Introduction to Parathyroidectomy
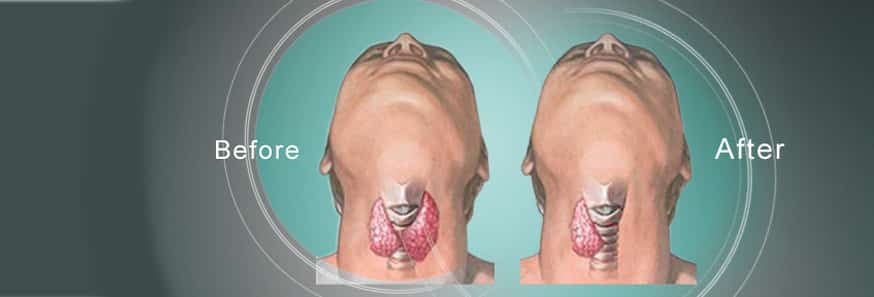
Parathyroidectomy is a specialized surgical procedure designed to remove one or more parathyroid glands, which are tiny endocrine organs located behind the thyroid gland in the neck. Despite their small size, these glands play a critical role in maintaining calcium and phosphorus balance in the body by producing parathyroid hormone (PTH). When the parathyroid glands become abnormal, due to conditions such as benign adenomas, hyperplasia (enlargement of multiple glands), or, in rare instances, parathyroid carcinoma, they can secrete excess PTH. This overproduction of PTH leads to hypercalcemia, a condition characterized by elevated calcium levels in the blood. Hypercalcemia can affect multiple organ systems, causing fatigue, muscle weakness, bone resorption, kidney stones, neurocognitive disturbances, cardiovascular issues, and gastrointestinal symptoms.
Parathyroidectomy is considered the definitive treatment for hyperparathyroidism. The procedure not only restores normal PTH and calcium levels but also prevents further systemic damage and improves the patient's overall quality of life. Modern surgical techniques have evolved to include minimally invasive parathyroidectomy (MIP), which reduces incision size, shortens recovery time, and minimizes scarring. Intraoperative PTH monitoring further increases the precision of surgery by confirming successful removal of abnormal glands in real time. The benefits of parathyroidectomy extend beyond symptom relief: it prevents long-term complications such as osteoporosis, kidney damage, neuromuscular dysfunction, and cognitive impairment. For patients with hyperparathyroidism, timely surgical intervention can transform health outcomes, restoring energy, bone strength, kidney function, and overall metabolic balance.
Causes and Risk Factors of Parathyroidectomy
Parathyroidectomy is most commonly indicated in patients with primary hyperparathyroidism, a condition in which one or more parathyroid glands autonomously secrete excess PTH. The most frequent cause is a single benign adenoma, responsible for approximately 80-85% of cases. Less frequently, multiple gland hyperplasia occurs, and very rarely, parathyroid carcinoma can be the underlying cause. These conditions lead to chronic hypercalcemia, which affects bone, kidney, heart, and neuromuscular function over time.
Secondary hyperparathyroidism is another cause, usually occurring in patients with chronic kidney disease or vitamin D deficiency. In these cases, the parathyroid glands enlarge and increase PTH secretion as a compensatory response to low calcium levels. When medical therapy is insufficient, surgical removal of part or all of the parathyroid glands becomes necessary. Tertiary hyperparathyroidism develops when glands become autonomously hyperactive after prolonged secondary hyperparathyroidism, often in post-renal transplant patients.
Risk factors for requiring parathyroidectomy include:
-
Age: Hyperparathyroidism is more common in adults over 50, with increased prevalence in postmenopausal women.
-
Gender: Women are disproportionately affected, particularly after menopause, due to hormonal changes affecting bone and calcium metabolism.
-
Genetic conditions: Familial syndromes, such as Multiple Endocrine Neoplasia types 1 and 2A, increase the likelihood of multi-gland disease.
-
Previous neck radiation: Patients exposed to radiation in the head or neck region are at higher risk.
-
Chronic kidney disease: Secondary hyperparathyroidism can progress to tertiary disease.
-
Vitamin D deficiency: Prolonged deficiency can exacerbate PTH overproduction.
-
Medications: Lithium therapy and certain diuretics may impact calcium metabolism.
Understanding these causes and risk factors allows clinicians to identify high-risk patients and intervene before severe complications develop.
Symptoms and Signs Indicating Parathyroidectomy
Parathyroid disorders affect multiple organ systems, and the clinical presentation can vary widely. Symptoms include:
-
Musculoskeletal: Persistent bone and joint pain, muscle weakness, and fragility fractures due to chronic bone resorption.
-
Renal: Kidney stones, nephrocalcinosis, frequent urination, and excessive thirst caused by hypercalcemia-induced polyuria.
-
Gastrointestinal: Nausea, constipation, abdominal pain, poor appetite, and sometimes pancreatitis.
-
Neurological/Cognitive: Fatigue, “brain fog,” mood disturbances, depression, anxiety, and decreased concentration.
-
Cardiovascular: Arrhythmias, hypertension, and increased risk of cardiovascular disease due to chronic hypercalcemia.
Clinical signs observed during evaluation include elevated serum calcium, elevated or inappropriately normal PTH, reduced bone mineral density on DEXA scans, imaging evidence of kidney stones, and rarely, palpable neck masses if a parathyroid carcinoma is present. Hypercalcemia may be asymptomatic in early stages, making laboratory evaluation critical. Persistent or severe symptoms, combined with biochemical abnormalities, often justify surgical intervention.
Diagnosis and Preoperative Evaluation
Diagnosis involves a combination of laboratory tests, imaging, and clinical evaluation:
Laboratory tests:
-
Total and ionized serum calcium
-
Parathyroid hormone (PTH) levels
-
Phosphorus and vitamin D status
-
Renal function (creatinine, GFR)
-
24-hour urinary calcium excretion
Imaging for localization:
-
Neck ultrasonography to identify enlarged glands
-
Technetium-99m sestamibi scan for functional localization
-
4D CT or MRI in complex or reoperative cases
Additional assessments:
-
Bone mineral density to assess osteoporosis or osteopenia
-
Kidney imaging to evaluate for stones or nephrocalcinosis
-
Cardiovascular and anesthetic evaluation to ensure surgical safety
Preoperative planning ensures precise localization, identification of abnormal glands, and selection of the most appropriate surgical approach, minimizing risk and optimizing outcomes.
Treatment Options for Parathyroidectomy
Surgical intervention is the primary treatment. Options include:
-
Minimally invasive parathyroidectomy (MIP): Targeted removal of a single abnormal gland using a small incision. Offers faster recovery, less pain, and minimal scarring.
-
Bilateral neck exploration: Recommended for multiple gland disease, inconclusive imaging, or familial syndromes.
-
Subtotal parathyroidectomy: Removal of 3-3.5 glands, often used in secondary or tertiary hyperparathyroidism.
-
Total parathyroidectomy with autotransplantation: Grafting small parathyroid tissue into another site (forearm) to preserve some function in severe multi-gland disease.
Postoperative care involves monitoring calcium and PTH levels, supplementation with calcium and vitamin D if necessary, and long-term follow-up to ensure stability of bone, kidney, and metabolic health.
Prevention and Management of Parathyroidectomy
While primary hyperparathyroidism cannot always be prevented, certain strategies reduce disease progression:
-
Maintain adequate vitamin D levels and correct deficiency early
-
Monitor calcium and PTH in high-risk populations
-
Address chronic kidney disease and mineral imbalances promptly
-
Optimize bone health with weight-bearing exercise and diet
-
Hydrate adequately to prevent kidney stones
Pre- and post-surgery management ensures the patient is medically optimized, complications are minimized, and long-term metabolic balance is maintained. Patient education about symptom recognition and lifestyle adherence is crucial.
Complications of Parathyroidectomy
Potential complications include:
-
Early: Bleeding/hematoma, wound infection, recurrent laryngeal nerve injury (voice changes), and transient hypocalcemia
-
Specific: Hungry bone syndrome, where bones rapidly absorb calcium postoperatively, requiring intensive supplementation
-
Long-term: Persistent or recurrent hyperparathyroidism, permanent hypoparathyroidism, residual bone or kidney damage
Surgeon experience, precise localization, and intraoperative PTH monitoring are critical to minimizing risks.
Living with Life After Parathyroidectomy
Recovery is generally rapid. Patients may experience normalization of calcium and PTH levels, relief from fatigue, bone pain, and kidney complications, and improvement in overall quality of life. Long-term follow-up includes:
-
Monitoring calcium, PTH, and kidney function
-
Periodic bone density testing
-
Hydration and dietary guidance to prevent stones
-
Weight-bearing exercises for bone health
-
Education about hypo- and hypercalcemia symptoms
Most patients regain normal activity and enjoy improved health, though pre-existing bone or kidney damage may require ongoing management.
Top 10 Frequently Asked Questions about Parathyroidectomy
1. What is a parathyroidectomy?
A parathyroidectomy is a surgical procedure to remove one or more parathyroid glands that are overactive or enlarged. These tiny glands, located behind the thyroid, regulate calcium levels in the body. The surgery is performed to treat hyperparathyroidism and restore normal calcium balance, preventing complications such as kidney stones, osteoporosis, and fatigue.
2. Why is parathyroidectomy performed?
Parathyroidectomy is typically recommended for patients with:
-
Primary hyperparathyroidism: Overactive glands often due to adenomas
-
Secondary hyperparathyroidism: Caused by chronic kidney disease
-
Tertiary hyperparathyroidism: Persistent hyperparathyroidism after kidney transplant
-
Symptoms of high calcium, including fatigue, depression, bone pain, kidney stones, and gastrointestinal issues
-
Risk of long-term complications like osteoporosis or fractures
Surgery is the most effective way to normalize calcium and parathyroid hormone (PTH) levels.
3. Who is a candidate for parathyroidectomy?
Candidates include:
-
Patients with symptomatic hyperparathyroidism
-
Individuals with asymptomatic hyperparathyroidism but with high calcium, kidney dysfunction, or low bone density
-
Patients whose parathyroid glands are enlarged, overactive, or producing excess PTH
-
Those in good overall health capable of undergoing surgery
Evaluation involves blood tests, imaging (ultrasound, Sestamibi scan, or CT scan), and bone density scans.
4. How is parathyroidectomy performed?
Parathyroidectomy is performed under general anesthesia. Approaches include:
-
Minimally invasive parathyroidectomy: Small neck incision guided by preoperative imaging and intraoperative PTH monitoring
-
Traditional bilateral exploration: Larger incision to explore all four glands, used for multiple gland disease or complex cases
The surgeon removes abnormal gland(s) while preserving healthy ones. Surgery usually takes 1-2 hours, and most patients can go home the same day or after one night in the hospital.
5. What are the benefits of parathyroidectomy?
-
Restores normal calcium levels
-
Reduces symptoms like fatigue, bone pain, depression, and kidney stones
-
Prevents long-term complications, including osteoporosis, fractures, and kidney disease
-
High success rate: Over 95% for primary hyperparathyroidism
-
Improved quality of life with increased energy and better overall health
Patients often notice symptom improvement soon after surgery.
6. Is parathyroidectomy painful?
During surgery, patients are under general anesthesia, so there is no pain during the procedure. Post-operative discomfort may include:
-
Mild neck pain or soreness at the incision site
-
Temporary difficulty swallowing
-
Mild swelling or stiffness
Pain is generally mild and managed with over-the-counter or prescribed pain medication, resolving within a few days.
7. What are the risks and complications?
While generally safe, parathyroidectomy carries potential risks:
-
Infection at the surgical site
-
Bleeding or hematoma formation
-
Injury to the recurrent laryngeal nerve, causing temporary or rare permanent hoarseness
-
Hypocalcemia (low calcium) if healthy glands are affected
-
Scar formation (usually small in minimally invasive surgery)
Experienced surgeons and proper post-operative monitoring reduce the risk of complications.
8. What is the recovery process after parathyroidectomy?
Recovery is usually quick:
-
Hospital stay: Outpatient or one night in hospital for observation
-
Activity restrictions: Avoid strenuous activity for 1-2 weeks
-
Calcium monitoring: Blood tests to monitor calcium and PTH levels
-
Follow-up: Regular check-ups to ensure calcium levels normalize
-
Symptom improvement: Fatigue and other symptoms improve within days to weeks
Most patients return to normal activities within a week.
9. How long does it take for calcium levels to normalize?
-
Calcium levels often begin to normalize within 24-48 hours after surgery.
-
Temporary calcium or vitamin D supplementation may be needed for a few weeks.
-
Full stabilization of calcium and PTH may take several weeks, monitored through regular blood tests.
10. How much does parathyroidectomy cost, and is it covered by insurance?
The cost depends on:
-
Hospital and surgeon fees
-
Anesthesia and operating room charges
-
Post-operative care, labs, and follow-up visits
Parathyroidectomy is medically necessary for hyperparathyroidism, and most health insurance plans cover the procedure, including surgery, hospital stay, and follow-up care. Patients should verify co-pays and out-of-pocket expenses with their insurance provider.


