Introduction to Parotid Gland Removal - Parotidectomy
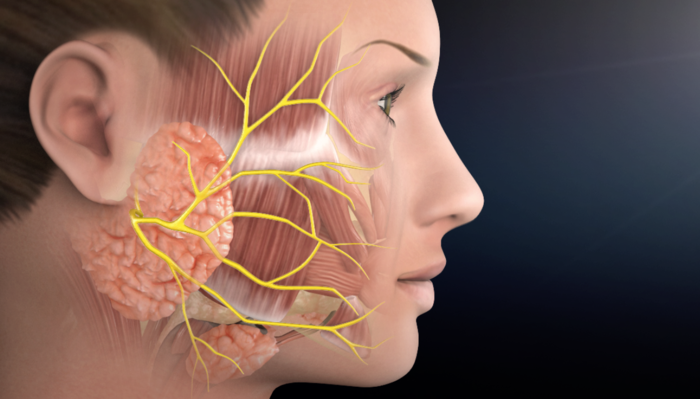
The parotid glands are the largest of the salivary glands and are located on either side of the face, just below and in front of the ears. These glands play a critical role in producing saliva, which aids digestion, lubricates the mouth, and protects the oral cavity from infections. The parotid glands also house the facial nerve, which controls facial expressions, making surgical intervention a delicate process.
Parotidectomy is a surgical procedure to remove part or all of the parotid gland. It is primarily performed when there is a growth, tumor, chronic infection, or obstruction that affects the gland's function or poses a risk of malignancy. Most tumors in the parotid gland are benign, but surgical removal is often recommended because even benign tumors can grow over time, cause facial asymmetry, or transform into malignant lesions. Advances in surgical techniques, such as nerve monitoring, microsurgery, and minimally invasive approaches, have improved patient outcomes, reduced complications, and enhanced recovery. Today, parotidectomy is considered a safe and effective solution for restoring health and preventing further complications.
Causes and Risks Leading to Parotid Gland Removal
Parotidectomy is recommended when the gland is affected by conditions that may compromise its function or pose a health risk.
Causes
-
Parotid Tumors: The most common reason for parotidectomy is the presence of tumors in the gland. Benign tumors such as pleomorphic adenoma and Warthin's tumor account for the majority of cases. Malignant tumors, although less common, include mucoepidermoid carcinoma, adenoid cystic carcinoma, acinic cell carcinoma, and metastatic lesions from skin cancers.
-
Chronic Parotitis: Long-term inflammation of the parotid gland can occur due to bacterial or viral infections, autoimmune conditions like Sjögren's syndrome, or duct obstructions. Persistent inflammation can lead to scarring, repeated infections, and functional impairment, necessitating surgical intervention.
-
Obstructive Conditions: Salivary stones, strictures, or narrowing of the salivary duct can block saliva flow, resulting in recurrent infections, swelling, and pain. Surgery may be required if conservative treatments fail.
-
Cysts and Non-Tumorous Lesions: Congenital cysts, lymphoepithelial cysts, or post-traumatic cysts may require removal if they interfere with normal function or cause cosmetic concerns.
Risk Factors
-
Age: Tumors are more common in adults aged 30-70 years.
-
Smoking: Increases the risk of certain tumors like Warthin's tumor.
-
Radiation Exposure: Past radiation therapy to the head and neck region can increase risk of malignant growths.
-
Autoimmune Disorders: Conditions such as Sjögren's syndrome may predispose individuals to chronic parotitis.
-
History of Skin Cancer: Malignant skin cancers like melanoma can metastasize to the parotid gland.
Symptoms and Signs Leading to Parotid Gland Removal
Symptoms vary depending on the underlying condition, but several key signs indicate the need for evaluation and possible surgery.
Common Symptoms
-
Swelling or Lump: A painless lump near the jaw or in front of the ear is often the first indication of a parotid tumor.
-
Facial Pain or Discomfort: May result from pressure due to the growth or inflammation of the gland.
-
Difficulty Chewing or Swallowing: Swelling or obstruction can interfere with normal oral function.
-
Dry Mouth: Reduced saliva production can occur due to chronic inflammation or gland dysfunction.
-
Recurrent Infections: Chronic parotitis or duct obstruction may cause repeated bouts of infection, swelling, or fever.
Red Flags Suggesting Malignancy
-
Facial Nerve Weakness or Paralysis: Tumors affecting the nerve may cause asymmetry or loss of movement in part of the face.
-
Rapidly enlarging mass or fixed lumps
-
Pain radiating toward the ear
-
Enlarged nearby lymph nodes
Prompt medical evaluation is critical if these signs appear.
Diagnosis of Parotid Gland Disorders
Accurate diagnosis is vital for selecting the appropriate treatment plan.
Clinical Evaluation
The diagnostic process begins with a detailed medical history, assessment of facial nerve function, physical examination, and inspection of the oral cavity and neck.
Imaging Studies
-
Ultrasound: Useful for detecting superficial masses and guiding biopsies.
-
CT Scan: Provides detailed information about tumor size, involvement of surrounding tissues, and any calcifications.
-
MRI: Best for evaluating deep-lobe tumors and differentiating benign from malignant lesions.
-
Sialography: Special imaging to assess duct obstruction and chronic parotitis.
Biopsy Techniques
-
Fine-Needle Aspiration Cytology (FNAC): Minimally invasive and effective for distinguishing benign from malignant lesions.
-
Core Needle Biopsy: Provides a larger tissue sample for more accurate histopathological evaluation when needed.
A combination of imaging and biopsy results guides surgical planning and helps predict postoperative outcomes.
Treatment Options for Parotid Gland Disorders
Treatment depends on the diagnosis, tumor type, size, and involvement of surrounding structures. Surgery is often the definitive treatment.
Surgical Procedures
-
Superficial Parotidectomy: Removes the outer lobe while preserving the facial nerve; commonly used for benign tumors.
-
Total Parotidectomy: Complete removal of the gland; indicated for malignant tumors or deep-lobe involvement.
-
Partial Parotidectomy: Limited removal of affected tissue, preserving as much healthy gland as possible.
-
Radical Parotidectomy: Involves removal of the gland along with the facial nerve in aggressive malignancies; often followed by nerve reconstruction.
Non-Surgical Treatments
-
Medications: Antibiotics for infections, anti-inflammatory drugs for pain, and steroids for autoimmune causes.
-
Sialendoscopy: Minimally invasive procedure to remove stones or widen ducts.
-
Radiation Therapy: Often used post-surgery for malignant tumors or when surgery is not feasible.
-
Chemotherapy: Reserved for advanced cancers, usually in combination with radiation.
Prevention and Management of Parotid Gland Disorders
While not all conditions can be prevented, patients can reduce risks and maintain parotid health.
-
Hydration: Drink plenty of water to maintain saliva flow.
-
Avoid Smoking: Reduces risk of certain tumors.
-
Oral Hygiene: Regular brushing, flossing, and dental checkups prevent infections.
-
Manage Autoimmune Diseases: Proper treatment can prevent chronic parotitis.
-
Sun Protection: Protecting the skin reduces the risk of metastasis to the parotid.
Before surgery, managing infections and maintaining nutrition can improve outcomes and reduce complications.
Complications of Parotidectomy
Despite modern techniques, complications may occur due to the gland's anatomy and proximity to the facial nerve.
Immediate Complications
-
Facial Nerve Weakness: Temporary weakness is common; permanent paralysis is rare.
-
Hematoma: Bleeding may occur and occasionally requires drainage.
-
Infection: Rare due to rich blood supply.
Long-Term Complications
-
Frey Syndrome: Sweating and flushing while eating due to nerve misdirection; treatable with Botox or surgery.
-
Salivary Fistula: Leakage of saliva under the skin, usually resolves conservatively.
-
Numbness: Particularly around the earlobe; often improves over time.
-
Cosmetic Concerns: Scarring or facial asymmetry; advanced techniques can minimize these effects.
Living with Parotidectomy
Most patients recover very well after parotidectomy and can return to normal life with few long-term effects.
A. Recovery Timeline
-
Hospital stay: 1-2 days
-
Return to daily activities: 1-2 weeks
-
Complete healing: Several weeks to a few months
-
Facial nerve recovery: Weeks to one year (if affected)
B. Lifestyle Adjustments
-
Maintain good hydration
-
Adopt a soft diet during initial healing
-
Protect incision from sunlight to avoid scarring
-
Attend physiotherapy for facial muscle strengthening
-
Avoid high-impact activities during recovery
C. Emotional and Psychological Support
Some patients may experience anxiety due to cosmetic changes or nerve weakness.
Counseling and support groups may be beneficial.
D. Long-Term Prognosis
-
Benign tumors: Excellent
outcomes with low recurrence if removed completely
-
Malignant tumors: Prognosis
depends on tumor type, stage, and treatment; early detection improves
survival
-
Quality of life: Generally
good, with minimal impact on chewing, speaking, or saliva production
Overall, most individuals lead normal lives, experiencing no significant
long-term disability.
Benign tumors: Excellent outcomes with low recurrence if removed completely
Malignant tumors: Prognosis depends on tumor type, stage, and treatment; early detection improves survival
Quality of life: Generally good, with minimal impact on chewing, speaking, or saliva production
Top 10 Frequently Asked Questions about Parotid Gland Removal - Parotidectomy
1. What is parotidectomy and when is it needed?
Parotidectomy is a surgical procedure to remove all or part of the parotid gland, which is the largest salivary gland located just in front of and below the ear. The surgery is typically needed when the gland develops abnormalities such as tumors (benign or malignant), chronic infections, obstructive stones, or cysts. The procedure aims to eliminate disease, relieve symptoms, and prevent recurrence while preserving the facial nerve, which controls expressions like smiling, blinking, and frowning.
This surgery is crucial because untreated tumors or chronic infections can lead to pain, swelling, recurrent infections, or, in malignant cases, the spread of cancer.
2. Why is parotid gland removal performed?
Parotid gland removal is performed for several medical reasons:
-
Benign tumors like pleomorphic adenomas or Warthin's tumor, which can grow and cause facial asymmetry or pressure.
-
Malignant tumors such as mucoepidermoid carcinoma, acinic cell carcinoma, or adenoid cystic carcinoma, which can invade surrounding tissues.
-
Chronic parotitis: Long-standing inflammation that is resistant to antibiotics and causes recurrent swelling or discomfort.
-
Obstructive salivary stones (sialolithiasis) that block saliva flow and cause pain or swelling during meals.
-
Cysts, abscesses, or infections that do not resolve with medical management.
Surgical removal not only resolves current symptoms but also prevents serious long-term complications, such as facial nerve damage, persistent infection, or malignant spread.
3. Who is a candidate for parotidectomy?
Candidates include:
-
Patients diagnosed with benign or malignant parotid tumors via imaging or biopsy.
-
Individuals suffering from chronic, recurrent infections unresponsive to medications.
-
Patients with salivary duct obstruction or stones causing pain, swelling, or saliva leakage.
-
Individuals with good overall health able to tolerate anesthesia and surgery.
-
Those needing preservation of facial movement for cosmetic and functional reasons.
A thorough preoperative evaluation includes physical examination, ultrasound or CT/MRI scans, and often fine-needle aspiration biopsy to identify the nature of the lesion.
4. How is parotid gland removal performed?
Parotidectomy is typically done under general anesthesia. The procedure can vary depending on the disease:
-
Superficial parotidectomy: Removes the outer portion of the gland, usually for benign tumors located in the superficial lobe.
-
Total parotidectomy: Removes the entire gland, often necessary for malignant tumors or diffuse disease.
-
Extracapsular dissection: A minimally invasive approach for small, well-defined tumors that preserves more healthy tissue.
During surgery, the facial nerve is carefully identified and protected, as it runs through the parotid gland. Surgeons also take care to create an incision that minimizes visible scarring while allowing full access to the diseased gland.
5. What are the benefits of parotidectomy?
The surgery offers multiple benefits:
-
Complete removal of tumors or stones, reducing the risk of recurrence.
-
Resolution of pain, swelling, and chronic infection, improving comfort and quality of life.
-
Prevention of malignant spread for cancerous tumors.
-
Preservation of facial nerve function, maintaining natural expressions and facial symmetry.
-
Long-term improvement in salivary gland function, reducing repeated infections and discomfort.
Patients often notice significant improvement in symptoms and daily comfort within weeks of surgery.
6. Is parotidectomy painful?
While patients are under general anesthesia during the procedure and feel no pain, mild discomfort is normal after surgery:
-
Soreness or tightness at the incision site.
-
Mild swelling or bruising around the ear and cheek.
-
Temporary numbness or tingling in areas surrounding the surgical site.
Pain is typically managed with prescription or over-the-counter pain medications and gradually subsides over 1-2 weeks.
7. What are the risks and complications of parotidectomy?
Although parotidectomy is generally safe, potential risks include:
-
Facial nerve injury, causing temporary or rarely permanent weakness or asymmetry.
-
Infection at the incision site.
-
Bleeding or hematoma formation, which may require drainage.
-
Salivary fistula, where saliva leaks through the incision.
-
Frey's syndrome, a rare condition where sweating occurs on the cheek while eating.
-
Scarring, which is usually minimal and often hidden along natural skin creases.
Experienced surgeons minimize these risks through meticulous surgical techniques and careful monitoring.
8. What is the recovery process after parotidectomy?
Recovery typically includes:
-
Hospital stay: 1-3 days depending on the complexity of surgery.
-
Activity restrictions: Avoid strenuous activity, heavy lifting, or twisting motions for 2-4 weeks.
-
Incision care: Keep the site clean and monitor for swelling, redness, or fluid accumulation.
-
Drain management: Temporary surgical drains may be placed to prevent fluid buildup.
-
Follow-up appointments: Regular visits to assess healing, facial nerve function, and ensure tumor removal was complete.
Most patients return to normal daily activities within 2-3 weeks, with full recovery and optimal cosmetic results over several months.
9. How long does it take to regain facial movement and appearance?
-
Mild swelling and bruising typically resolve within 1-2 weeks.
-
Temporary facial weakness may take weeks to months to fully recover if the facial nerve is affected.
-
Scars gradually fade over several months, often becoming nearly invisible.
-
Long-term results include restored facial symmetry, resolution of symptoms, and improved quality of life.
10. How much does parotidectomy cost, and is it covered by insurance?
The cost of parotidectomy depends on:
-
Hospital and surgeon fees.
-
Anesthesia and operating room charges.
-
Post-operative care, imaging, and follow-up visits.
Parotidectomy is usually medically necessary for tumors, stones, or chronic infections, and is covered by most health insurance plans, including surgery, hospitalization, and post-operative care. Cosmetic-only procedures may not be fully covered. Patients should confirm coverage, co-pays, and out-of-pocket expenses with their insurance provider before surgery.


