Introduction to Otoclisis
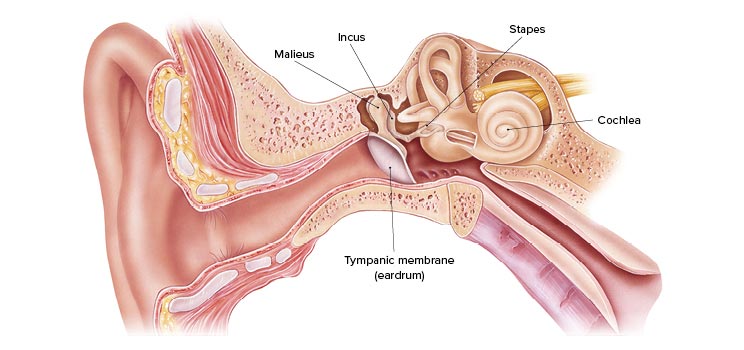
Otoclisis refers to a clinical condition / treatment protocol (depending on source) involving the ear-specifically the auditory canal, middle ear, or associated structures. It may denote a therapeutic irrigation of the ear canal (sometimes called “otic lysis” or “otoclysis”) or less commonly a condition of the ear that requires special clearance. In this context we will treat it as a condition requiring medical attention and possible treatment. The inner workings of the ear - the external auditory canal, tympanic membrane, middle ear and Eustachian tube - are finely balanced systems that rely on proper ventilation, drainage, ear-wax (cerumen) protection, skin integrity, and absence of pathogens. When any of these are disturbed, treatment such as otoclisis may be required.
Often ear disorders present with symptoms of fullness, hearing change, discharge, itching, or pain; the correct diagnosis and management restore hearing, relieve discomfort and prevent long term damage. This article will provide a broad and detailed review of what otoclisis is (or when such treatment is indicated), what causes it, the risk profile, symptoms and signs, how it is diagnosed, different treatment options including the procedure itself (if relevant), preventive strategies, possible complications, and guidance on living with this condition or after-care of the procedure. The aim is to equip patients, caregivers, and medical website readers with up-to-date, clear information about otoclisis so that they understand when to seek help, what to expect, and how to manage it.
Causes and Risk Factors of Otoclisis
The need for otoclisis (or the underlying ear condition requiring such treatment) may arise due to a variety of causes, many of which involve disturbances of the ear canal, middle ear or Eustachian tube environment.
Causes
-
Excess moisture or water exposure (swimming, diving, humid climates) leading to ear canal skin maceration and infection.
-
Trauma or micro-trauma to the ear canal (using cotton-buds, ear-phones, hearing aids that irritate skin) which disrupts cerumen layer and skin barrier.
-
Accumulation of cerumen (ear-wax) or foreign bodies that block drainage, trap moisture, and predispose to infection or inflammation.
-
Chronic middle-ear disease or Eustachian tube dysfunction which leads to poor ventilation, fluid accumulation, negative pressure, or repeated infections.
-
Preexisting skin conditions (eczema, psoriasis) in the ear canal which alter the protective barrier and predispose to infection or debris build-up.
-
Prior ear surgeries or perforated tympanic membrane which alter anatomy and make the ear canal / middle ear vulnerable.
-
Immunocompromised state (diabetes, HIV, corticosteroid use) which reduces ability to clear infections or heal.
-
Environmental and lifestyle factors: warm/humid climate, frequent swimming, use of prophylactic ear drops that alter normal flora, use of hearing aids or ear plugs for long periods.
Risk Factors
-
Swimming or water sports participation (especially in tropical/warm climates).
-
Frequent travel, diving or humidity exposure.
-
Use of ear-phones or ear-buds for long hours, pushing wax deeper.
-
History of chronic otitis media, repeated ear infections.
-
Diabetes mellitus, immunodeficiency, uncontrolled chronic disease.
-
Use of topical ear drops (especially antibiotics or steroids) without proper diagnosis - may predispose to secondary fungal or bacterial overgrowth.
-
Advanced age or very young age (with less robust ear canal skin defense).
-
Occupational exposure to dust, chemicals, or repeated misuse of ear canal.
Understanding these causes and risk factors helps clinicians identify which patients may benefit from early evaluation, and helps individuals take preventive measures to reduce the risk of requiring otoclisis.
Symptoms and Signs of Otoclisis
When the ear canal, middle ear or adjacent structures become compromised, a range of symptoms and physical signs may develop. In the context of otoclisis (or the underlying condition treated by it) the following may be experienced:
Symptoms
-
Itching (pruritus) in the ear canal; a common early sign.
-
Sensation of fullness or “blocked ear” - as though fluid or pressure is present.
-
Mild to moderate pain (otalgia) or discomfort in the ear.
-
Hearing reduction (conductive hearing loss) because blockage, fluid, debris or fungal/bacterial mass interfere with sound conduction.
-
Discharge (otorrhoea) from the ear - may be clear, yellow, green, brown, or even black if fungal debris are present.
-
Tinnitus (ringing or buzzing in the ear) or noise sensitivity.
-
Flaky skin inside the ear canal, crusts, or debris build-up visible.
-
In more advanced cases: dizziness/vertigo (if middle ear or inner ear involvement), persistent pain, swelling behind the ear, or fever (if infection).
Signs on Physical Examination
-
On otoscopic inspection: debris, fungal hyphae, crusts, or wax impacted inside the ear canal.
-
Redness, swelling (edema) of the ear canal skin.
-
Presence of fluid behind the tympanic membrane or a perforation in the eardrum.
-
Reduced mobility of the tympanic membrane (on pneumatic otoscopy) if middle ear fluid is present.
-
Abnormal hearing tests: pure tone audiometry showing conductive type hearing loss; tympanometry may show negative pressure or fluid.
-
In fungal cases: visible black, white or gray fungal colonies in ear canal.
When such symptoms persist beyond a short time, worsen, or are associated with recurrent issues, the patient may require diagnostic evaluation and possibly an intervention such as otoclisis (ear canal cleaning/irrigation) to manage the condition effectively.
Diagnosis of Otoclisis
Diagnosis of the condition requiring otoclisis (and the appropriateness of the otoclisis treatment) is a multi-step process involving history, physical exam, and sometimes adjunct tests.
Patient History
The clinician will ask about: onset and duration of symptoms (itching, fullness, hearing loss, discharge); exposure to water/swimming; use of ear devices or drops; prior ear infections or surgeries; underlying medical conditions (diabetes, immunosuppression); hearing symptoms; any vertigo or tinnitus; prior treatments attempted and responses.
Physical Examination
-
Otoscopy: careful inspection of the ear canal and tympanic membrane. Look for debris, foreign bodies, wax impaction, fungal elements, signs of inflammation, perforation.
-
Assessment of canal skin integrity, signs of swelling or chronic change.
-
Tympanic membrane mobility test (pneumatic otoscopy) to assess middle-ear fluid.
-
Hearing screening (whisper test, tuning fork tests for air-versus-bone conduction) as a basic check.
Adjunctive Diagnostic Tests
-
Audiometry: to quantify the hearing loss and determine type (conductive vs sensorineural).
-
Tympanometry: to check middle ear pressure and mobility of tympanic membrane.
-
Swab/culture: in recurrent or unusual cases, a sample of discharge or debris may be sent for fungal/bacterial culture to identify the pathogen.
-
Imaging: Very rarely, CT scan of mastoid/temporal bone may be needed if complicated middle-ear disease, mastoiditis or anatomical abnormalities are suspected.
-
If the ear canal is blocked with wax or debris, part of the diagnosis may simply involve removing the blockage and reassessing.
Determining the Need for Otoclisis
Once the diagnosis is clear, the clinician decides whether an ear canal cleaning/irrigation (otoclisis) or other procedure is indicated. Key factors guiding this decision: persistence of debris/impaction, ear-canal narrowing, recurrent infections, presence of fungal mass, poor response to conservative treatments, or high-risk underlying condition. Proper diagnosis ensures the right intervention is chosen and avoids unnecessary risks.
Treatment Options for Otoclisis
Treatment of the condition addressed by otoclisis (ear-canal/middle-ear debris, infection, obstruction) involves a tiered approach - from conservative measures to procedural interventions. These include the otoclisis itself, as well as adjunctive treatments.
Conservative (Non-procedural) Treatments
-
Dry-ear care: avoiding water in the ear canal, using ear-plugs during swimming, gently drying ears after exposure to moisture.
-
Ear-wax management: avoiding over-cleaning with cotton-buds; using cerumenolytic drops if wax accumulation is an issue.
-
Topical medications: in cases of infection (bacterial or fungal) - antifungal drops (eg clotrimazole) or antibacterial ear drops (when indicated) combined with ear canal cleaning. Studies show fungal infections (otomycosis) often respond to topical antifungals.
-
Addressing underlying risk factors: e.g., good glycemic control in diabetes, treating eczema/skin conditions, avoiding irritating ear devices, reducing exposure to high-humidity/water.
The Otoclisis Procedure (Ear-Canal Irrigation / Cleaning)
When debris, wax impaction, fungal masses, or chronic ear-canal blockage persists, otoclisis (also sometimes called ear-canal irrigation/clearing) may be indicated. The procedure typically comprises:
-
Visual evaluation of the ear canal under magnification/otoscope.
-
Removal of visible debris, wax, fungal elements using suction, micro-instruments, or gentle irrigation with saline or warm water-based solution.
-
In some cases, the canal is dried and then treated with otic drops (antifungal/antibacterial) to prevent recurrence.
-
Sometimes the canal may be mechanically widened or shaped if narrowing exists, or a temporary dressing may be placed to keep the canal dry and clean for some time.
The benefit of otoclisis is more complete clearance of blockage, improved penetration of topical medication, better ventilation and drainage in the ear canal, and reduced recurrence of disease. The decision for otoclisis is made by an ENT specialist (otolaryngologist), especially when recurrent cases, anatomical issues or risk-factors exist.
Surgical / Advanced Treatments
If underlying anatomical abnormalities, chronic middle-ear disease, perforated tympanic membrane, cholesteatoma, or mastoid involvement exists, further interventions may be required. These may involve tympanoplasty (repair of eardrum), mastoidectomy, canaloplasty (widening of the ear canal), or insertion of ventilation tubes. While these go beyond basic otoclisis, they may be required in complex or refractory cases.
Post-Procedure Care
Following otoclisis, the patient must maintain ear-care: keeping ears dry, avoiding inserting objects, using prescribed drops, follow-up visits for canal inspection, monitoring hearing changes, and ensuring any underlying conditions are managed. Patient education is key to avoiding recurrence.
Prevention and Management of Otoclisis
Prevention is vital in reducing the need for otoclisis or recurrence of ear-canal disorders. Effective strategies include:
Preventive Measures
-
Avoiding prolonged water exposure in the ear canal: use of ear-plugs when swimming, careful drying of ears after showers or swimming.
-
Maintain a small natural amount of ear-wax (cerumen) as it protects the canal; avoid over-cleaning or inserting cotton-buds.
-
Treating skin conditions promptly: eczema, psoriasis, dermatitis around the ear canal invite fungal/bacterial colonization.
-
Regular ear checks if you use hearing aids, ear-plugs, or devices that sit in the ear canal for long durations.
-
Managing chronic conditions: diabetes, immunosuppression, allergies, and ensuring they are well-controlled.
-
Avoiding use of topical ear drops (especially antibiotics or steroids) without medical supervision, as these may disrupt normal flora and predispose to fungal infections (otomycosis) which then may require more complex care.
-
Maintaining proper ear ventilation: ensuring Eustachian tube function is optimal, treating allergies or nasal congestion that impair ear ventilation.
Management Strategies for Ongoing or Recurrent Cases
-
Schedule periodic check-ups with an ENT specialist if you have a history of ear-canal blockage, frequent infections, or anatomical predisposition.
-
Develop a personal ear-care routine: gently drying ears after water exposure, avoiding insertion of foreign objects, using low-heat hair-dryer if indicated, avoiding scratches inside ear canal.
-
Use of prophylactic topical acidified ear-drops after swimming in high-risk environments (warm/humid water) to maintain dryness and acidic environment inhibiting fungal growth.
-
Awareness of early signs: itching, fullness, hearing changes - prompt inspection prevents progression.
-
If wax buildup is a recurring issue, consult ENT for professionally-managed wax removal rather than attempting self-removal.
Complications of Otoclisis
While otoclisis is typically a safe and beneficial procedure, and conditions prompting it often respond well, potential complications exist - both from the underlying ear condition and from the procedure itself.
Complications from the Underlying Condition
-
Untreated ear-canal blockage/infection may progress to more serious middle-ear involvement, tympanic membrane perforation, mastoiditis, or chronic otitis media. Fungal infections especially may recur or become chronic.
-
Hearing loss: Persistent conductive hearing loss may occur and in some cases lead to permanent damage if mid-/inner-ear structures are involved.
-
Spread of infection: In immunocompromised individuals, superficial fungal or bacterial ear infections may progress to invasive disease.
Complications from the Procedure (Otoclisis)
-
Canal trauma: inadvertent injury to canal skin or tympanic membrane during clearance.
-
Infection: although the aim is to treat infection, any instrumentation carries a small risk of introducing infection or exacerbating existing one.
-
Dizziness or vertigo: if very cold or forceful irrigation is used, inner-ear irritation may occur.
-
Bleeding or pain: transient discomfort or minor bleeding from canal skin is possible.
-
Recurrence: despite treatment, unless risk-factors are managed, recurrence remains possible - requiring repeated interventions.
To minimize risk, otoclisis should be performed by trained personnel (ENT specialist or audiologist under guidance), with appropriate technique, sterile equipment, and proper follow-up care.
Living with the Condition of Otoclisis
Living with a condition that requires ear-canal clearance/otoclisis or having undergone the procedure involves ongoing care, lifestyle adjustments and vigilant follow-up to maintain ear health and prevent recurrence.
Daily Living & Self-Care
-
After undergoing ear-canal cleaning, protect your ears from water ingress - use ear-plugs when swimming/showering, tilt the head to allow drainage, gently dry the ear with a hair dryer on low setting.
-
Avoid inserting cotton-buds or objects into the ear canal. Instead, clean the outer ear gently with a soft cloth.
-
If you use hearing aids or ear-phones, maintain hygiene; remove ear-devices periodically to allow canal ventilation, clean the tips and avoid prolonged continuous use.
-
Maintain good control of systemic conditions such as diabetes, skin disorders, allergies. These influence ear-canal health and recurrence risk.
-
Monitor your hearing. If you notice persistent fullness, hearing loss, tinnitus or worsening symptoms, consult your ENT promptly.
-
Use prophylactic care if your risk remains high: regular check-ups, preventative drops, and avoid exposure to humid/warm water when possible.
Emotional & Practical Considerations
-
Recurring ear issues can be frustrating. Maintain communication with your ENT specialist about best practices, signs of relapse, and when intervention is needed.
-
For children or older adults especially, ensure ear care routines are clearly understood by caretakers.
-
Hearing changes may impact communication - consider audiology consultation and hearing aid evaluation if needed.
-
Recognise the importance of preventive behavior: ear health isn't a “one-time” fix - maintaining the benefits of otoclisis requires ongoing attention.
Long-Term Outlook
With proper diagnosis, treatment, and preventive measures, most individuals who require otoclisis or similar ear-canal treatments achieve good outcomes: relief from symptoms, restoration of hearing/conduction, reduced recurrence of debris/infection, and improved quality of life. Recurrence remains a possibility, especially if underlying risk-factors persist, thus establishing a long-term ear-care plan is essential.
Top 10 Frequently Asked Questions about Otoclisis
1. What is Otoclisis?
Otoclisis is a specialized ear procedure that involves delivering medication directly into the middle ear or inner ear space to treat chronic or recurrent ear problems. The procedure is particularly useful in managing chronic otitis media, resistant infections, or inner ear inflammation. Unlike systemic medication, otoclisis ensures that a high concentration of the drug reaches the site of infection or inflammation, maximizing effectiveness while minimizing side effects elsewhere in the body.
In some cases, otoclisis can be performed using a tiny catheter, cannula, or via a myringotomy (small incision in the eardrum) to allow medication to enter the middle ear. It is often used in conjunction with other ENT treatments for comprehensive management.
2. Why is Otoclisis performed?
Otoclisis is typically recommended when conventional treatments, such as oral antibiotics, antifungals, or steroid therapy, fail to treat ear infections effectively. Specific reasons for performing otoclisis include:
-
Persistent or chronic ear infections: Patients with repeated middle ear infections that do not respond to oral or systemic antibiotics.
-
Resistant infections: Infections caused by bacteria or fungi resistant to standard therapy.
-
Structural or anatomical problems: Eustachian tube dysfunction, perforated eardrum, or middle ear fluid buildup.
-
Inflammation-related hearing loss: Conditions like labyrinthitis, vestibular disorders, or chronic inflammation affecting the inner ear.
-
Prevention of complications: Untreated infections can lead to mastoiditis, cholesteatoma, or long-term hearing damage.
By delivering medication directly to the affected area, otoclisis can accelerate healing, prevent recurrence, and improve hearing and comfort.
3. Who is a candidate for Otoclisis?
Candidates for otoclisis generally include:
-
Children and adults with recurrent or chronic ear infections that do not respond to oral medications.
-
Patients with resistant pathogens who require targeted therapy.
-
Individuals with anatomical issues that interfere with ear drainage, such as narrow eustachian tubes.
-
Patients unable to tolerate systemic antibiotics due to allergies or gastrointestinal issues.
-
Those needing localized treatment for inner ear inflammation or hearing problems.
A complete ENT evaluation is essential before the procedure. This may include:
-
Ear examination (otoscopy)
-
Hearing tests (audiometry)
-
Imaging studies (CT or MRI of the ear, if necessary)
-
Laboratory tests to identify the type of pathogen causing infection
4. How is Otoclisis performed?
Otoclisis is a minimally invasive procedure. Here's a step-by-step explanation:
-
Anesthesia: Local anesthesia is applied to numb the ear canal and eardrum. Children or anxious patients may receive sedation.
-
Accessing the middle ear: A tiny puncture in the eardrum (myringotomy) may be made if necessary.
-
Medication delivery: Using a catheter or cannula, the prescribed medication (antibiotic, antifungal, or steroid) is delivered directly into the middle ear space.
-
Post-procedure support: In some cases, absorbable packing is placed to maintain medication contact and protect the ear.
The procedure typically takes 15-30 minutes and is usually outpatient, meaning the patient can go home the same day.
5. What types of medications are used in Otoclisis?
The choice of medication depends on the condition being treated:
-
Antibiotics: For bacterial infections, e.g., otitis media or chronic ear infections.
-
Antifungal agents: For fungal infections in the middle ear.
-
Corticosteroids: To reduce inflammation and swelling of middle or inner ear tissues.
-
Combination therapies: Sometimes antibiotics and steroids are combined for maximum effect.
Delivering these medications directly into the middle ear ensures higher local concentration compared to oral therapy, increasing effectiveness while reducing systemic side effects.
6. What are the benefits of Otoclisis?
Otoclisis offers numerous advantages, including:
-
Targeted therapy: Directly treats the infection or inflammation at its source.
-
Faster recovery: Resolves chronic ear infections more quickly than systemic therapy.
-
Minimally invasive: No large incisions, minimal disruption of ear structures.
-
Reduced systemic side effects: Less impact on other organs, avoiding antibiotic-related complications.
-
Improved hearing: Restores middle ear function, reduces fluid, and improves sound conduction.
-
Preventive benefit: Reduces recurrence and prevents long-term complications, like cholesteatoma or permanent hearing loss.
7. Is Otoclisis painful?
The procedure is generally pain-free due to local anesthesia or sedation. After the procedure, patients may experience:
-
Mild pressure or fullness in the ear
-
Temporary discomfort or irritation
-
Slight fluid drainage from the ear
Pain is usually mild and can be managed with over-the-counter painkillers. Most patients resume normal activities immediately after the procedure.
8. What are the risks and complications?
Otoclisis is considered safe, but potential risks include:
-
Ear discomfort or fullness for a few days
-
Minor bleeding at the puncture site (if myringotomy is performed)
-
Dizziness or vertigo temporarily after the procedure
-
Allergic reaction to medications used
-
Secondary infection (rare if sterile technique is followed)
-
Temporary hearing fluctuations
Most complications are rare and typically mild when the procedure is performed by an experienced ENT surgeon.
9. What is the recovery process after Otoclisis?
Recovery is usually fast and straightforward:
-
Post-procedure: Most patients go home the same day.
-
Activity restrictions: Avoid water in the treated ear for several days.
-
Ear care: Mild ear drainage or fullness may occur and resolve in a few days.
-
Follow-up: ENT visits ensure infection resolution and determine if repeat treatment is needed.
-
Hearing improvement: Patients often notice better hearing within days to weeks, depending on the severity of the infection and underlying ear condition.
10. How much does Otoclisis cost, and is it covered by insurance?
The cost varies depending on:
-
Hospital or clinic fees
-
Surgeon's expertise
-
Type and volume of medication used
-
Number of treatment sessions required
Otoclisis is generally considered medically necessary for chronic or recurrent ear infections and is often covered by insurance. Cosmetic or elective procedures may not be covered. Patients should confirm insurance coverage, co-pays, and out-of-pocket costs with both their hospital and insurance provider.


