Introduction to PCNL
Percutaneous Nephrolithotomy (PCNL) is a minimally invasive surgical procedure designed to remove large or complex kidney stones. Unlike traditional open surgery, PCNL requires only a small incision in the back or flank area, through which a narrow tube (called a nephroscope) is inserted directly into the kidney. Using specialized instruments, the surgeon fragments and removes the stones, often in a single session. The procedure has revolutionized kidney stone management, particularly for stones larger than 20 mm, staghorn calculi (stones that occupy multiple parts of the kidney), or stones that cannot be effectively treated with less-invasive methods such as shockwave therapy or ureteroscopy.
PCNL combines modern imaging technology, precise surgical technique, and specialized lithotripsy devices to achieve high success rates with minimal recovery time. The procedure is performed under general anesthesia, and patients often experience significant relief from pain and obstruction after surgery. With the advancement of miniaturized PCNL (mini-PCNL, ultra-mini, and micro-PCNL), the procedure has become even safer, reducing complications, minimizing blood loss, and allowing for faster recovery. The main goal of PCNL is complete stone clearance, preservation of renal function, and prevention of recurrent stone formation.
Causes and Risk Factors for Conditions Requiring PCNL
PCNL is indicated primarily for kidney stones that are large, complex, or resistant to conventional treatments. The main causes include:
-
Large kidney stones: Stones larger than 20 mm, including those filling multiple calyces, are difficult to treat with shockwave therapy or ureteroscopy.
-
Staghorn calculi: Complex stones that occupy multiple calyces can impair kidney function and increase the risk of infection.
-
Recurrent stones: Patients who have previously had stones that have not fully cleared may require PCNL to remove residual fragments.
-
Obstructive stones: Stones that block urine flow, leading to hydronephrosis (swelling of the kidney) or recurrent infections.
-
Hard or resistant stones: Certain stone compositions, such as cystine or calcium oxalate monohydrate stones, are resistant to less-invasive fragmentation techniques.
Risk factors for developing complex stones that may require PCNL include:
-
Poor hydration or chronic dehydration, which concentrates urine and promotes stone formation.
-
Metabolic disorders, such as hyperparathyroidism, high uric acid levels, or cystinuria.
-
Chronic urinary tract infections, which can lead to struvite stones.
-
Anatomical abnormalities of the kidney or ureter, such as calyceal diverticula or horseshoe kidneys.
-
Dietary factors, including high intake of oxalates, sodium, or animal protein.
-
Obesity and sedentary lifestyle.
-
Genetic predisposition and family history of kidney stones.
Identifying the underlying cause of stone formation is crucial not only for surgical planning but also for preventing recurrence after PCNL.
Symptoms and Signs of Kidney Stones Requiring PCNL
Patients with stones requiring PCNL often present with symptoms that reflect both the size and location of the stone. Common signs and symptoms include:
-
Flank pain: Sharp, severe pain in the back or side, often radiating toward the groin. Pain may come in waves (renal colic) and intensify during stone movement.
-
Hematuria: Blood in the urine, which may be visible (red or pink) or microscopic. Stones can scratch the urinary tract lining, causing bleeding.
-
Recurrent urinary tract infections: Infected stones can harbor bacteria, leading to persistent infections, fever, or even sepsis.
-
Obstructive symptoms: Decreased urine output, swelling of the affected kidney (hydronephrosis), nausea, and sometimes vomiting.
-
Chronic dull pain: In large or staghorn stones, patients may experience ongoing discomfort rather than acute pain.
-
Systemic signs: Fever, malaise, or loss of appetite may occur if infection accompanies the stone.
Early recognition of these symptoms is essential, as prolonged obstruction can lead to permanent kidney damage. Large or complex stones often remain asymptomatic for months, making imaging crucial for timely diagnosis and treatment planning.
Diagnosis of Conditions Requiring PCNL
The diagnosis of kidney stones begins with a thorough medical history and physical examination, focusing on the onset, location, severity of pain, prior stone history, and associated urinary symptoms.
Laboratory tests include:
-
Urinalysis to detect blood, crystals, or infection.
-
Urine culture to identify bacteria if infection is suspected.
-
Blood tests to evaluate kidney function (creatinine, eGFR), electrolyte balance, calcium, uric acid, and parathyroid hormone levels if metabolic disorders are suspected.
Imaging studies are critical in PCNL planning:
-
Non-contrast CT scan is the gold standard, providing precise information on stone size, density, location, and kidney anatomy.
-
Ultrasound is useful to detect hydronephrosis and larger stones, particularly in patients where radiation exposure should be minimized.
-
X-ray (KUB) may be used for follow-up, especially for radiopaque stones.
Specialized tests: For recurrent stones, 24-hour urine collection assesses calcium, oxalate, citrate, uric acid, and other stone-forming components. Imaging also guides surgical planning, including tract placement, patient positioning (prone or supine), and the need for single or multiple tracts.
Treatment Options for Kidney Stones
Non-Surgical Treatment
-
Hydration and pain management: Small stones may pass spontaneously with adequate fluid intake and analgesics.
-
Medical therapy: Medications may include alpha-blockers (to relax ureter muscles) or drugs targeting metabolic causes (thiazides, potassium citrate, allopurinol).
-
Extracorporeal Shock Wave Lithotripsy (ESWL): Uses sound waves to fragment stones, effective for small, uncomplicated stones.
Surgical Treatment: PCNL
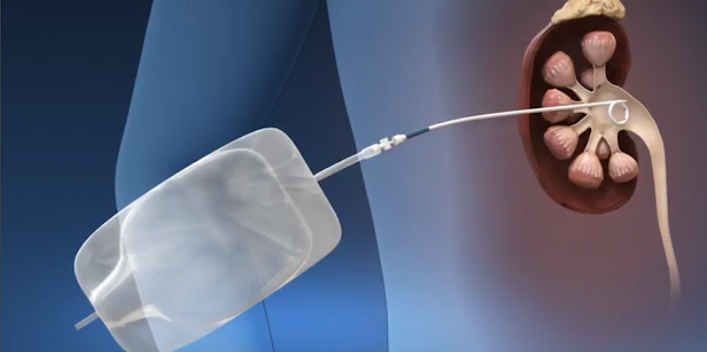
PCNL is preferred for large, complex, or refractory stones. The procedure includes:
-
Patient positioning (usually prone, sometimes supine).
-
Creation of a small skin incision over the flank.
-
Percutaneous access to the kidney using imaging guidance.
-
Insertion of a nephroscope to visualize and fragment stones with ultrasound, laser, or pneumatic lithotripsy.
-
Removal of fragments through the tract.
-
Placement of a nephrostomy tube if necessary.
Mini-PCNL and Micro-PCNL use smaller tracts to reduce bleeding, pain, and recovery time while maintaining high stone clearance rates.
Other Surgical Options
-
Open or robotic surgery is rarely needed, reserved for extremely complex stones or abnormal anatomy.
-
Ureteroscopy may be used in conjunction with PCNL for residual stones.
Prevention and Long-Term Management
Preventing recurrence is as important as treating existing stones:
-
Hydration: Maintain urine output of >2.5 L/day.
-
Dietary modifications: Reduce high-oxalate foods, moderate sodium, limit excessive animal protein, ensure adequate calcium intake.
-
Medical therapy: Use medications tailored to metabolic abnormalities detected on urine and blood tests.
-
Infection control: Prompt treatment of UTIs to prevent struvite stone formation.
-
Follow-up imaging: Ultrasound or CT to monitor residual fragments or recurrence.
-
Lifestyle: Weight management, regular physical activity, avoid dehydration, and minimize stone-promoting supplements.
-
Kidney health: Monitor blood pressure, diabetes, and renal function over time.
Complications of PCNL
While PCNL is minimally invasive, complications may occur:
-
Bleeding: Most common serious complication; may require transfusion or embolization.
-
Infection/sepsis: Preoperative sterile urine culture and antibiotics are crucial.
-
Injury to adjacent organs: Rare but possible (colon, spleen, pleura).
-
Residual stones: Some fragments may remain, requiring secondary procedures.
-
Urinary leaks, fistula, or nephrostomy tract complications.
-
Postoperative pain, hematoma, or prolonged recovery.
-
Long-term risks: Recurrent stones if underlying metabolic issues are not addressed, or kidney function decline if obstruction persists.
Living with Kidney Stones and Post-PCNL Recovery
Living with kidney stones before PCNL can involve repeated pain attacks, dietary restrictions, infections, and anxiety about kidney health. Post-PCNL recovery typically includes:
-
Hospital stay of 1-2 days for uncomplicated cases.
-
Limited physical activity for several weeks.
-
Monitoring of urine output, pain management, and nephrostomy care if present.
-
Gradual resumption of normal diet and daily activities.
-
Regular follow-up imaging and metabolic evaluation to prevent recurrence.
-
Patients often experience dramatic relief from pain and obstruction after PCNL, improved kidney drainage, and reduced infection risk.
Long-term outlook is excellent when preventive strategies are followed, and patients can maintain kidney health and a stone-free life. Lifestyle modifications, hydration, dietary management, and ongoing medical follow-up are essential to prevent new stone formation and protect renal function.
Top 10 Frequently Asked Questions about PCNL (Percutaneous Nephrolithotomy)
1. What is PCNL (Percutaneous Nephrolithotomy)?
Percutaneous Nephrolithotomy, commonly referred to as PCNL, is a minimally invasive surgical procedure for removing kidney stones that are too large, complex, or dense to be treated with other non-invasive methods such as shock wave lithotripsy (SWL) or ureteroscopy. In PCNL, a small incision is made in the patient's back, and a thin tube called a nephroscope is inserted directly into the kidney. Specialized instruments are then used to visualize, fragment, and remove stones while preserving kidney tissue. This procedure is particularly effective for large stones (>2 cm), staghorn calculi, or multiple stones.
2. Why is PCNL performed?
PCNL is indicated in patients who have:
-
Large kidney stones that cannot be managed with SWL or ureteroscopy
-
Complex stones, such as staghorn calculi occupying multiple parts of the kidney
-
Resistant stones that have failed prior non-invasive treatments
-
Symptomatic stones causing severe pain, urinary obstruction, recurrent infections, or hematuria
-
Kidney damage risk, where stones threaten kidney function
PCNL allows complete stone removal in a single procedure, relieving pain, preventing recurrent infections, and protecting kidney function.
3. Who is a candidate for PCNL?
PCNL is suitable for patients with:
-
Large, hard, or complex kidney stones
-
Stones causing obstruction, infection, or recurrent urinary tract problems
-
Failed prior treatments like SWL or ureteroscopy
-
Overall good health, including stable cardiovascular and pulmonary function, to tolerate general anesthesia
Patients with uncontrolled urinary infections, bleeding disorders, or certain anatomical abnormalities may need preoperative management or alternative procedures before undergoing PCNL.
4. How is PCNL performed?
PCNL is performed under general anesthesia. The procedure involves:
-
Patient positioning: Typically prone (face-down) or sometimes supine, depending on stone location
-
Percutaneous access: A small needle is inserted into the kidney under imaging guidance (X-ray or ultrasound)
-
Tract dilation: The access tract is gradually widened to allow insertion of the nephroscope
-
Stone visualization and fragmentation: Stones are broken down using ultrasonic, laser, or mechanical lithotripsy
-
Stone removal: Fragments are extracted through the nephroscope
-
Drain placement: A nephrostomy tube may be temporarily placed to facilitate urine drainage and prevent obstruction
The procedure usually takes 1-3 hours, depending on the number and size of stones.
5. What are the benefits of PCNL?
-
High stone clearance rate: Effective for large and complex stones
-
Minimally invasive: Smaller incisions compared to open surgery
-
Pain relief: Alleviates symptoms caused by obstruction or stone irritation
-
Preserves kidney function: Reduces the risk of long-term kidney damage
-
Shorter recovery time: Patients often resume normal activities within 1-2 weeks
PCNL is widely preferred for complex stones because it is safe, effective, and reproducible in experienced hands.
6. Is PCNL painful?
During surgery, patients are under general anesthesia, so no pain is felt. Postoperative discomfort may include:
-
Mild flank or incision pain
-
Bruising or swelling around the surgical site
-
Temporary urinary discomfort or blood in urine
Pain is usually manageable with medications and significantly improves within a few days. Most patients are able to mobilize and begin light activities the day after surgery.
7. What are the risks and complications of PCNL?
Although PCNL is generally safe, potential complications include:
-
Bleeding, sometimes requiring transfusion
-
Infection or sepsis, especially if urinary infection is present preoperatively
-
Injury to surrounding organs, such as colon, spleen, or lungs (rare)
-
Residual stones, potentially requiring secondary procedures
-
Urine leakage from the nephrostomy tract
-
Temporary fever or flank discomfort
Most complications are rare and manageable when performed in specialized centers with experienced surgeons.
8. What is the recovery process after PCNL?
-
Hospital stay: Typically 1-3 days for monitoring
-
Activity: Avoid heavy lifting or strenuous activity for 1-2 weeks
-
Hydration: Drink plenty of fluids to flush the urinary system and prevent infection
-
Nephrostomy care: Follow instructions to prevent infection and ensure proper drainage
-
Follow-up: Imaging (X-ray or CT) is used to confirm complete stone removal
Most patients return to normal daily activities within 1-2 weeks, and full recovery occurs within a month.
9. How successful is PCNL?
PCNL has a very high success rate, with over 90% of large or complex stones completely removed in a single procedure. Factors influencing success include:
-
Stone size, number, and location
-
Kidney anatomy
-
Surgical expertise and equipment used
Residual stones, if any, can often be treated with secondary procedures such as flexible ureteroscopy.
10. How much does PCNL cost, and is it covered by insurance?
The cost of PCNL depends on:
-
Hospital and surgeon fees
-
Anesthesia and operating room charges
-
Postoperative care, imaging, and follow-up
PCNL is considered medically necessary for large or complex kidney stones and is usually covered by most health insurance plans, including hospitalization and post-operative care. Patients should verify coverage, co-pays, and out-of-pocket expenses with their insurance provider before surgery.


