Introduction to Phaco With PMMA IOL
Phaco with PMMA IOL refers to phacoemulsification cataract surgery followed by implantation of a Polymethyl Methacrylate (PMMA) intraocular lens. This procedure is one of the most widely performed surgical interventions in ophthalmology. Cataracts-clouding of the natural crystalline lens-are a leading cause of reversible blindness worldwide. When the cataract progresses to the point where it interferes with daily activities such as reading, driving, recognising faces, or navigating in bright or dim lighting, surgical removal becomes necessary.
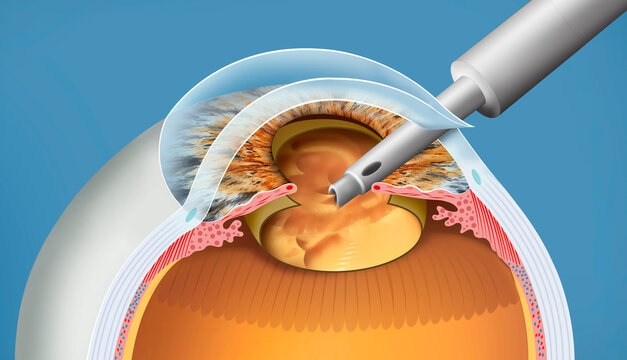
Phacoemulsification is an advanced technique in which a small ultrasonic probe is inserted through a micro-incision to break the cataract into tiny pieces, which are then gently suctioned out. Once the cloudy lens is removed, an artificial lens is implanted to restore clear focusing ability. PMMA lenses were among the earliest lens materials used in cataract surgery and still remain popular in many parts of the world due to their high clarity, long-term stability, low cost, and excellent biocompatibility.
Unlike foldable acrylic or silicone IOLs, PMMA lenses are rigid and therefore require a slightly larger incision for implantation. While this may increase healing time or induce mild astigmatism, PMMA IOLs continue to be highly reliable in resource-constrained settings and in patients who require durable, long-lasting optical clarity. Over decades, research has consistently shown that PMMA lenses can provide excellent visual outcomes with proper surgical technique and postoperative care.
This article explores every aspect of Phaco With PMMA IOL surgery-including causes, symptoms, diagnosis, treatment options, prevention strategies, complication risks, and long-term post-surgery experience.
Causes & Risk Factors Requiring Phaco With PMMA IOL
The main reason a patient undergoes phacoemulsification with PMMA IOL implantation is cataract formation. Cataracts occur when proteins in the natural lens break down and create opacification. Although ageing is the most common cause, several factors contribute to early or accelerated cataract development.
Primary Causes:
-
Age-related degeneration: Most individuals over 60 experience some degree of lens clouding.
-
Genetic predisposition: Family history increases likelihood of early cataract formation.
-
Trauma: Blunt or penetrating injuries to the eye can cause traumatic cataracts.
-
Medical disorders: Diabetes mellitus, hypertension, and metabolic diseases.
-
Medications: Long-term use of corticosteroids (oral, topical, or inhaled).
-
Lifestyle factors: Smoking, excessive alcohol consumption, and prolonged UV exposure.
-
Eye conditions: Chronic uveitis, glaucoma, retinal diseases.
Why PMMA IOL Specifically?
In many healthcare systems, PMMA lenses are chosen because:
-
They are more affordable compared to foldable lenses.
-
They offer durable optics with minimal long-term degradation.
-
They are suitable for larger, stable capsules during standard phaco surgery.
Risk Factors Influencing Surgery:
-
Dense or hyper-mature cataracts requiring higher phaco energy.
-
Small pupils, pseudoexfoliation syndrome, or zonular weakness.
-
Pre-existing corneal diseases increasing risk of postoperative oedema.
-
Patients with diabetes have higher incidence of complications like macular edema.
Understanding these causes and risks helps ophthalmologists plan safer surgical outcomes and counsel patients effectively.
Symptoms & Signs Leading to Phaco With PMMA IOL Surgery
Cataracts progress gradually, and many patients may not initially notice vision changes. However, as clouding intensifies, symptoms often become more significant and affect daily functioning.
Common Symptoms:
-
Persistent blurred or cloudy vision
-
Increased glare sensitivity, especially from oncoming headlights
-
Halos around lights
-
Faded or yellowed colour perception
-
Difficulty reading or recognising faces
-
Poor night vision
-
Frequent changes in glasses prescription
-
Double vision in one eye (monocular diplopia)
Clinical Signs Noted During Examination:
-
Visible lens opacification using slit-lamp microscope
-
Decreased visual acuity (e.g., 6/18 or worse)
-
Reduced contrast sensitivity
-
Small pupil response in advanced cataracts
-
Shallow anterior chamber in some age-related or hyper-mature cataracts
Patients who report difficulty performing routine tasks-such as driving at night, reading fine print, or working in bright sunlight-are ideal candidates for cataract extraction. As symptoms escalate, non-surgical options such as spectacles or magnifiers become insufficient. In such cases, phaco surgery with PMMA IOL implantation offers an effective and permanent vision restoration solution.
Diagnosis of Cataract & Evaluation Before Phaco With PMMA IOL
Diagnosis of a cataract is straightforward, but choosing the ideal surgical approach requires a detailed evaluation. Ophthalmologists perform a comprehensive eye assessment to determine the cataract's maturity, eye health, and suitability for PMMA lens implantation.
Diagnostic Steps:
-
Visual Acuity Test: Measures clarity of vision at distance and near.
-
Slit-lamp Examination: Determines type of cataract (nuclear, cortical, posterior subcapsular).
-
Tonometry: Assesses intraocular pressure, especially important if glaucoma coexists.
-
Dilated Fundus Examination: Evaluates retina and optic nerve health.
-
Refraction Test: Determines refractive error and planning for postoperative vision.
-
Ocular Biometry: Critical test measuring axial length and corneal curvature for IOL power calculation.
-
Corneal Topography: Maps corneal surface, important for astigmatism evaluation.
-
Endothelial Count: Ensures corneal health, especially in dense cataracts requiring higher phaco energy.
Preoperative Planning Includes:
-
Selecting IOL power for best uncorrected vision.
-
Reviewing systemic health, such as diabetes or hypertension.
-
Discussing patient expectations-e.g., need for reading glasses post-surgery.
-
Confirming suitability of PMMA IOL based on incision size and cost considerations.
Proper diagnosis and meticulous preoperative workup significantly improve visual outcomes and reduce postoperative complications.
Treatment Options - Phaco With PMMA IOL and Alternatives
The primary treatment for visually significant cataracts is surgical extraction followed by artificial lens implantation.
Phacoemulsification With PMMA IOL
This is the standard, widely performed technique. Surgery involves:
-
Creating a small incision (larger than foldable IOL surgery due to rigid PMMA lens).
-
Performing capsulorhexis to access the natural lens.
-
Using ultrasonic phaco probe to break and aspirate lens material.
-
Inserting a rigid PMMA intraocular lens into the capsular bag.
-
Closing the wound, sometimes with sutures.
Advantages of PMMA IOL:
-
Cost-effective and highly accessible.
-
Long-term optical clarity.
-
Strong biocompatibility.
Limitations:
-
Larger incision leads to potentially slower recovery.
-
Higher risk of surgically induced astigmatism.
Alternative Treatments
-
Foldable acrylic IOLs (most common in modern cataract surgery)
-
Toric IOLs for astigmatism correction
-
Multifocal IOLs for spectacle-free vision
-
Monofocal IOLs for standard clarity at a single distance
-
Manual Small-Incision Cataract Surgery (MSICS) in very dense cataracts or limited-resource settings
Patients are selected for PMMA lenses based on ocular anatomy, affordability, and surgeon recommendation.
Prevention & Management Strategies
While cataracts cannot always be prevented, several lifestyle and medical measures reduce progression and help manage risks before and after surgery.
Prevention of Cataract Progression:
-
Control diabetes and blood pressure
-
Avoid smoking and excessive alcohol
-
Wear UV-protective sunglasses
-
Avoid prolonged corticosteroid use unless medically necessary
-
Maintain a nutritious diet high in antioxidants (vitamin C, vitamin E, lutein)
Pre-Surgical Risk Management:
-
Optimise blood sugar levels
-
Treat dry-eye or inflammation before surgery
-
Evaluate pupil dilation ability
-
Manage glaucoma to prevent postoperative pressure spikes
Post-Operative Management:
-
Strict use of antibiotic and steroid eye drops
-
Avoid rubbing, heavy lifting, dust exposure
-
Attend scheduled follow-ups at Day 1, Week 1, and Month 1
-
Use protective eye shield at night
Early identification of complications-such as infection, high intraocular pressure, or macular edema-helps preserve long-term visual outcomes.
Complications Associated With Phaco With PMMA IOL
Although considered a safe and highly successful procedure, complications may occasionally occur.
Intraoperative Complications:
-
Posterior capsule rupture
-
Zonular dialysis (weak lens support)
-
Thermal injury to corneal incision
-
Lens fragment drop into the vitreous
Early Postoperative Complications:
-
Infection (endophthalmitis)
-
Corneal edema
-
Raised intraocular pressure
-
Wound leak due to larger incision
-
Inflammation
Late Complications:
-
Posterior Capsule Opacification (PCO): Common with PMMA lenses; treated with YAG laser capsulotomy.
-
IOL decentration or tilt
-
Cystoid macular edema
-
Persistent astigmatism
-
Dry eye symptoms
Most complications are treatable when detected early. Proper surgical technique and adherence to postoperative instructions greatly reduce risks.
Living With the Condition After Phaco With PMMA IOL
After phacoemulsification with PMMA IOL, most patients experience substantial improvement in clarity and quality of life. Visual recovery typically occurs within a few days, although complete healing of the incision may take several weeks.
What Patients Can Expect:
-
Mild discomfort, tearing, or scratchy sensation initially
-
Gradual reduction in glare and halos
-
Significant improvement in brightness and colour perception
-
Possible need for spectacles for reading or distance depending on lens power
Lifestyle Adjustments:
-
Avoid eye makeup for 2 weeks
-
Avoid swimming for at least 3-4 weeks
-
Use sunglasses outdoors to protect from UV light
-
Maintain overall eye health through regular checkups
-
Monitor for symptoms such as sudden vision loss, redness, or severe pain
Long-Term Outcomes:
PMMA intraocular lenses are stable and durable for a lifetime. Patients enjoy restored independence, improved functionality, and enhanced visual comfort. With proper care, annual eye exams, and healthy lifestyle practices, long-term results remain excellent.
Top 10 Frequently Asked Questions about Phaco With PMMA IOL
1. What is Phaco with PMMA IOL?
Phaco with PMMA IOL refers to a cataract removal technique where ultrasound energy (phacoemulsification) is used to break and remove the cloudy natural lens, and a PMMA (Polymethyl Methacrylate) intraocular lens is implanted to restore clear vision. PMMA lenses are rigid and have been used for decades due to their excellent clarity, biocompatibility, and long-term stability. This technique is widely practiced globally and offers dependable visual outcomes. It is especially common in settings where cost-effective solutions are preferred while still ensuring high-quality vision.
2. How is the procedure performed?
Cataract surgery using phacoemulsification is typically performed under local anesthesia with numbing eye drops. The surgeon makes a small corneal incision and inserts a phaco probe, which emits controlled ultrasound energy to emulsify the cataract into microscopic fragments. These fragments are suctioned out through the same probe. After thoroughly cleaning the capsular bag, the surgeon inserts a PMMA intraocular lens. Because PMMA lenses are rigid, they are inserted through a slightly larger incision compared to foldable lenses. Once positioned correctly, the incision may be closed with fine sutures depending on the surgeon's preference. The entire procedure generally lasts 15-20 minutes and is painless for most patients.
3. Why are PMMA lenses still used today?
Despite the availability of newer foldable lenses, PMMA IOLs remain a widely used and trusted choice worldwide. They are extremely durable, offer excellent optical clarity, and have a long track record of safety and predictability. PMMA lenses are also significantly more affordable than premium IOLs, making them ideal for patients seeking a dependable lens without additional cost. In many regions, these lenses are preferred because they are available, reliable, and suitable for a broad range of cataract cases. Their non-foldable design has little impact on long-term vision results.
4. Is Phaco with PMMA IOL safe?
Yes, this surgery is considered safe and is performed millions of times across the world every year. The safety profile of phacoemulsification is well-established. PMMA lenses, too, are known for exceptional biocompatibility, meaning they are well-tolerated by the tissues inside the eye. Like any surgical procedure, there are risks, but they are rare when performed by an experienced surgeon. Potential complications may include infection, swelling, posterior capsular opacification, or mild refractive errors. With proper surgical technique and postoperative care, the risks are minimal and outcomes are highly satisfactory.
5. What are the advantages of PMMA lenses?
PMMA lenses offer numerous benefits, including outstanding optical clarity, long-term lens stability, and resistance to deposits or degradation. These lenses do not change shape, yellow over time, or break, making them extremely reliable for long-term vision. They are also cost-effective, making cataract surgery more accessible to patients from diverse socioeconomic backgrounds. Their biocompatible nature reduces the chance of inflammation or allergic reactions. For healthcare systems performing high volumes of cataract surgeries, PMMA lenses remain a dependable and economical option.
6. Are there disadvantages?
The primary disadvantage of PMMA lenses is that they require a larger incision (usually 5-7 mm), which may result in slightly slower healing compared to surgeries using foldable lenses. The larger incision may also increase the risk of surgically induced astigmatism. Additionally, because PMMA lenses are monofocal, they provide clear vision at only one distance. Patients may still need glasses for reading or intermediate tasks. Despite these limitations, PMMA lenses remain highly effective for restoring clear vision after cataract removal.
7. How long is the recovery period?
Recovery after phaco with PMMA IOL is generally smooth and predictable. Most patients notice improved vision within the first 48 hours. Mild blurriness, glare, or light sensitivity may persist for a few days as the eye heals. Full recovery typically takes 4-6 weeks, during which the incision heals, inflammation subsides, and vision stabilizes. Patients should follow all postoperative instructions closely to ensure optimal results. Regular follow-up visits allow the surgeon to monitor healing and adjust treatment if necessary.
8. What postoperative care is required?
Proper postoperative care is essential for safe and effective healing. Patients are typically prescribed antibiotic and anti-inflammatory eye drops for several weeks. It is important to avoid rubbing the eyes, heavy lifting, strenuous exercise, and exposure to dust or water for at least a week. Protective eyewear may be recommended while sleeping to prevent accidental pressure on the eye. Patients should also avoid swimming pools, eye makeup, and direct sunlight until cleared by their doctor. Following all instructions helps ensure the best visual outcome.
9. Will I still need glasses after surgery?
Most patients with PMMA monofocal lenses will need glasses for reading or detailed close work. Some may also require glasses for distance if mild refractive error remains after healing. This is normal, as PMMA lenses are designed to provide clear vision primarily at one focal distance. If a patient desires spectacle independence, alternative lens types-such as foldable multifocal or toric lenses-may be recommended. However, for standard cataract correction, PMMA lenses provide excellent clarity and value.
10. Who is a good candidate for Phaco with PMMA IOL?
Ideal candidates include patients diagnosed with visually significant cataracts who desire a reliable and cost-effective treatment option. PMMA lenses are suitable for those without corneal abnormalities, severe astigmatism, or complex ocular conditions requiring specialized lenses. They are especially recommended for patients seeking a proven, long-established lens technology. A thorough preoperative evaluation-including eye measurements, ocular health assessment, and vision testing-helps determine if PMMA IOL implantation is the best choice.


