Introduction to Phacoemulsification
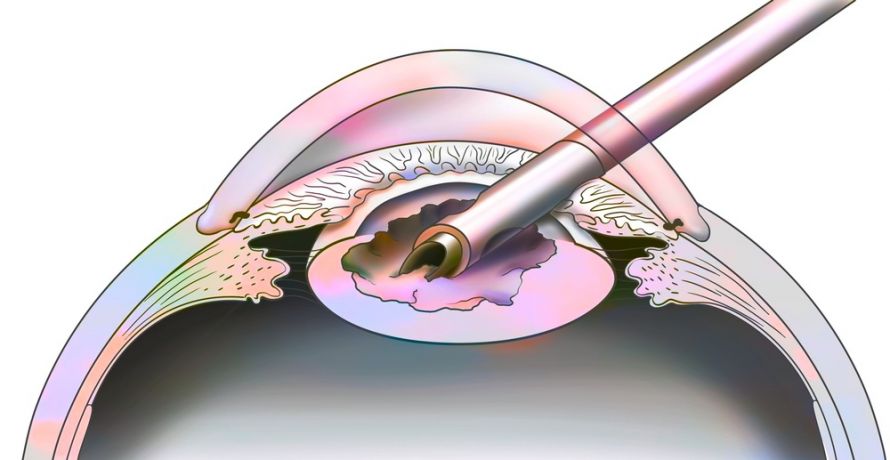
Phacoemulsification is a modern cataract surgery technique that has revolutionized the management of age-related and secondary cataracts. In this procedure, the surgeon uses ultrasonic vibrations to break up the eye's cloudy natural lens (cataract) into tiny fragments, which are then aspirated through a small corneal incision. After removal, the eye's lens is replaced with a foldable intraocular lens (IOL) to restore clear vision.
This technique offers several advantages over traditional extracapsular cataract extraction (ECCE): smaller incision, reduced surgical trauma, faster healing, less induced astigmatism, and minimal postoperative inflammation. Phacoemulsification is now considered the gold standard for cataract surgery worldwide, with millions of procedures performed annually.
The surgery is typically performed under topical or peribulbar anesthesia, which allows the patient to remain comfortable while minimizing systemic risks. The procedure involves a series of carefully coordinated steps: corneal incision, capsulorhexis (opening of anterior lens capsule), hydrodissection, phacoemulsification of the lens nucleus, aspiration of cortical material, and insertion of the IOL. The small incision often self-seals, eliminating the need for sutures. Beyond visual rehabilitation, phacoemulsification significantly improves quality of life, enabling patients to regain independence, reduce fall risk, and resume normal activities.
Causes and Risk Factors of Cataracts Leading to Phacoemulsification
While phacoemulsification is a treatment, it is performed to correct vision impairment caused by cataracts. Cataracts are characterized by opacification of the natural lens, reducing clarity of vision.
Causes
-
Age-Related Changes: Gradual protein aggregation in the lens leading to nuclear sclerosis.
-
Diabetes Mellitus: High glucose levels accelerate lens glycation and opacification.
-
Trauma: Blunt or penetrating eye injuries can lead to post-traumatic cataracts.
-
Medications: Prolonged corticosteroid therapy and certain medications (e.g., amiodarone) increase risk.
-
Congenital Factors: Genetic mutations, metabolic disorders, or developmental anomalies.
-
UV Light Exposure: Chronic sunlight exposure damages lens proteins.
-
Ocular Inflammation: Chronic uveitis or previous ocular surgery can precipitate cataract formation.
Risk Factors
-
Systemic Conditions: Diabetes, hypertension, obesity.
-
Lifestyle: Smoking, excessive alcohol consumption, poor nutrition.
-
Ocular Co-morbidities: Glaucoma, retinal disorders, prior ocular trauma.
-
Surgical Complexity Risks: Dense cataracts, small pupils, zonular weakness, or ocular surface disease increase surgical difficulty.
Recognizing these causes and risk factors helps ophthalmologists determine timing of surgery and optimize outcomes.
Symptoms and Clinical Signs of Cataracts
Cataracts typically progress gradually, and symptoms may be subtle initially. Patients often present with:
Symptoms
-
Blurry Vision: Both near and distant vision gradually worsens.
-
Glare and Halos: Especially at night, affecting driving and outdoor activities.
-
Color Perception Changes: Colors appear faded or yellowed.
-
Monocular Diplopia: Double vision in the affected eye.
-
Reading Difficulty: Near vision tasks become challenging.
-
Frequent Prescription Changes: Rapid changes in glasses or contact lens prescriptions.
Signs
-
Slit-Lamp Examination: Lens opacities such as nuclear sclerosis, cortical spokes, or posterior subcapsular cataracts.
-
Red Reflex Changes: Diminished or uneven red reflex observed during examination.
-
Lens Density Assessment: Determines phacoemulsification energy requirements.
-
Associated Ocular Findings: Presence of glaucoma, retinal degeneration, or corneal pathology may influence surgical planning.
Early recognition of these symptoms allows timely intervention with phacoemulsification before irreversible visual impairment occurs.
Diagnosis and Preoperative Evaluation
Successful phacoemulsification requires careful preoperative assessment:
Ophthalmic Examination
-
Visual Acuity Testing: Distance and near vision.
-
Slit-Lamp Biomicroscopy: Detailed lens evaluation and anterior segment assessment.
-
Fundus Examination: Assessment of retina and optic nerve to anticipate postoperative visual outcomes.
-
Intraocular Pressure Measurement: Screening for glaucoma.
Biometric Evaluation
-
Axial Length Measurement: For accurate IOL power calculation.
-
Keratometry: Measures corneal curvature.
-
Anterior Chamber Depth: Helps select appropriate IOL size.
-
Endothelial Cell Count: Especially in corneal disease or post-surgery eyes.
Systemic and Perioperative Considerations
-
Medical Clearance: Cardiovascular, diabetic, and systemic assessment.
-
Patient Counseling: Discuss realistic expectations, types of IOLs, postoperative care, and potential complications.
-
Preoperative Eye Preparation: Topical antibiotics, pupil dilation, antiseptic cleaning.
Comprehensive evaluation ensures optimal surgical planning and reduced complication risk.
Treatment Options and Surgical Procedure
Phacoemulsification involves removal of the cataractous lens and implantation of an IOL:
Surgical Steps
-
Anesthesia: Topical, peribulbar, or retrobulbar.
-
Micro-Incision: 2-3 mm corneal limbal incision.
-
Capsulorhexis: Creating a circular opening in the anterior lens capsule.
-
Hydrodissection and Hydrodelineation: Separates lens cortex from capsule.
-
Phacoemulsification: Ultrasonic fragmentation of lens nucleus.
-
Cortex Aspiration: Removal of remaining lens material.
-
IOL Implantation: Foldable lens inserted into capsular bag.
-
Incision Closure: Often self-sealing; sutures rarely needed.
Intraocular Lens Options
-
Monofocal IOLs: Correct distance vision; reading glasses often required.
-
Multifocal IOLs: Provide near and distance vision.
-
Toric IOLs: Correct corneal astigmatism.
-
Accommodating IOLs: Move with ciliary body for dynamic focusing.
Advanced Techniques
-
Femtosecond Laser-Assisted Cataract Surgery (FLACS): Improves precision for capsulotomy and lens fragmentation.
-
Manual Small Incision Cataract Surgery (MSICS): Used for dense cataracts or limited-resource settings.
Prevention and Perioperative Management
Prevention and perioperative management for penile lengthening (phalloplasty) address risk reduction, patient safety, and optimized outcomes through multidisciplinary steps before, during, and after surgery.
Preventive Measures
-
UV Protection: Sunglasses to reduce lens damage.
-
Control of Systemic Diseases: Diabetes, hypertension, hyperlipidemia.
-
Lifestyle Modifications: Smoking cessation, balanced diet, antioxidant-rich nutrition.
-
Early Eye Screening: Routine exams for early detection.
Perioperative Care
-
Optimize systemic health and ocular conditions.
-
Preoperative antibiotics to minimize infection risk.
-
Patient education regarding eye protection and activity limitations.
-
Postoperative plan for medications, follow-up visits, and monitoring complications.
Complications of Phacoemulsification
Phacoemulsification, a modern cataract surgery technique, is generally safe but can involve several intraoperative and postoperative complications. While most are rare or manageable with proper technique and follow-up, understanding these helps optimize outcomes and inform patient consent.
Intraoperative
-
Posterior capsule rupture
-
Zonular dehiscence
-
Nucleus fragment drop
-
Iris trauma
Early Postoperative
-
Corneal edema
-
Elevated intraocular pressure
-
Mild anterior chamber inflammation
-
Wound leak or hypotony
Late Complications
-
Posterior capsular opacification (PCO)
-
IOL decentration or dislocation
-
Cystoid macular edema
-
Retinal detachment in predisposed patients
-
Glare or halos with multifocal IOLs
Proper surgical technique, preoperative evaluation, and postoperative follow-up reduce risks.
Living with the Condition After Surgery
After phacoemulsification cataract surgery, most people experience major improvements in vision and daily independence, though full adaptation and the best outcomes depend on individual healing, follow-up, and attention to postoperative care.
Recovery
-
Vision improves within 24-48 hours; full healing in 4-6 weeks.
-
Temporary glare, halos, or mild discomfort are common.
Postoperative Care
-
Eye drops (antibiotics, anti-inflammatories).
-
Avoid rubbing eyes, swimming, and heavy lifting.
-
Regular follow-up to monitor IOL position and healing.
Lifestyle and Long-Term Care
-
UV protection, regular eye exams, and systemic disease management.
-
Awareness of late complications (PCO, retinal changes).
-
Realistic expectations: excellent vision restoration in most patients, with possible need for reading glasses.
Top 10 Frequently Asked Questions about Phacoemulsification
1. What is phacoemulsification and how does it work?
Phacoemulsification is a modern cataract surgery technique where the natural cloudy lens of the eye (cataract) is broken into tiny pieces using ultrasound energy delivered through a small probe. These fragments are suctioned out of the eye, and a foldable intraocular lens (IOL) is inserted to restore clear vision. This technique is highly preferred due to its minimally invasive approach, smaller incision size (2-3 mm), and rapid recovery time, compared to older cataract removal methods like extracapsular or intracapsular cataract extraction. Phacoemulsification preserves eye structure and reduces surgical trauma, allowing patients to regain functional vision much faster.
2. Why is phacoemulsification performed?
Phacoemulsification is indicated when cataracts cause significant visual impairment that affects daily life. Common reasons include:
-
Blurry or cloudy vision making reading, driving, or recognizing faces difficult
-
Glare, halos, or double vision caused by lens opacity
-
Difficulty with night vision
-
Cataract-related complications, such as secondary glaucoma or lens-induced uveitis
-
Lifestyle improvement in patients seeking better visual quality
Early intervention can prevent progressive vision loss and complications, making phacoemulsification a safe and effective solution.
3. Who is an ideal candidate for phacoemulsification?
Candidates are adults or elderly patients with visually significant cataracts. Specifically:
-
Patients with cataract-related visual symptoms interfering with daily life
-
Individuals with healthy cornea and retina for optimal post-surgical outcomes
-
Patients with controlled systemic conditions, such as diabetes or hypertension
-
Individuals who desire rapid recovery and minimal surgical trauma
-
Patients who may not benefit from medication or conservative management, as cataracts cannot be treated with eye drops
Ophthalmologists evaluate visual acuity, cataract severity, ocular health, and systemic conditions before recommending surgery.
4. How is phacoemulsification performed step-by-step?
-
Anesthesia: Usually topical eye drops or local anesthesia; sedation may be added for anxious patients.
-
Incision: A tiny self-sealing incision (2-3 mm) is made at the cornea's edge, eliminating the need for stitches.
-
Capsulorhexis: The surgeon creates an opening in the front of the lens capsule.
-
Phacoemulsification: An ultrasonic probe breaks the cataract into microscopic fragments, which are suctioned out.
-
IOL implantation: A foldable intraocular lens is inserted into the empty lens capsule to restore vision.
-
Closure: The incision is self-sealing; a small shield may be applied for protection.
The procedure is usually completed within 15-30 minutes, and most patients can go home the same day.
5. What are the benefits of phacoemulsification?
-
Minimally invasive, preserving corneal structure and reducing recovery time
-
Rapid visual rehabilitation; many patients notice improvement within 24-48 hours
-
High success rate, with most patients achieving 20/40 vision or better
-
Reduced risk of complications compared to older techniques
-
Versatility with modern IOLs: monofocal, multifocal, toric, or accommodating lenses
-
Improved quality of life, enabling daily activities like driving, reading, and computer work
Overall, phacoemulsification is considered the gold standard for cataract surgery worldwide.
6. Is phacoemulsification painful?
During the surgery:
-
Topical or local anesthesia ensures the patient feels no pain.
-
Mild pressure or vibration may be sensed but is not painful.
After surgery:
-
Mild soreness, burning, or foreign body sensation may occur
-
Temporary tearing or light sensitivity
-
Discomfort is usually managed with over-the-counter analgesics and post-operative eye drops
-
Most patients report minimal pain, with full comfort returning in 1-2 days.
7. What are the risks and potential complications?
Phacoemulsification is highly safe, but potential risks include:
-
Infection (endophthalmitis) - very rare but serious
-
Posterior capsule rupture, which may require additional procedures
-
Corneal edema or swelling, usually transient
-
Retinal detachment or macular edema - rare but possible
-
Dislocation of the IOL
-
Secondary cataract (posterior capsule opacification) may develop months or years later
-
Glaucoma or intraocular pressure changes
Experienced surgeons and modern sterile techniques reduce complication rates significantly, with over 95% of patients experiencing successful outcomes.
8. What is the recovery process after phacoemulsification?
-
Hospital stay: Usually outpatient; patient can go home the same day
-
Eye protection: A small protective shield may be worn for 24-48 hours
-
Medication: Antibiotic and anti-inflammatory eye drops for several weeks
-
Activity: Avoid heavy lifting, swimming, or rubbing the eye for 2-4 weeks
-
Follow-up: Eye examination after 1 day, 1 week, and 4-6 weeks to monitor healing and vision
Most patients experience significant visual improvement within a few days, with full stabilization over 4-6 weeks.
9. How successful is phacoemulsification?
-
Success rate exceeds 95-98% for restoring functional vision
-
Most patients achieve 20/40 vision or better, suitable for driving and daily tasks
-
Visual improvement is usually noticeable immediately, with optimal results over several weeks
-
Complications are rare and generally manageable
-
Outcomes are excellent when combined with modern foldable IOLs, enabling correction of astigmatism or presbyopia
10. How much does phacoemulsification cost, and is it covered by insurance?
Cost depends on:
-
Hospital and surgeon fees
-
Type of intraocular lens (standard monofocal vs. premium multifocal or toric)
-
Anesthesia and operating room charges
-
Post-operative care and follow-up
Phacoemulsification is medically necessary for vision impairment due to cataracts, and most insurance plans cover standard cataract surgery. Premium IOLs or elective enhancements may incur additional out-of-pocket costs. Patients should confirm coverage, co-pays, and potential extra expenses with their insurance provider.


