistent conductive hearing loss if prosthesis placement is suboptimal or middle ear conditions are unfavorable.
-
Sensorineural hearing loss due to trauma to the inner ear.
-
Tympanic membrane perforation or graft failure, causing recurrent infection or hearing deficits.
-
Infection or otorrhea, particularly in poorly ventilated ears.
-
Revision surgery may be required in cases of prosthesis failure or inadequate hearing improvement.
Meticulous preoperative planning, precise surgical technique, and diligent postoperative follow-up minimize these risks.
Living with the Condition After Ossiculoplasty
After ossiculoplasty, most people experience significant improvements in hearing and quality of life, though the degree and timeline of recovery vary. Living with the condition after the procedure requires patience through the healing period, commitment to follow-up care, and often lifestyle adjustments to protect hearing for the long term.
Short-Term Recovery
-
Pain management, limited ear exposure to water, and avoidance of nose-blowing or heavy lifting are essential in the initial postoperative period.
-
Regular follow-up is required to monitor prosthesis position, remove packing, and assess hearing improvement.
Long-Term Adaptation
-
Most patients experience meaningful improvement in hearing and quality of life.
-
Ongoing monitoring and management of middle ear health are necessary to prevent recurrence or prosthesis issues.
-
Lifestyle adjustments include avoiding trauma, protecting the ear during swimming, and maintaining good ear hygiene.
-
Patients may still require amplification devices for optimal auditory function, depending on individual recovery and residual hearing loss.
Successful long-term outcomes depend on patient adherence, regular monitoring, and proactive management of ear health, ensuring sustained improvement in hearing and communication ability.
Top 10 Frequently Asked Questions about Ossiculoplasty
1. What is ossiculoplasty?
Ossiculoplasty is a surgical procedure that repairs or reconstructs the ossicles, the tiny bones in the middle ear (malleus, incus, and stapes) that transmit sound from the eardrum to the inner ear. Damage to these bones can result from chronic ear infections, trauma, congenital defects, or previous surgeries, leading to hearing loss. Ossiculoplasty restores the continuity of the ossicular chain and improves hearing.
2. Why is ossiculoplasty performed?
Ossiculoplasty is recommended for patients with:
-
Conductive hearing loss caused by damaged ossicles
-
Chronic ear infections leading to erosion or destruction of middle ear bones
-
Trauma to the middle ear
-
Congenital malformations of the ossicles
-
Failed previous ear surgeries affecting the ossicles
The primary goal is to improve hearing by reconstructing the ossicular chain and restoring sound transmission to the inner ear.
3. Who is a candidate for ossiculoplasty?
Ideal candidates include:
-
Patients with conductive hearing loss confirmed through audiometry
-
Individuals with a stable middle ear environment (no active infection)
-
Healthy adults or children able to tolerate anesthesia and surgery
-
Patients with realistic expectations about hearing improvement
A detailed evaluation by an ENT or otologic surgeon, including audiogram and CT scan, is essential to assess the ossicles and middle ear condition.
4. How is ossiculoplasty performed?
The procedure is usually performed under general anesthesia. The surgeon accesses the middle ear through the ear canal or a small incision behind the ear. Depending on the type of damage, ossiculoplasty may involve:
-
Partial ossicular replacement prosthesis (PORP): Replacing part of the ossicular chain.
-
Total ossicular replacement prosthesis (TORP): Replacing the entire chain when all ossicles are damaged.
-
Using the patient's own ossicles or cartilage to reconstruct the chain.
The reconstructed ossicles are carefully positioned to restore sound conduction from the eardrum to the inner ear.
5. What are the benefits of ossiculoplasty?
-
Improvement in hearing and speech perception
-
Reduction of dependence on hearing aids
-
Restoration of middle ear function
-
Enhanced quality of life and communication abilities
-
Prevention of progressive hearing loss due to untreated ossicular damage
Most patients notice a significant improvement in hearing after recovery.
6. Is ossiculoplasty painful?
The procedure is performed under anesthesia, so patients do not feel pain during surgery. Post-operative discomfort may include:
-
Mild ear pain or pressure
-
Temporary dizziness or imbalance
-
Swelling around the ear (if a post-auricular incision was made)
Pain is typically mild and managed with prescription or over-the-counter medications. Discomfort usually subsides within a few days.
7. What are the risks and complications of ossiculoplasty?
While generally safe, potential risks include:
-
Infection in the middle ear
-
Persistent or incomplete hearing improvement
-
Damage to surrounding structures, including the inner ear
-
Prosthesis displacement or extrusion
-
Tinnitus (ringing in the ear)
-
Rare complications such as dizziness or taste disturbances
Careful surgical technique and proper post-operative care reduce these risks significantly.
8. What is the recovery process after ossiculoplasty?
Recovery usually involves:
-
Hospital stay: Often outpatient or 1-2 days depending on the procedure
-
Avoiding water exposure in the ear for several weeks
-
Gradual resumption of normal activities, avoiding heavy lifting or straining
-
Follow-up audiograms to assess hearing improvement
-
Medications: Antibiotics, ear drops, or pain relievers as prescribed
Most patients notice improvement in hearing within weeks, though complete healing may take several months.
9. How much hearing improvement can be expected?
Hearing improvement depends on factors such as:
-
Extent of ossicular damage
-
Type of prosthesis or reconstruction used
-
Health of the eardrum and inner ear
Many patients experience significant improvement, though some may still require hearing aids for optimal hearing in certain situations. Realistic expectations are important.
10. How much does ossiculoplasty cost, and is it covered by insurance?
The cost depends on hospital fees, surgeon expertise, anesthesia, and post-operative care. Ossiculoplasty is usually considered medically necessary for hearing restoration and is often covered by health insurance, including hospital charges, surgical fees, and audiology follow-ups. Cosmetic or elective procedures unrelated to hearing improvement may not be covered. Patients should check with their insurance provider for coverage details, co-pays, and out-of-pocket costs.


