Introduction to Parotid Gland Removal
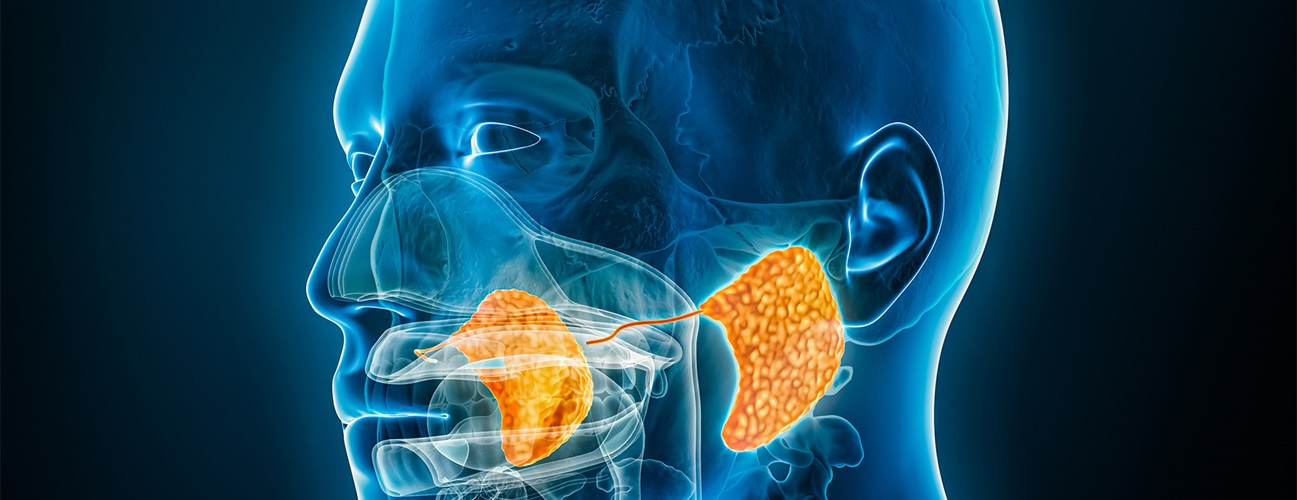
Parotid gland removal, medically known as parotidectomy, is a surgical procedure performed to remove all or part of the parotid gland - the largest of the salivary glands located on each side of the face, just in front of the ears. The parotid gland plays a crucial role in producing saliva, which aids digestion, lubricates the mouth, protects teeth, and maintains overall oral health. The parotid gland is uniquely positioned around the facial nerve, the nerve responsible for facial expressions, making any surgical procedure in this region highly delicate and specialised.
Parotidectomy is performed for a range of conditions, most commonly parotid tumours. While the majority of these tumours are benign, they often continue to grow and can cause complications if left untreated. Malignant tumours require timely and complete removal as the primary treatment approach. Other conditions such as chronic infections, salivary duct blockages, autoimmune disorders, or trauma may also lead to the need for surgery.
The procedure may involve removing only the superficial lobe of the gland (superficial parotidectomy), both lobes of the gland (total parotidectomy), or, in more advanced disease, surrounding tissues including branches of the facial nerve (radical parotidectomy). Given its complexity, parotid gland removal is typically carried out by experienced head and neck surgeons or maxillofacial surgeons with expertise in facial nerve preservation.
Understanding the purpose, process and expected outcomes of the surgery helps patients prepare mentally and physically. This guide covers the causes, symptoms, diagnosis, treatment options, recovery, potential complications and long-term lifestyle considerations associated with parotid gland removal.
Causes and Risk of Parotid Gland Removal
The primary causes for parotid gland removal (parotidectomy) include tumors (both benign and malignant), chronic infection, and blockage due to stones. Risk factors involve tumor characteristics, chronic inflammatory or infectious conditions, and, less commonly, congenital or systemic diseases.
Underlying conditions that lead to removal
-
Most common reason: Tumours (neoplasms) of the parotid gland - benign (e.g., pleomorphic adenoma, Warthin tumour) or malignant (e.g., mucoepidermoid carcinoma, adenoid cystic carcinoma)
-
Other causes: chronic infections of the parotid (chronic parotitis), salivary duct stones (sialolithiasis) blocking the gland, congenital malformations, or rare inflammatory processes.
-
Less commonly, metastases from cancers elsewhere can involve the parotid and require removal.
Risk factors
-
Tumour risk: although rare, about 75-80% of primary parotid tumours are benign; ~20% malignant in many series.
-
Factors increasing risk of gland disease or tumours: radiation exposure to head & neck, previous gland disease, smoking (especially with Warthin tumour), or certain viral infections. (You may need to check latest data for India/Asia)
-
Surgical risk factors: tumour size, location (deep lobe vs superficial), proximity/involvement of facial nerve, prior surgery or radiation to the area → all increase complexity.
Why removal may be the recommended treatment
-
For benign tumours: to prevent growth, compression of nearby structures, aesthetic issues, risk (albeit low) of malignant transformation.
-
For malignant tumours: removal is often primary management to achieve cure or control of disease.
-
For obstructive causes: e.g., stones causing repeated infection, damage to gland function, may lead to consideration of removal.
You can emphasise that the decision for removal is usually made after careful evaluation and the surgical plan is tailored according to the lesion, patient's general condition and goals.
Symptoms and Signs of Parotid Gland Removal
After parotid gland removal (parotidectomy), patients commonly experience a mix of expected post-surgical symptoms and potential complications. Recognizing these signs helps manage recovery and identify when further medical attention is needed.
What the patient may notice before surgery
-
A lump or swelling in front of the ear or in the cheek area (parotid region) is often the first sign. This is common with tumours.
-
Pain or discomfort: some tumours may be painless; others may cause dull ache, especially with inflammation or rapid growth.
-
Facial nerve symptoms: weakness of facial muscles (e.g., inability to smile, raise eyebrow, drooping) may be a sign of nerve involvement by tumour.
-
Changes in saliva or swallowing: if the gland is obstructed or inflamed, one may notice dry mouth, difficulty swallowing, swelling after eating etc.
-
Recurrent infections: episodes of parotitis (swelling of gland) or sialadenitis may occur.
Signs the surgeon will look for
-
On examination: firm or mobile mass in parotid region; signs of fixation to surrounding tissues (which may indicate malignancy)
-
Facial nerve assessment: testing each branch to ensure muscles of expression are intact.
-
Lymph node enlargement in neck if malignant disease suspected.
-
Imaging findings: though that is technical (will cover in diagnosis).
Diagnosis of Parotid Gland Removal
Diagnosis leading to parotid gland removal (parotidectomy) relies on a careful combination of clinical evaluation, imaging, and tissue sampling to distinguish benign from malignant tumors, localize lesions, and guide the surgical approach.
Step-by-step diagnostic work-up
-
History and physical examination: assess symptoms, duration, growth rate of lump, presence of pain or facial nerve involvement, risk factors.
-
Imaging studies
-
Ultrasound: often the first choice for a superficial lump.
-
CT scan or MRI: for deeper lesions, assessing relation to facial nerve, bone involvement, deep lobe extension.
-
In certain cases, PET/CT if metastasis is suspected.
-
-
Tissue sampling (biopsy, cytology)
-
Fine-needle aspiration (FNA) to sample the lump to determine benign vs malignant.
-
Sometimes core biopsy if needed, though care must be taken because the tumour may seed.
-
-
Pre-operative planning
-
Mapping of facial nerve, anatomical relationships; nerve monitoring may be considered.
-
-
Other pre-surgery investigations
-
Routine blood work, general anaesthesia assessment, possibly dental/oral health check since the gland sits near oral cavity.
-
Making the decision for removal
-
Based on benign vs malignant status, size and location of lesion, involvement of nerve or adjacent structures, patient's general health.
-
The surgeon and multidisciplinary team will plan the type of removal: superficial, total, radical, with or without neck dissection.
Latest updates / special considerations (for blog to stay up to date)
-
Use of intra-operative nerve monitoring has become more common to reduce risk to facial nerve.
-
Pre-operative imaging techniques are improving (higher resolution MRI, 3T MRI) aiding in surgical planning.
-
Less invasive approaches (where feasible) to reduce morbidity - mention but emphasise that standard surgery remains mainstay.
Treatment Options of Parotid Gland Removal
The main treatment for parotid gland removal (parotidectomy) is surgery, with several distinct approaches tailored to tumor type, extent, and relationship to the facial nerve. The choice of surgical technique aims to maximize tumor control, minimize functional loss, and reduce complications.
The main surgical options
-
Superficial parotidectomy: removal of the tumour in the superficial lobe (above the facial nerve) while preserving deep lobe.
-
Total parotidectomy: removal of both superficial and deep lobes. This is done when tumour involves deep lobe or both lobes.
-
Radical parotidectomy: in malignant disease where the facial nerve is involved, sometimes the nerve and surrounding tissues must be removed.
Additional surgical considerations
-
Removal of lymph nodes (neck dissection) if malignant disease is present or suspected.
-
Reconstruction: if a large defect results, reconstructive techniques may be used to restore contour and function.
-
Use of drains, wound closure, cosmetic considerations (scar placement in front of ear/under ear crease)
Non-surgical / adjunct treatments
-
In benign lesions that are very small and asymptomatic, sometimes observation may be offered (depending on surgeon's decision).
-
Radiotherapy may be used in malignant cases post-surgery (adjuvant) or when surgery is not feasible. (Include note)
-
For obstructive gland conditions (stones) less invasive methods such as sialendoscopy may be used (though removal may still be required in some cases) - mention as a modern adjunct.
Pre-operative preparation and what to expect during surgery
-
Under general anaesthesia. Pre-op instructions: stop eating, review medications, smoking cessation.
-
Description of procedure: incision in front of ear/along hairline, careful identification of facial nerve, removal of gland/tumour, insertion of drain, closure.
-
Typical time: 2-4 hours. Hospital stay may vary (overnight or few days) depending on extent.
Post-operative care & recovery
-
Pain management, wound care (keeping incision dry, drain management).
-
Monitoring for facial nerve function immediately after surgery.
-
Gradual return to normal activity; heavy lifting/strenuous activity may be avoided for 4-6 weeks (or per surgeon advice).
-
Follow-up visits: removal of sutures, drain removal, longer term monitoring especially in malignant cases (for recurrence)
Outlook and prognosis
-
For benign tumours, prognosis after complete removal is very good.
-
For malignant tumours, the outcome depends on tumour type, stage, margin status, nerve involvement.
-
Emphasise that surgical removal is aimed for cure or control, and early diagnosis improves outcomes.
Prevention and Management of Parotid Gland Removal
Prevention and management before and after parotid gland removal (parotidectomy) focus on careful preoperative planning, minimizing surgical risks, promoting effective wound healing, and addressing complications quickly to ensure optimal recovery and long-term function.
Prevention (or early detection) of underlying disease
-
Since removal is a treatment rather than something you prevent, focus here on prevention of gland disease that leads to removal:
-
Avoid or minimise risk factors: e.g., reduce exposure to ionising radiation to head/neck when possible.
-
Maintain good oral hygiene, manage recurrent infections of salivary glands promptly.
-
For salivary stones: if symptomatic, early treatment to prevent gland damage.
-
For benign lumps: regular monitoring if small and asymptomatic, seeking ENT evaluation if new swelling in parotid region.
-
Management (pre- and post-surgery)
-
Pre-surgery: optimise general health (e.g., control diabetes, hypertension, stop smoking) to reduce surgical risks.
-
Post-surgery:
-
Wound care, follow instructions re: dressing, drain management, hygiene.
-
Facial nerve exercises or physiotherapy if there is temporary weakness.
-
Monitor for signs of complications (see next section) and follow up regularly.
-
Long-term: For malignant cases, ongoing surveillance is important to detect recurrence early.
-
-
Lifestyle management:
-
Diet: after surgery, soft food initially; hydration; good nutrition to support healing.
-
Activity: avoid heavy exertion until cleared by surgeon.
-
Scar management: massage, sun protection to help scar fade over time.
-
Role of patient education and support
-
Inform patient about what to expect, typical recovery timeline, potential nerve issues, scar appearance, follow-up schedule.
-
Encourage emotional/psychological support, because head & neck surgery can have cosmetic and functional consequences.
Complications of Parotid Gland Removal
Parotid gland removal (parotidectomy) can lead to several complications ranging from mild, transient issues to more serious long-term effects. The most notable risks include facial nerve palsy, Frey's syndrome, wound problems, infection, and cosmetic concerns.
Common and important complications
-
Facial nerve injury/weakness: Because the facial nerve runs through the parotid gland, surgical manipulation can cause temporary or, less commonly, permanent weakness.
-
Numbness of earlobe/skin area: The greater auricular nerve may be affected, leading to numbness around the ear/neck region.
-
Salivary fistula / sialocele: Leakage of saliva from the remaining gland tissue or duct may form a fluid collection (sialocele) or fistula.
-
Frey's syndrome (gustatory sweating): Sweating and flushing over the parotid region when eating due to aberrant nerve regeneration. This is a known late complication.
-
Bleeding / hematoma: Post-operative bleeding under the skin flap can occur; hence drains are used.
-
Infection: As with any surgery, risk of wound infection or deeper infection.
-
Scar / cosmetic issues: Depression in cheek contour if large tissue removed; visible scar; asymmetry of face.
Rare but serious complications
-
Permanent facial paralysis (if nerve must be sacrificed).
-
Recurrence of tumour (for malignant and some benign tumours) requiring further treatment.
-
Chronic pain, first-bite syndrome (pain on first bite of meal) - less common but noted.
How to reduce risk of complications
-
Surgeons with head & neck / parotid experience.
-
Pre-operative imaging and planning to map nerve.
-
Intra-operative nerve monitoring where appropriate.
-
Good surgical technique, patient compliance with post-op instructions (keeping drain, wound care).
-
Early recognition and management of complications (e.g., sialocele aspiration, physiotherapy for facial weakness).
Living with the Condition of Parotid Gland Removal
Living with the condition after parotid gland removal (parotidectomy) generally brings good long-term quality of life and recovery for most patients, yet it often requires adjustment to some persistent sensory changes and minor functional or cosmetic effects. Most people adapt well over time, with satisfaction increasing in the months and years after surgery.
What patients may expect after surgery
-
Recovery timeline: Many patients return to usual daily activities within a few weeks, but full recovery (especially nerve function) may take months.
-
Scar: Initially the scar may be visible; over months it usually fades and becomes less conspicuous, often hidden in natural creases near ear/neck.
-
Facial nerve function: If minor weakness, this may improve gradually; physiotherapy or facial exercises may help.
-
Sensation changes: Numbness of earlobe/cheek may persist but often becomes less bothersome with time.
-
Cosmetic contour: In cases of total gland removal, some hollowing (depression) of cheek might occur; reconstructed in some cases. You may mention massage, fillers or fat grafting as options.
Long-term follow-up
-
For malignant tumours: periodic follow-ups (every 1-3 months in year 1, then spaced out) to monitor for recurrence.
-
For benign tumours: regular check-ups to ensure no recurrence (though rare with complete removal).
-
Functional monitoring: saliva production may be reduced; talk about dry mouth management if relevant.
Quality of life considerations
-
Eating: if first-bite syndrome or gustatory sweating occur, they can affect meals. Strategies such as avoiding very spicy/sour foods, using antiperspirant for Frey's syndrome may help.
-
Emotional/psychological impact: Because surgery involves head/neck and may affect appearance and facial movement, counselling and support groups may be beneficial.
-
Supportive therapies: facial physiotherapy, scar massage, occupational therapy (if needed).
-
Lifestyle: maintaining good oral hygiene, hydration, and avoiding trauma to operated area (e.g., protecting the scar from sun).
Tips for patients
-
Follow surgeon's post-operative instructions strictly (drain care, wound hygiene, activity limitations).
-
Report any signs of infection, new swelling, worsening facial weakness promptly.
-
Maintain follow-up appointments; keep a record of your baseline and any changes.
-
Be patient: nerve recovery may take months; improvements may be gradual.
-
Seek help if concerned about appearance, contour issues or functional problems - modern reconstructive options exist.
Top 10 Frequently Asked Questions about Parotid Gland Removal
1. What is parotid gland removal?
Parotid gland removal, also known as parotidectomy, is a surgical procedure to remove all or part of the parotid gland-the largest salivary gland located in front of and below the ear. Surgery is often performed to remove tumors (benign or malignant), chronic infections, or stones that block saliva flow. The procedure aims to treat disease while preserving important facial structures, particularly the facial nerve.
2. Why is parotid gland removal performed?
Parotid gland removal is indicated for:
-
Benign tumors like pleomorphic adenomas or Warthin's tumor
-
Malignant tumors such as mucoepidermoid carcinoma or adenoid cystic carcinoma
-
Chronic parotitis or repeated infections that do not respond to medication
-
Obstructive salivary stones causing pain or swelling
-
Cysts or abscesses within the gland
Surgery helps relieve symptoms, prevent recurrence, and remove cancerous growths when present.
3. Who is a candidate for parotidectomy?
Candidates include:
-
Patients with confirmed tumors, cysts, or stones in the parotid gland
-
Individuals with chronic infections or inflammation unresponsive to medical treatment
-
Patients who are healthy enough for surgery and anesthesia
-
Individuals requiring cosmetic and functional preservation of the face, particularly the facial nerve
Preoperative evaluation includes physical examination, imaging (ultrasound, CT, MRI), and sometimes fine-needle aspiration to identify the nature of the lesion.
4. How is parotid gland removal performed?
Parotidectomy is performed under general anesthesia. The surgical approach depends on the tumor's location and type:
-
Superficial parotidectomy: Removes the outer portion of the gland, usually for benign tumors.
-
Total parotidectomy: Removes the entire gland, often required for malignant tumors.
-
Extracapsular dissection: Minimally invasive removal of small, well-defined tumors.
During surgery, the facial nerve is carefully identified and preserved to maintain facial movement. Incisions are typically made in front of the ear and extend to the neck for cosmetic and functional reasons.
5. What are the benefits of parotid gland removal?
-
Eliminates tumors or stones, preventing further growth or complications
-
Reduces pain, swelling, and infection
-
Prevents spread of malignant tumors
-
Preserves facial nerve function in most cases
-
Improves quality of life by restoring normal salivary function and reducing recurrent infections
Patients usually notice significant improvement in symptoms and comfort after recovery.
6. Is parotid gland removal painful?
During surgery, general anesthesia ensures no pain is felt. Post-operative discomfort may include:
-
Mild to moderate pain or tenderness around the incision
-
Swelling or bruising near the ear and cheek
-
Temporary numbness around the surgical site
Pain is typically managed with prescribed analgesics, and most discomfort resolves within 1-2 weeks.
7. What are the risks and complications of parotidectomy?
Although generally safe, potential risks include:
-
Facial nerve injury, causing temporary or rare permanent weakness on one side of the face
-
Infection at the surgical site
-
Bleeding or hematoma formation
-
Salivary fistula, where saliva leaks through the incision
-
Frey's syndrome, causing sweating on the cheek during eating
-
Scar formation, usually minimal and hidden along natural lines
Experienced surgeons take measures to protect the facial nerve and minimize complications.
8. What is the recovery process after parotid gland removal?
Recovery involves:
-
Hospital stay: Often 1-3 days depending on the surgery's complexity
-
Activity restrictions: Avoid strenuous activity and heavy lifting for 2-4 weeks
-
Incision care: Keep the area clean, watch for redness or swelling
-
Drain care: Temporary drains may be placed to prevent fluid accumulation
-
Follow-up visits: Monitor healing, facial nerve function, and tumor recurrence
Most patients resume normal activities within a few weeks, with gradual improvement in comfort and facial movement.
9. How long does it take to regain normal facial function and appearance?
-
Mild swelling and bruising usually resolve in 1-2 weeks
-
Facial nerve function is monitored; temporary weakness may resolve over weeks to months
-
Scar appearance improves gradually, often becoming barely noticeable
-
Long-term results include restored comfort, resolution of symptoms, and a normal-looking neck and face
10. How much does parotid gland removal cost, and is it covered by insurance?
The cost depends on:
-
Hospital and surgeon fees
-
Anesthesia and operating room charges
-
Post-operative care, including imaging and follow-up visits
Parotidectomy is usually medically necessary, particularly for tumors or chronic infections, and is covered by most insurance plans. Cosmetic concerns alone may not be fully covered. Patients should confirm coverage, co-pays, and out-of-pocket costs with their insurance provider.


