Introduction to Perineal Resection of Rectum
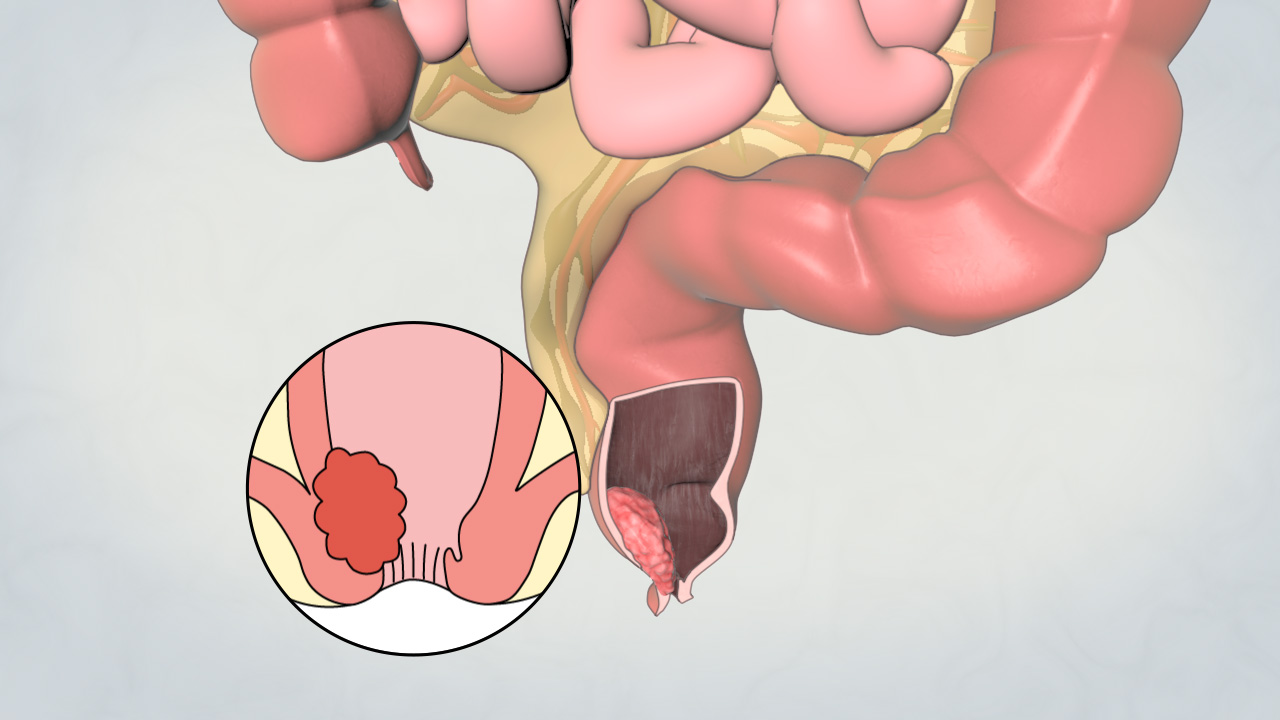
Perineal resection of the rectum is a specialized surgical procedure that involves removal of the distal rectum, often including the anal canal and surrounding mesorectum, through a perineal approach. It is primarily indicated for low rectal cancers, recurrent or residual disease, chronic inflammatory bowel disease with distal involvement, radiation-induced strictures, and severe perineal fistulas or obstruction. The rectum is a 12-15 cm muscular structure located deep in the pelvis, connected proximally to the sigmoid colon and distally to the anal canal. Its proximity to vital pelvic structures—including the bladder, prostate, seminal vesicles, vagina, ureters, and pelvic floor muscles—makes surgical intervention complex and necessitates precise planning.
The perineal approach is preferred for very low rectal lesions, particularly when sphincter-sparing techniques are not feasible. It allows direct access to the diseased tissue, facilitates complete tumor excision, and provides optimal margins while allowing for careful management of adjacent structures. This approach may be combined with abdominal mobilization of the colon, either through open, laparoscopic, or robotic-assisted surgery, to ensure complete removal of the rectum and mesorectum. The primary goals of perineal resection are: oncologic clearance in cancer cases, resolution of chronic or recurrent disease, preservation of function whenever possible, and optimizing postoperative recovery and quality of life. Preoperative counseling focuses on potential outcomes, including the possibility of permanent colostomy, changes in bowel, urinary, and sexual function, wound healing challenges, and long-term rehabilitation requirements.
Causes and Risk Factors for Perineal Resection
Perineal resection is indicated for severe or advanced rectal disease. Understanding the causes and risk factors is critical for patient selection, surgical planning, and counseling.
Underlying Causes
-
Low Rectal or Anal Canal Cancer: Tumors within 5 cm of the anal verge frequently require resection of the rectum and anal canal to achieve negative oncologic margins.
-
Recurrent Rectal Disease: Residual tumors after prior surgery or failed sphincter-preserving interventions may necessitate extensive perineal excision.
-
Inflammatory Bowel Disease (IBD): Severe Crohn's disease or ulcerative colitis with distal involvement can lead to strictures, fistulas, abscesses, or chronic infection, making surgery necessary.
-
Radiation-Induced Fibrosis or Necrosis: Previous pelvic radiotherapy may compromise tissue integrity, leading to obstruction, pain, or fistulas.
-
Pelvic Trauma: Blunt or penetrating trauma causing obstruction, chronic infection, or rectal perforation may necessitate resection.
-
Severe Obstruction or Infection: Chronic anal stenosis, perineal sepsis, or fistula formation.
Risk Factors
-
Patient-Specific: Age, obesity, diabetes, malnutrition, smoking, immunosuppression.
-
Disease-Specific: Tumor size, anal sphincter or pelvic floor involvement, prior radiation, chronic inflammation, adjacent organ invasion.
-
Procedure-Specific: Extent of resection, need for perineal flap reconstruction, multi-organ involvement, prior pelvic surgery causing adhesions.
These risk factors influence surgical planning, risk of complications, and postoperative recovery, and must be thoroughly evaluated during preoperative assessment.
Symptoms and Clinical Presentation
Patients requiring perineal resection may present with a wide range of functional, local, and systemic symptoms depending on the underlying pathology:
-
Altered Bowel Habits: Increased frequency, urgency, tenesmus, narrow-caliber stools, incomplete evacuation.
-
Rectal Bleeding: Hematochezia or occult blood; may indicate malignancy, ulceration, or chronic inflammation.
-
Pain: Chronic perineal, pelvic, or lower abdominal pain; may radiate to the sacrum or thighs.
-
Obstructive Symptoms: Difficulty passing stool, constipation, or sensation of blockage.
-
Systemic Manifestations: Weight loss, fatigue, anemia in malignancy, fever in chronic infection.
-
Fistulas and Abscesses: Chronic drainage, recurrent infections, or perineal sinus formation.
Physical Examination Findings: Palpable perineal or pelvic mass, anal canal irregularities, perineal skin changes, induration, fistula tracts, inguinal or pelvic lymphadenopathy. Functional assessment includes evaluation of continence, urinary flow, and sexual function, which helps predict postoperative outcomes.
Diagnosis and Preoperative Evaluation
A comprehensive preoperative evaluation ensures successful outcomes and patient safety:
-
Endoscopic Evaluation: Colonoscopy or sigmoidoscopy with biopsy to confirm pathology.
-
Imaging: MRI pelvis (tumor staging, sphincter and mesorectum involvement, adjacent organ invasion); CT chest/abdomen/pelvis (rule out metastasis); endorectal ultrasound for low rectal lesions.
-
Laboratory Tests: Complete blood count, electrolytes, liver and renal function, nutritional markers, coagulation profile, tumor markers (CEA in cancer), inflammatory markers (CRP, ESR in IBD).
-
Functional Assessment: Anal manometry, continence evaluation, urinary and sexual function assessment.
-
Preoperative Counselling: Explanation of permanent colostomy, wound healing expectations, functional outcomes, and psychosocial considerations.
-
Multidisciplinary Planning: Collaboration with colorectal surgeons, plastic surgeons for possible flap reconstruction, stoma care nurses, physiotherapists, and dieticians.
-
Patient Optimization: Smoking cessation, nutritional support, correction of anemia, bowel preparation, prehabilitation (exercise, pelvic floor training).
Treatment Options and Surgical Techniques
Perineal resection involves careful dissection of the rectum and anal canal, with attention to oncologic principles and functional preservation:
-
Abdominoperineal Resection (APR): Removal of the distal rectum, anal canal, and mesorectum, with creation of a permanent end colostomy.
-
Extended Resection: Incorporates adjacent organs (bladder, prostate, vagina) when invasion is present.
-
Minimally Invasive Techniques: Laparoscopic or robotic-assisted surgery for abdominal mobilization reduces trauma and accelerates recovery.
-
Pelvic Floor Reconstruction: Muscle or fasciocutaneous flaps used for perineal defects, particularly in irradiated tissue.
-
Sphincter-Preserving Options: Low anterior resection or coloanal anastomosis may be feasible if tumor allows.
-
Neoadjuvant Therapy: Preoperative chemoradiation can reduce tumor size, facilitating more conservative surgery.
-
Adjuvant Therapy: Postoperative chemotherapy or radiotherapy based on pathology and staging.
Postoperative care includes pain control, stoma education, wound management, early mobilization, and physiotherapy for pelvic floor recovery.
Prevention and Perioperative Management
Effective management involves preventing disease progression and optimizing perioperative care:
-
Disease Prevention: Routine colorectal cancer screening, early intervention for IBD, lifestyle modifications.
-
Preoperative Optimization: Nutritional support, correction of anemia, smoking cessation, diabetes control, prehabilitation, and stoma site marking.
-
Perioperative Management: Meticulous surgical technique, wound care, flap coverage when necessary, ERAS protocols including early nutrition and mobilization.
-
Postoperative Management: Pain control, colostomy support, physiotherapy for pelvic floor, infection surveillance, wound monitoring.
-
Long-Term Management: Ongoing surveillance for recurrence, stoma care, bowel habit optimization, psychosocial support, and rehabilitation.
Complications of Perineal Resection Of Rectum
Perineal resection carries early, intermediate, and long-term risks:
-
Early Complications: Intraoperative bleeding, injury to bladder/prostate/vagina, perineal wound infection, ileus, DVT/PE.
-
Intermediate Complications: Chronic perineal sinus, pelvic floor dysfunction, urinary or sexual dysfunction, perineal hernia, small bowel obstruction.
-
Long-Term Complications: Permanent colostomy complications (prolapse, parastomal hernia), chronic perineal pain, altered bowel habits, sexual dysfunction, psychological impact.
Preventive strategies include meticulous surgical technique, preoperative optimization, postoperative monitoring, and structured follow-up.
Living with the Condition After Surgery
Postoperative life requires adaptation and rehabilitation:
-
Stoma Management: Education on appliance care, skin protection, troubleshooting complications, and follow-up.
-
Bowel Function Adaptation: Dietary modification, hydration, medications for bowel regulation.
-
Pelvic Floor Rehabilitation: Physiotherapy to improve continence, mobility, and quality of life.
-
Psychosocial Support: Counseling for body image, sexual health, and social reintegration.
-
Medical Follow-Up: Ongoing surveillance for recurrence, stoma assessment, long-term bowel function monitoring, and quality-of-life evaluation.
Patients can regain independence and maintain a fulfilling lifestyle with structured education, support, and rehabilitation.
Top 10 Frequently Asked Questions about Perineal Resection of the Rectum
1. What is perineal resection of the rectum?
Perineal resection of the rectum is a surgical procedure to remove part or all of the rectum through an incision in the perineum (the area between the anus and the genitals). It is usually performed to treat rectal cancer, severe rectal disease, or trauma. The goal is to remove diseased tissue, relieve symptoms, and restore bowel function.
2. Why is perineal rectal resection performed?
This surgery is performed in cases of:
-
Rectal cancer, especially low-lying tumors near the anus
-
Severe rectal prolapse
-
Inflammatory bowel disease (e.g., Crohn's disease, ulcerative colitis) with localized disease
-
Trauma or injury to the rectum
-
Palliative care, to relieve obstruction or bleeding in advanced disease
Perineal resection helps eliminate diseased tissue, improve quality of life, and prevent complications.
3. Who is a candidate for perineal rectal resection?
Candidates include patients with:
-
Rectal disease confined to the distal rectum or anal canal
-
Tumors or lesions unsuitable for minimally invasive or local excision
-
Good overall health to tolerate anesthesia and surgery
-
No severe comorbidities that increase surgical risk
A thorough evaluation, including colonoscopy, MRI or CT scans, and biopsy, helps determine suitability.
4. How is perineal rectal resection performed?
Perineal resection is usually performed under general anesthesia:
-
Positioning: Patient lies in the lithotomy or prone position.
-
Incision: A surgical incision is made in the perineum.
-
Rectum removal: Diseased part of the rectum is excised carefully.
-
Reconstruction: Depending on the extent, the colon may be reconnected to the anus or a temporary/permanent colostomy may be created.
-
Closure: Soft tissues and skin are sutured, and drainage may be placed if needed.
The procedure is tailored to disease extent, tumor location, and patient anatomy.
5. What are the benefits of perineal rectal resection?
-
Removes diseased or cancerous tissue
-
Relieves symptoms such as bleeding, pain, or obstruction
-
Prevents disease progression, including metastasis in cancer
-
Improves bowel function or allows safe stoma creation
-
Enhances quality of life, especially in patients with advanced disease
It is often chosen for tumors low in the rectum where abdominal approaches may not be feasible.
6. Is perineal rectal resection painful?
During surgery, general anesthesia ensures no pain. After surgery, patients may experience:
-
Pain at the incision site
-
Discomfort or pressure in the perineal region
-
Mild swelling or bruising
Pain is typically managed with analgesics, local care, and supportive positioning. Most patients report gradual improvement over days to weeks.
7. What are the risks and complications?
Perineal rectal resection is generally safe but carries risks:
-
Infection at the incision site or within the pelvis
-
Bleeding or hematoma formation
-
Anastomotic leak if the colon is reconnected
-
Urinary or sexual dysfunction, especially in extensive resections
-
Stoma-related complications, if a colostomy is created
-
Rare complications like deep vein thrombosis, pulmonary embolism, or anesthesia-related issues
Careful surgical planning and post-operative monitoring minimize these risks.
8. What is the recovery process after perineal rectal resection?
-
Hospital stay: Typically 5-10 days, depending on complexity
-
Activity: Light movement encouraged early; avoid heavy lifting for several weeks
-
Wound care: Keep the perineal incision clean and dry; monitor for infection
-
Bowel management: Gradual diet advancement; stool softeners may be prescribed
-
Follow-up: Regular visits to monitor wound healing, bowel function, and oncological status
Full recovery may take 4-6 weeks, with progressive return to normal activities.
9. How successful is perineal rectal resection?
Success depends on:
-
Extent of disease and tumor stage
-
Completeness of rectal excision
-
Patient adherence to post-operative care
-
For cancer patients, long-term survival and recurrence rates are closely monitored
Most patients experience symptom relief and improved bowel function, with excellent oncologic outcomes when performed in specialized centers.
10. How much does perineal rectal resection cost, and is it covered by insurance?
The cost depends on:
-
Hospital and surgeon fees
-
Anesthesia and operating room charges
-
Post-operative care, imaging, and follow-up
-
Stoma care supplies, if applicable
Perineal rectal resection is medically necessary for rectal cancer or severe disease, and most insurance plans cover the procedure, including hospitalization and follow-up care. Patients should verify coverage, co-pays, and out-of-pocket expenses before surgery.


