Introduction to Pharyngoplasty
Pharyngoplasty is a surgical procedure designed to correct structural or functional problems in the pharynx (throat) and soft palate. Its primary aim is to improve speech, breathing, and swallowing, depending on the underlying medical issue. The most common reasons for pharyngoplasty are velopharyngeal insufficiency (VPI), which affects speech, and obstructive sleep apnea (OSA), which affects breathing during sleep.
In VPI, the soft palate fails to close properly against the pharyngeal wall during speech. This incomplete closure allows air to escape through the nose, causing hypernasal speech and articulation difficulties. In adults, pharyngoplasty is often performed to correct airway obstructions caused by a long or floppy soft palate, enlarged tonsils, or excess tissue in the throat that collapses during sleep.
Modern surgical techniques, such as pharyngeal flap surgery, sphincter pharyngoplasty, lateral pharyngoplasty, and barbed pharyngoplasty, allow surgeons to tailor the procedure to the patient's anatomy, resulting in better functional outcomes and faster recovery. Pharyngoplasty can be performed on both children and adults, but the indications vary depending on whether the patient primarily experiences speech or breathing issues. Overall, pharyngoplasty is an important procedure that significantly enhances quality of life for patients by restoring critical speech and airway functions.
Causes and Risk Factors of Pharyngoplasty
Pharyngoplasty is not a disease but a surgical solution to correct underlying problems. Understanding the causes helps identify who might need this procedure.
Causes in Children (Speech-Related)
-
Cleft Palate: Even after surgical repair, children may develop incomplete closure of the velopharyngeal valve, leading to persistent speech problems.
-
Congenital Syndromes: Syndromes such as velocardiofacial syndrome, Down syndrome, or other craniofacial anomalies can result in weak or misaligned soft palate muscles.
-
Neuromuscular Disorders: Conditions such as cerebral palsy can weaken the muscles of the soft palate, leading to VPI.
-
Previous Surgeries: Tonsillectomy, adenoidectomy, or other throat surgeries may alter the anatomy of the soft palate and pharynx, resulting in poor closure during speech.
Causes in Adults (Airway-Related)
-
Obstructive Sleep Apnea (OSA): Collapse of the upper airway during sleep, often due to thickened pharyngeal tissues, enlarged tonsils, or a long/floppy soft palate.
-
Anatomical Predisposition: Some adults naturally have narrow airways or redundant tissue in the throat.
-
Lifestyle Factors: Obesity, smoking, and aging can worsen airway obstruction.
-
History of Radiation Therapy: Radiation to the head and neck can cause tissue changes that affect airway function.
Risk Factors
-
Age: Young children and older adults may face higher surgical risks.
-
Comorbidities: Heart disease, obesity, or uncontrolled diabetes can complicate surgery.
-
Anatomical Variations: Scar tissue, previous surgery, or abnormal growth patterns.
-
Severity of Underlying Condition: More severe VPI or OSA increases the complexity of surgery.
Symptoms and Signs Acupressure Treats
Symptoms of conditions requiring pharyngoplasty vary depending on whether the issue is speech-related or airway-related.
Speech-Related Symptoms
-
Hypernasal Speech: Excessive nasal resonance during speaking.
-
Nasal Air Escape: Air leaks through the nose while pronouncing consonants like "p," "b," "t," or "d."
-
Poor Articulation: Difficulty producing certain sounds, reducing speech intelligibility.
-
Speech Fatigue: Speaking for a long time may worsen hypernasality.
Airway-Related Symptoms
-
Loud Snoring: Persistent and disruptive during sleep.
-
Sleep Apnea Signs: Observed pauses in breathing, gasping, or choking during sleep.
-
Daytime Fatigue: Excessive sleepiness, difficulty concentrating, and irritability.
-
Headaches and Poor Sleep Quality: Waking unrefreshed in the morning.
Other Signs
-
Difficulty Swallowing: Dysphagia, especially postoperatively or with severe VPI.
-
Nasal Regurgitation: Food or liquid passing into the nose during swallowing.
-
Throat Discomfort: Foreign-body sensation or chronic sore throat.
-
Mouth Breathing: Especially during sleep or after previous throat surgery.
Diagnosis of Pharyngoplasty-Indicative Conditions
Accurate diagnosis is essential for planning the surgical procedure.
Speech Evaluation
-
Conducted by a speech-language pathologist (SLP).
-
Includes perceptual assessment of resonance and articulation.
-
Objective tools like nasometry measure nasal airflow and acoustic energy during speech.
Dynamic Visualization
-
Nasoendoscopy: A flexible endoscope examines the movement of the soft palate and pharyngeal walls during speech.
-
Videofluoroscopy: X-ray imaging captures dynamic closure of the velopharyngeal valve during speech.
Airway Assessment
-
Polysomnography (Sleep Study): Measures apnea-hypopnea events, oxygen levels, and sleep quality in OSA patients.
-
Drug-Induced Sleep Endoscopy (DISE): Identifies the site of airway collapse for precise surgical planning.
Imaging
-
CT or MRI: Evaluate structural anatomy of the soft palate, pharynx, and lateral walls.
Preoperative Evaluation
-
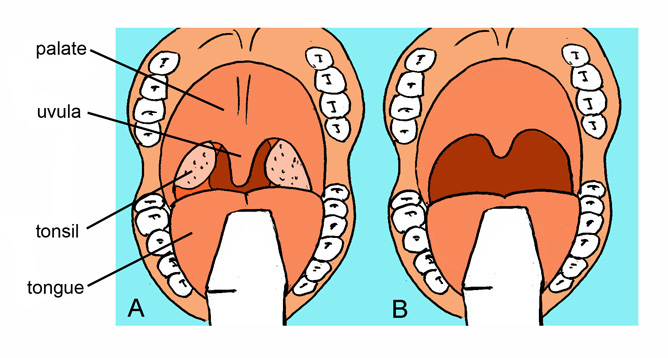
Physical examination by an ENT surgeon, including tonsil size, uvula length, and lateral wall anatomy.
-
Medical assessment to check comorbidities and anesthesia risk.
Treatment Options for Pharyngoplasty
Treatment may involve non-surgical and surgical approaches, depending on severity and type of disorder.
Non-Surgical Approaches
-
Speech Therapy: First-line for mild VPI; helps strengthen palatal muscles and improve articulation.
-
Lifestyle Changes for OSA: Weight management, positional therapy, nasal treatments, and CPAP machines.
Surgical Options
-
Pharyngeal Flap Surgery: A tissue flap from the back of the throat is attached to the soft palate, closing the velopharyngeal gap while maintaining lateral airflow.
-
Sphincter Pharyngoplasty: Tissue flaps are repositioned to form a circular sphincter around the velopharyngeal port, improving closure during speech.
-
Lateral Pharyngoplasty: Primarily for OSA; enlarges and stabilizes the airway by repositioning lateral pharyngeal tissues.
-
Barbed Pharyngoplasty: Minimally invasive; barbed sutures reposition soft tissues with less trauma and faster recovery.
-
Augmentation Pharyngoplasty: Adds tissue to the posterior pharyngeal wall to improve closure.
-
Robotic-Assisted Pharyngoplasty: Advanced precision for reshaping lateral walls and soft palate in airway cases.
Adjunctive Procedures
-
Tonsillectomy, uvula reduction, or tongue base surgery may be combined to optimize outcomes for OSA or severe VPI.
Prevention and Management of Pharyngoplasty
Prevention
-
Early speech therapy for children at risk of VPI.
-
Prompt evaluation and management of airway obstruction in adults.
-
Maintaining healthy weight and good sleep hygiene to prevent worsening of OSA.
Management
-
Postoperative Speech Therapy: Essential for optimizing articulation and resonance.
-
Airway Monitoring: OSA patients may require follow-up sleep studies to ensure airway stability.
-
Lifestyle Measures: Weight control, smoking cessation, managing allergies, and sleep hygiene.
-
Long-Term Follow-Up: Especially important in children for craniofacial growth and speech development.
Complications of Pharyngoplasty
Pharyngoplasty is generally safe but may have complications.
Immediate Risks
-
Pain, swelling, or mild bleeding.
-
Difficulty swallowing or throat discomfort.
-
Temporary changes in voice quality.
Long-Term Complications
-
Persistent or recurrent VPI.
-
Overcorrection or undercorrection causing hyponasality or hypernasality.
-
Airway obstruction or residual OSA.
-
Suture-related discomfort in barbed techniques.
-
Impact on craniofacial growth in children (rare).
-
Need for revision surgery.
Living with the Condition of Pharyngoplasty
Postoperative Recovery
-
Hospital stay for monitoring in airway cases.
-
Soft diet and careful wound care.
-
Gradual return to normal activities.
Speech and Airway Outcomes
-
Improved speech clarity and intelligibility in children with VPI.
-
Better sleep quality, reduced snoring, and improved oxygenation in adults with OSA.
Quality of Life
-
Enhanced social interactions, confidence, and communication.
-
Reduced daytime fatigue and improved productivity.
Long-Term Follow-Up
-
Regular speech and airway assessment.
-
Monitoring for growth and possible revision surgery.
-
Adaptation to changes in throat sensation or airflow.
Top 10 Frequently Asked Questions about Pharyngoplasty
1. What is Pharyngoplasty?
Pharyngoplasty is a surgical procedure performed to correct abnormalities or dysfunctions in the pharynx (throat). It is most commonly used to treat velopharyngeal insufficiency (VPI), a condition where the soft palate does not close properly against the back of the throat during speech. This results in nasal-sounding voice, speech difficulty, and air leakage. Pharyngoplasty works by modifying or reconstructing the tissues in the throat to improve closure of the velopharyngeal sphincter. It may involve repositioning muscles, tightening tissues, or creating tissue flaps. The procedure helps improve speech quality, reduce nasal air escape, and enhance swallowing function in certain cases.
2. Who needs a pharyngoplasty?
Patients who have VPI due to congenital conditions like cleft palate, submucous cleft palate, or neuromuscular disorders are common candidates. It is also performed in individuals with persistent speech disorders despite previous palate surgeries or intensive speech therapy. Children who develop hypernasal speech after adenoid removal may require pharyngoplasty if the problem does not resolve. Some adults may need the surgery due to trauma, tumors, or neurological conditions affecting throat muscles. A thorough evaluation by a speech-language pathologist, ENT surgeon, and plastic surgeon helps determine eligibility.
3. How is the pharyngoplasty procedure performed?
The surgery is conducted under general anesthesia. The exact technique depends on the patient's anatomy and severity of VPI. Common techniques include sphincter pharyngoplasty, pharyngeal flap surgery, and Furlow palatoplasty. In sphincter pharyngoplasty, tissue flaps from the sides of the throat are rotated to form a smaller opening, improving velopharyngeal closure. In pharyngeal flap surgery, tissue from the back wall of the throat is attached to the soft palate. The goal is to direct airflow properly for normal speech. The surgery typically takes 1-2 hours.
4. What conditions can pharyngoplasty treat?
Pharyngoplasty is primarily used for:
-
Velopharyngeal insufficiency (VPI)
-
Hypernasal speech
-
Cleft palate-related speech disorders
-
Speech problems after adenoidectomy
-
Structural throat abnormalities
-
Neuromuscular dysfunction affecting swallowing or speech
By improving closure between the soft palate and throat, the procedure enhances speech resonance, reduces nasal escape, and supports proper swallowing mechanics in some patients.
5. What is the recovery period like after pharyngoplasty?
Most patients stay in the hospital for 1-2 days post-surgery. A sore throat, mild swelling, and difficulty swallowing are normal for the first week. Soft foods and plenty of fluids are recommended. Full recovery may take 2-6 weeks. The surgical site gradually heals, swelling decreases, and speech starts improving as tissues settle. Follow-up appointments ensure proper healing and evaluate speech progress. Many patients resume normal activities within two weeks, depending on comfort and surgeon's advice.
6. Are there risks or complications associated with pharyngoplasty?
Like any surgical procedure, pharyngoplasty carries some risks. Possible complications include bleeding, infection, pain, snoring, airway obstruction, or sleep apnea due to reduced airway space. In some cases, the procedure may not fully correct VPI, requiring adjustments or additional treatment. Children may temporarily develop nasal congestion or changes in speech patterns during healing. Complications are rare when the surgery is performed by experienced specialists and when postoperative instructions are followed carefully.
7. Will speech improve after pharyngoplasty?
Yes, the primary goal of pharyngoplasty is to improve speech. Most patients experience significant reduction in hypernasality, better speech clarity, and improved resonance. However, surgery is not always an instant cure. Patients typically require ongoing speech therapy to retrain muscles, correct articulation, and optimize speech quality. Combining surgery with professional speech therapy results in the best long-term outcomes.
8. How should a patient prepare for pharyngoplasty?
Preparation includes a complete evaluation by an ENT surgeon, plastic surgeon, and speech-language pathologist. Imaging tests such as nasoendoscopy or videofluoroscopy are often used to assess velopharyngeal movement. Patients may need pre-surgical speech therapy to build strength and awareness. Fasting guidelines must be followed before anesthesia. Parents should explain the procedure to children in a reassuring manner. The surgeon will discuss risks, expectations, and postoperative care to ensure a smooth recovery.
9. What postoperative care is required after pharyngoplasty?
Patients should consume soft foods, avoid strenuous activity, and stay hydrated. Pain medications and antibiotics may be prescribed. Good oral hygiene is essential to prevent infection. Children should avoid yelling, crying excessively, or forceful blowing of the nose for several weeks. Follow-up visits monitor healing, speech changes, and airway function. Speech therapy typically resumes once healing is sufficient. Caregivers should watch for breathing difficulties, unusual swelling, or persistent pain and report concerns promptly.
10. Is pharyngoplasty a permanent solution?
For many patients, pharyngoplasty provides long-lasting improvement in speech and velopharyngeal function. Once the tissues heal and adapt, results are generally stable. However, continued speech therapy is often necessary to maximize outcomes. In some cases—especially in growing children or those with neurological conditions—additional surgeries or adjustments might be required over time. Most individuals experience significant, lifelong improvements in communication and quality of life.


