Introduction to Partial Shoulder Endoprosthesis
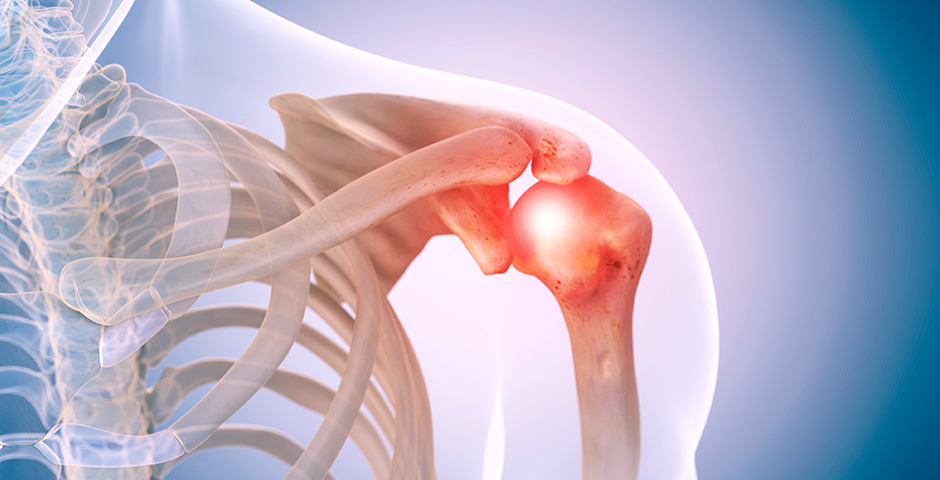
A Partial Shoulder Endoprosthesis is a specialized surgical implant used to replace only a portion of the shoulder joint, usually the humeral head, while preserving the patient's natural glenoid (shoulder socket). Unlike total shoulder replacement, which replaces both the humeral head and glenoid, partial endoprosthesis focuses on targeted reconstruction. This procedure is also known as hemiarthroplasty and is primarily indicated for patients with severe humeral head damage due to fractures, arthritis, avascular necrosis, or tumors.
The shoulder is one of the most mobile joints in the body, enabling a wide range of motion for daily activities such as lifting, pushing, and rotating. Because of its mobility, the shoulder is prone to injuries, degenerative conditions, and tumors that can compromise joint function. Partial shoulder endoprosthesis allows surgeons to restore function, reduce pain, and maintain as much natural anatomy as possible, especially in younger or active patients where preserving the glenoid is advantageous.
Modern surgical techniques have evolved to include modular implants, minimally invasive approaches, and patient-specific prosthesis design. These advancements improve outcomes, reduce complications, and promote faster recovery. This guide provides a comprehensive overview of indications, causes, risk factors, symptoms, diagnosis, treatment, prevention, complications, and long-term living considerations for partial shoulder endoprosthesis.
Causes and Risk Factors Leading to Partial Shoulder Endoprosthesis
Partial shoulder endoprosthesis is indicated primarily when the humeral head is damaged but the glenoid remains relatively intact. The most common causes include:
A. Causes
-
Traumatic Shoulder Fractures
-
Complex proximal humerus fractures that cannot be reconstructed by plates or screws.
-
Fractures with bone loss or compromised blood supply to the humeral head.
-
-
Osteoarthritis of the Humeral Head
-
Degeneration of the humeral head cartilage leading to pain and limited mobility.
-
Partial replacement may preserve healthy glenoid cartilage.
-
-
Avascular Necrosis (Osteonecrosis)
-
Loss of blood supply to the humeral head results in bone collapse.
-
Hemiarthroplasty restores joint anatomy and alleviates pain.
-
-
Tumors of the Proximal Humerus
-
Primary bone tumors or metastatic lesions may necessitate partial replacement after tumor resection.
-
-
Failed Previous Surgery
-
Previous internal fixation failures, nonunion of fractures, or complications from prior shoulder procedures may warrant hemiarthroplasty.
-
B. Risk Factors
-
Advanced age: Older adults are more prone to fractures and degenerative changes.
-
Osteoporosis: Weakens the proximal humerus, increasing fracture risk.
-
High-energy trauma: Sports injuries, falls, or accidents can damage the humeral head.
-
Chronic shoulder overuse: Repetitive overhead activities increase wear and tear.
-
Metabolic or vascular disorders: Conditions affecting bone health may predispose to avascular necrosis.
Early identification of risk factors allows preventive measures, optimized surgical planning, and better postoperative outcomes.
Symptoms and Signs Indicating Partial Shoulder Endoprosthesis
Patients who may require partial shoulder replacement often present with a combination of pain, functional limitation, and structural deformity.
A. Pain
-
Chronic pain localized to the shoulder joint, especially at night or during overhead activities.
-
Pain may result from arthritis, fracture malunion, or avascular necrosis.
B. Limited Range of Motion
-
Difficulty lifting the arm, reaching behind the back, or performing daily tasks.
-
Stiffness due to joint degeneration or post-traumatic changes.
C. Deformity or Visible Abnormality
-
Shoulder may appear flattened or asymmetric in cases of humeral head collapse.
-
Malalignment after fracture can alter shoulder contour.
D. Weakness
-
Inability to lift objects overhead.
-
Reduced strength during pushing or pulling movements.
E. Signs Specific to Underlying Causes
-
Swelling and tenderness (fracture or acute injury)
-
Audible clicking or grinding (degenerative changes)
-
Functional impairment disproportionate to pain (tumor involvement)
Recognizing these symptoms early ensures timely surgical consultation and improved outcomes.
Diagnosis of Partial Shoulder Endoprosthesis Candidates
Diagnosis of candidates for partial shoulder endoprosthesis (hemiarthroplasty) involves a combination of clinical assessment, imaging, and evaluation of the patient's functional needs and underlying pathology. Typical candidates are those with specific shoulder conditions where only the humeral head (ball) is replaced, not the glenoid (socket).
A. Clinical Evaluation
-
Detailed medical and surgical history.
-
Physical examination assessing shoulder alignment, range of motion, strength, and stability.
-
Evaluation of rotator cuff integrity.
-
Assessment of neurological function to rule out nerve injuries.
B. Imaging Studies
-
X-rays
-
Determine fracture patterns, degenerative changes, humeral head collapse, and alignment.
-
-
CT Scan
-
Provides 3D visualization of fracture fragments, bone loss, or tumor involvement.
-
-
MRI
-
Evaluates soft tissue structures including rotator cuff tendons, cartilage, and labrum.
-
-
Bone Scan or PET Scan
-
Used if tumor involvement is suspected.
-
C. Laboratory Tests
-
Routine preoperative blood work for surgical clearance.
-
Tumor markers if malignancy is suspected.
-
Inflammatory markers if infection is suspected.
Treatment Options for Partial Shoulder Endoprosthesis
Treatment for partial shoulder endoprosthesis-also called shoulder hemiarthroplasty-involves replacing the damaged humeral head (the ball of the shoulder joint) with an artificial implant, while leaving the glenoid (socket) untouched. The approach is tailored based on the patient's anatomy and underlying disease.
A. Surgical Treatment
Partial shoulder replacement is the primary treatment for irreparable humeral head damage.
Types of Partial Shoulder Endoprosthesis
-
Standard Hemiarthroplasty
-
Replaces only the humeral head while preserving the glenoid.
-
Indicated for fractures, osteonecrosis, or localized arthritis.
-
-
Tumor Endoprosthesis
-
Modular or custom-designed prosthesis to reconstruct proximal humerus after tumor resection.
-
-
Modular/Custom Implants
-
Allows precise anatomical reconstruction.
-
Accommodates variable bone quality and size.
-
B. Non-Surgical Management (Limited Role)
-
Physical therapy for mild osteoarthritis or partial fractures.
-
Pain management with NSAIDs or corticosteroid injections.
-
Activity modification and bracing.
-
Non-surgical approaches are usually temporary and cannot restore severe structural damage.
C. Surgical Procedure Overview
-
Patient positioned in beach-chair or supine position.
-
Surgical approach via deltopectoral or anterolateral incision.
-
Humeral head excised carefully.
-
Prosthesis implanted and fixed with or without cement.
-
Rotator cuff repaired and tension checked.
-
Wound closed and postoperative drain inserted if required.
D. Postoperative Rehabilitation
-
Early passive range of motion exercises.
-
Gradual progression to active-assisted and active exercises.
-
Strengthening of rotator cuff and deltoid muscles.
-
Regular follow-up imaging to monitor implant position.
Prevention and Management of Partial Shoulder Endoprosthesis
Prevention and management after partial shoulder endoprosthesis (hemiarthroplasty) focus on protecting the surgical repair, preventing complications, and ensuring optimal recovery through a tailored rehabilitation program.
A. Prevention
-
Fall prevention strategies in older adults.
-
Bone-strengthening measures such as calcium, vitamin D, and weight-bearing exercises.
-
Avoidance of high-risk activities that may cause fractures.
-
Early treatment of arthritis and rotator cuff injuries.
B. Preoperative Management
-
Optimize overall health (blood pressure, diabetes, nutrition).
-
Evaluate bone quality for implant selection.
-
Treat existing infections or inflammation.
-
Prehabilitation exercises to strengthen surrounding muscles.
C. Postoperative Management
-
Pain control and wound care.
-
Gradual rehabilitation protocol to restore motion and strength.
-
Long-term monitoring for implant loosening or wear.
-
Education on safe activities to prevent dislocation or fractures.
Complications of Partial Shoulder Endoprosthesis
Partial shoulder endoprosthesis (shoulder hemiarthroplasty) is effective for selected shoulder conditions, but it carries risks of early and late complications that can impact function and quality of life.
Though generally safe, complications can occur:
-
Infection
-
Superficial or deep; may require antibiotics or revision surgery.
-
-
Dislocation
-
Rare; proper prosthesis positioning reduces risk.
-
-
Prosthetic Loosening or Wear
-
Over time, implant may loosen, requiring revision.
-
-
Rotator Cuff Injury
-
Undiagnosed cuff tears can impair function.
-
-
Fracture
-
Periprosthetic fracture during or after surgery.
-
-
Nerve or Blood Vessel Injury
-
Axillary nerve or brachial plexus may be affected.
-
-
Pain or Stiffness
-
Persistent pain may indicate improper implant positioning or rotator cuff dysfunction.
-
Living with Partial Shoulder Endoprosthesis
Living with a partial shoulder endoprosthesis (hemiarthroplasty) often enables meaningful pain relief and functional improvement, but optimal results depend on patient commitment to rehabilitation and adaptation to lifelong joint care. Most individuals return to daily routines, though some limitations and unique long-term considerations persist.
A. Recovery Timeline
-
Hospital stay: 2-5 days.
-
Early mobility: Passive exercises begin within days.
-
Full functional recovery: 3-6 months depending on age, rotator cuff integrity, and rehabilitation.
B. Daily Life Considerations
-
Avoid heavy lifting for the first 6-12 weeks.
-
Gradual return to normal activities and sports.
-
Regular physiotherapy to maintain strength and mobility.
-
Awareness of implant limitations to prevent overuse.
C. Long-Term Prognosis
-
Most patients achieve significant pain relief and improved shoulder function.
-
Lifespan of the prosthesis varies, but modern implants last 10-20 years.
-
Revision surgery may be needed for wear, loosening, or recurrent problems.
D. Emotional and Social Considerations
-
Counseling may help adjust to limited motion initially.
-
Support groups for joint replacement patients can provide guidance and motivation.
Top 10 Frequently Asked Questions about Partial Shoulder Endoprosthesis
1. What is a partial shoulder endoprosthesis?
A partial shoulder endoprosthesis is a type of shoulder joint replacement surgery in which only part of the shoulder joint is replaced. Specifically, the humeral head (the ball of the upper arm bone) is replaced with a prosthetic implant while keeping the glenoid (the socket) intact. This procedure is typically performed for patients with severe damage to the humeral head due to arthritis, trauma, or avascular necrosis, while the socket remains healthy.
2. Why is partial shoulder replacement performed?
Partial shoulder endoprosthesis is indicated for patients with:
-
Osteoarthritis or degenerative joint disease affecting the humeral head
-
Avascular necrosis, where blood supply to the humeral head is compromised
-
Traumatic fractures of the humeral head not amenable to fixation
-
Severe shoulder pain, stiffness, or loss of function not relieved by conservative treatments
The surgery aims to relieve pain, restore function, and improve range of motion while preserving as much of the natural joint as possible.
3. Who is a candidate for partial shoulder endoprosthesis?
Ideal candidates include:
-
Patients with localized damage to the humeral head and an intact glenoid
-
Individuals with severe shoulder pain or limited mobility despite non-surgical treatments
-
Patients in good general health able to undergo anesthesia and rehabilitation
-
Those without active infections or significant rotator cuff damage
Preoperative evaluation includes X-rays, MRI or CT scans, and a thorough physical examination to determine joint integrity and suitability for partial replacement.
4. How is partial shoulder endoprosthesis performed?
The procedure is performed under general anesthesia and typically involves:
-
Incision: A surgical cut over the shoulder to access the joint.
-
Removal of damaged humeral head: The diseased bone is carefully removed.
-
Insertion of prosthetic implant: A metal or ceramic humeral head prosthesis is placed and secured in the humerus.
-
Closure: Soft tissues and muscles are repaired, and the incision is closed with sutures or staples.
Surgery usually takes 1-2 hours, and patients are monitored in the hospital for 1-2 days postoperatively.
5. What are the benefits of partial shoulder replacement?
-
Pain relief: Eliminates chronic pain caused by humeral head damage.
-
Restoration of function: Improves shoulder mobility and strength.
-
Minimally invasive compared to total replacement: Preserves the glenoid and natural joint structures.
-
Shorter recovery and rehabilitation: Compared to total shoulder arthroplasty.
-
Durability: Modern implants are designed for long-term use, often lasting 10-15 years or more.
Patients often regain daily activities and quality of life soon after surgery.
6. Is partial shoulder endoprosthesis painful?
During surgery, general anesthesia ensures no pain. After the procedure, mild to moderate pain and soreness around the shoulder are common, managed with:
-
Prescription pain medications or anti-inflammatories
-
Ice packs and gentle movement exercises
-
Post-operative physical therapy for gradual mobility improvement
Pain typically decreases over the first 2-4 weeks as healing progresses.
7. What are the risks and complications of partial shoulder replacement?
While generally safe, potential risks include:
-
Infection at the surgical site or deep within the joint
-
Prosthesis loosening or dislocation
-
Nerve or blood vessel injury around the shoulder
-
Stiffness or limited range of motion if rehabilitation is inadequate
-
Fracture of the humerus during or after surgery
-
Rare complications like blood clots or adverse reaction to anesthesia
Careful surgical technique and adherence to post-operative care significantly reduce risks.
8. What is the recovery process after partial shoulder replacement?
-
Hospital stay: Typically 1-2 days for monitoring.
-
Immobilization: Arm may be kept in a sling for 2-4 weeks.
-
Physical therapy: Begins soon after surgery, focusing on gentle
range-of-motion exercises followed by strengthening.
-
Activity restrictions: Avoid heavy lifting or overhead
activities for several weeks.
-
Follow-up: Regular visits to monitor healing, implant
positioning, and shoulder function.
Hospital stay: Typically 1-2 days for monitoring.
Immobilization: Arm may be kept in a sling for 2-4 weeks.
Physical therapy: Begins soon after surgery, focusing on gentle range-of-motion exercises followed by strengthening.
Activity restrictions: Avoid heavy lifting or overhead activities for several weeks.
Follow-up: Regular visits to monitor healing, implant positioning, and shoulder function.
Most patients regain functional range of motion within 3-6 months, depending on age and preoperative condition.
9. How long does a partial shoulder endoprosthesis last?
Modern humeral head implants are designed to last 10-15 years or more, depending on activity level, age, and post-operative care. Partial shoulder replacement preserves more natural tissue, which can extend implant longevity compared to total shoulder replacement in selected patients.
10. How much does partial shoulder replacement cost, and is it covered by insurance?
The cost depends on:
-
Hospital and surgeon fees
-
Anesthesia and operating room charges
-
Implant type and post-operative care
Partial shoulder replacement is usually considered medically necessary for severe arthritis, trauma, or avascular necrosis, and most insurance plans cover the procedure, including hospital stay and follow-up care. Cosmetic or elective replacements may not be fully covered. Patients should confirm coverage, co-pays, and out-of-pocket expenses before surgery.


