Introduction to Peripheral Bypass Surgery
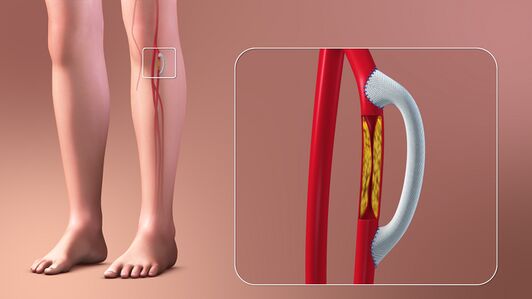
Peripheral bypass surgery, also known as peripheral arterial bypass, is a surgical procedure designed to restore blood flow to the limbs when arteries are blocked or narrowed due to Peripheral Artery Disease (PAD). PAD is primarily caused by atherosclerosis, where fatty plaques accumulate in the arterial walls, restricting blood flow. This can lead to claudication (leg pain during walking), non-healing ulcers, gangrene, and in severe cases, limb loss. When less invasive procedures such as angioplasty or stenting are insufficient or unsuitable—due to long-segment arterial blockages, complex arterial anatomy, or prior failed interventions—peripheral bypass surgery becomes the treatment of choice.
The procedure involves creating an alternate route (bypass) for blood to flow around the blocked artery, using either a patient's own autologous vein (often the saphenous vein) or a synthetic graft (PTFE or Dacron). The bypass can be performed in various locations depending on blockage site: femoropopliteal bypass for thigh arteries, aortobifemoral bypass for aortoiliac disease, or axillofemoral bypass for high-risk abdominal patients. The primary goals of surgery are to relieve pain, heal ulcers, prevent amputation, and improve mobility and quality of life. In modern practice, peripheral bypass surgery is often complemented by minimally invasive endovascular interventions as part of a hybrid approach, ensuring both efficacy and faster recovery.
Causes and Risk Factors of Peripheral Bypass Surgery
Peripheral bypass surgery is performed when blood flow to the legs or arms is critically reduced. The underlying causes generally involve progressive atherosclerosis, leading to arterial stenosis or occlusion.
Major Causes
-
Peripheral Artery Disease (PAD): The most common cause, where plaque buildup narrows or blocks arteries.
-
Diabetes-Associated Arteriopathy: Accelerates PAD, increases small vessel disease, and increases risk of limb ischemia.
-
Previous Vascular Surgery or Failed Endovascular Interventions: Patients may require bypass if stents fail or repeat angioplasty is not feasible.
-
Trauma or Injury: Damage to limb arteries from accidents can necessitate bypass for limb salvage.
-
Chronic Infections or Gangrene: Arterial compromise due to infection or tissue necrosis may require restoration of blood flow.
Risk Factors
-
Lifestyle Factors: Smoking, physical inactivity, poor diet.
-
Medical Conditions: Diabetes, hypertension, high cholesterol, obesity.
-
Age: PAD is more common in older adults.
-
Genetic Factors: Family history of cardiovascular disease increases risk.
-
Other Vascular Conditions: Previous heart attack, stroke, or renal artery disease.
Understanding these risk factors allows clinicians to identify high-risk patients, optimize preoperative management, and predict postoperative outcomes.
Symptoms and Signs Leading to Peripheral Bypass Surgery
Patients with severe PAD requiring bypass often present with a combination of functional, local, and systemic symptoms.
Common Symptoms
-
Intermittent Claudication: Pain, cramping, or fatigue in the calf, thigh, or buttocks triggered by walking or exertion.
-
Rest Pain: Severe pain in the feet or toes while resting, often at night.
-
Non-Healing Ulcers or Wounds: Especially in diabetics, caused by poor blood flow.
-
Coldness or Pallor in Limbs: Indicating reduced arterial circulation.
-
Muscle Weakness or Fatigue: Reduced exercise tolerance and walking distance.
-
Skin Changes: Shiny skin, hair loss, thickened toenails, or skin color changes.
Physical Examination Findings
-
Diminished or absent pulses in the femoral, popliteal, dorsalis pedis, or posterior tibial arteries.
-
Audible bruits over affected arteries.
-
Ulcers, gangrene, or necrotic tissue in severe cases.
-
Temperature differences between limbs, cyanosis, or delayed capillary refill.
Recognizing these symptoms early allows for timely referral to vascular specialists and improves limb salvage outcomes.
Diagnosis and Pre-Surgical Evaluation
A comprehensive preoperative evaluation is crucial for successful peripheral bypass surgery.
Diagnostic Tests
-
Ankle-Brachial Index (ABI): Simple, non-invasive test to assess blood flow.
-
Doppler Ultrasound: Measures blood flow in arteries and detects blockages.
-
CT Angiography or MR Angiography: Provides detailed anatomical mapping of blockages.
-
Digital Subtraction Angiography (DSA): Gold standard for planning surgical bypass.
-
Vein Mapping: For autologous graft planning, typically evaluating the saphenous vein.
Preoperative Assessment
-
Comorbidities: Cardiovascular, renal, and pulmonary status must be evaluated.
-
Laboratory Tests: CBC, renal and liver function, coagulation profile, blood sugar control.
-
Medication Review: Anticoagulants, antiplatelets, or drugs affecting healing.
-
Functional Assessment: Mobility, exercise tolerance, and baseline limb function.
-
Patient Education: Risks of surgery, potential complications, lifestyle modifications, and stoma (if applicable).
Optimizing these factors improves surgical safety, reduces complications, and increases graft longevity.
Treatment Options of Peripheral Bypass Surgery
Peripheral bypass surgery restores blood flow by creating a detour around blocked arteries.
Surgical Approaches
-
Femoropopliteal Bypass: Bypasses blockage between femoral and popliteal arteries.
-
Aortobifemoral Bypass: Treats aortoiliac disease in high-risk patients.
-
Axillofemoral Bypass: Extra-anatomic bypass for patients unsuitable for abdominal surgery.
-
Tibial or Crural Bypass: Restores flow to distal leg or foot in severe ischemia.
Graft Materials
-
Autologous Vein: Saphenous vein preferred for long-term patency.
-
Synthetic Grafts: PTFE or Dacron used when vein unavailable or short segment bypass.
Adjunctive Treatments
-
Endovascular interventions for hybrid procedures.
-
Antiplatelet therapy post-surgery.
-
Rehabilitation programs to improve walking distance and limb function.
The choice of bypass depends on blockage location, graft availability, patient comorbidities, and limb salvage requirements.
Prevention and Management Around Peripheral Bypass Surgery
Effective management includes preventing disease progression and optimizing perioperative outcomes.
Preventive Measures
-
Smoking cessation, exercise programs, and weight management.
-
Control of diabetes, hypertension, and hyperlipidemia.
-
Early treatment of leg wounds to prevent tissue loss.
Perioperative Management
-
Prehabilitation: improve cardiovascular and musculoskeletal fitness.
-
Nutritional optimization and infection control.
-
Wound preparation and graft mapping.
-
Patient counseling regarding post-surgical care and lifestyle changes.
Postoperative Management
-
Pain control, anticoagulation/antiplatelet therapy, wound surveillance.
-
Physical therapy and supervised walking programs.
-
Long-term follow-up: graft monitoring via ultrasound, periodic ABI, and management of risk factors.
Complications of Peripheral Bypass Surgery
Peripheral bypass carries risks that can be categorized as early, intermediate, or late.
Early Complications
-
Surgical site infection or hematoma
-
Graft thrombosis or occlusion
-
Bleeding or wound dehiscence
-
Cardiac or pulmonary complications
Intermediate Complications
-
Graft stenosis requiring revision
-
Pseudoaneurysm at anastomosis site
-
Nerve injury (sensory/motor deficits)
Long-Term Complications
-
Graft failure or occlusion
-
Recurrence of claudication
-
Amputation if tissue necrosis persists
-
Chronic wound or ulceration
-
Reduced limb mobility or persistent pain
Preventive strategies include meticulous surgical technique, careful postoperative monitoring, lifestyle modification, and medication adherence.
Living with the Condition After Peripheral Bypass Surgery
Recovery and adaptation are critical for long-term success:
-
Wound Care and Monitoring: Regular assessment of incision and graft site.
-
Activity and Rehabilitation: Gradual return to walking and exercise; supervised exercise programs to improve circulation.
-
Lifestyle Management: Smoking cessation, diet modifications, diabetic control, weight management.
-
Psychological Support: Coping with chronic disease, fear of limb loss, and maintaining quality of life.
-
Medical Follow-Up: Regular vascular check-ups, graft patency evaluation, and monitoring for new PAD symptoms.
Patients who adhere to lifestyle and medical recommendations often experience pain relief, improved walking distance, ulcer healing, and limb salvage, significantly improving quality of life.
Top 10 Frequently Asked Questions about Peripheral Bypass Surgery
1. What is peripheral bypass surgery?
Peripheral bypass surgery is a vascular procedure that restores blood flow to the limbs by bypassing blocked or narrowed arteries. Surgeons create an alternate pathway using a vein from the patient's body or a synthetic graft, allowing blood to flow around the blockage and reach tissues that were previously deprived of oxygen.
2. Why is peripheral bypass surgery performed?
Peripheral bypass surgery is indicated for patients with:
-
Peripheral artery disease (PAD) causing blocked arteries in the legs or arms
-
Severe leg pain or claudication while walking or at rest
-
Non-healing ulcers or wounds due to poor blood flow
-
Gangrene or risk of limb loss
-
When medications, lifestyle changes, or minimally invasive procedures (like angioplasty) are insufficient to restore adequate circulation
The surgery improves blood supply, relieves pain, and reduces the risk of amputation.
3. Who is a candidate for peripheral bypass surgery?
Candidates include patients with:
-
Significant arterial blockages confirmed via Doppler ultrasound, CT angiography, or MRI angiography
-
Symptoms such as leg pain at rest, tissue loss, or poor wound healing
-
Patients healthy enough to tolerate anesthesia and surgery
-
Individuals who have failed non-surgical treatments
A multidisciplinary evaluation ensures patients are suitable for bypass surgery.
4. How is peripheral bypass surgery performed?
Peripheral bypass surgery is usually done under general or regional anesthesia:
-
Incision: A cut is made near the blocked artery
-
Graft placement: A vein from the patient (usually the saphenous vein) or a synthetic graft is used to bypass the blockage
-
Attachment: The graft is connected above and below the blocked segment to restore blood flow
-
Closure: Incision sites are sutured, and blood flow is tested
The procedure can take 2–4 hours, depending on blockage location and graft type.
5. What are the benefits of peripheral bypass surgery?
-
Restores blood flow to affected limbs
-
Relieves pain and discomfort, including claudication
-
Promotes healing of ulcers, wounds, or gangrene
-
Prevents limb loss in patients with critical ischemia
-
Improves mobility and quality of life
Peripheral bypass is highly effective when non-invasive measures fail, providing long-term relief.
6. Is peripheral bypass surgery painful?
During surgery, anesthesia ensures no pain is felt. Post-operative pain may include:
-
Mild to moderate soreness at incision sites
-
Bruising or swelling along the grafted limb
-
Temporary discomfort while walking or moving the limb
Pain is typically managed with prescription pain medications and gradually decreases over the first 1–2 weeks.
7. What are the risks and complications?
Although generally safe, peripheral bypass surgery carries potential risks:
-
Infection at the incision or graft site
-
Bleeding or hematoma formation
-
Blood clots within the graft
-
Graft failure or narrowing over time
-
Nerve injury causing temporary numbness or weakness
-
Rare complications: heart attack, stroke, or anesthesia-related issues
Close monitoring and post-operative care minimize complications.
8. What is the recovery process after peripheral bypass surgery?
-
Hospital stay: Typically 3–7 days, depending on procedure complexity
-
Activity: Gradual mobilization encouraged; avoid strenuous activity until cleared
-
Wound care: Keep incision clean, dry, and monitor for infection
-
Medications: Blood thinners may be prescribed to prevent clotting
-
Follow-up: Regular imaging and check-ups to monitor graft function
Full recovery may take 4–8 weeks, with gradual improvement in walking ability and limb function.
9. How successful is peripheral bypass surgery?
-
Success rates are high, with most patients experiencing improved blood flow and symptom relief
-
Long-term graft patency depends on graft type, surgical technique, and patient lifestyle
-
Patients who quit smoking, manage diabetes, and maintain healthy cholesterol have better outcomes
-
Repeat procedures are sometimes necessary if graft narrows over time
Most patients regain functional mobility and quality of life post-surgery.
10. How much does peripheral bypass surgery cost, and is it covered by insurance?
Cost depends on:
-
Hospital and surgeon fees
-
Anesthesia and operating room charges
-
Post-operative care, imaging, and medications
Peripheral bypass surgery is medically necessary for PAD or critical limb ischemia, and most insurance plans cover the procedure, including hospitalization and follow-up care. Patients should confirm coverage, co-pays, and out-of-pocket costs with their insurance provider.


