Introduction to Pneumatic Retinopexy
Pneumatic retinopexy is a minimally invasive ophthalmic procedure designed to repair certain types of retinal detachments, particularly those involving retinal tears or breaks in the upper (superior) portion of the retina. The retina is a thin, light-sensitive layer at the back of the eye that plays a critical role in visual function by transmitting visual signals to the brain. When a retinal break occurs, the fluid inside the eye can leak underneath the retina, causing it to separate from its underlying tissues. This condition, known as retinal detachment, is a medical emergency that threatens permanent vision loss if untreated.
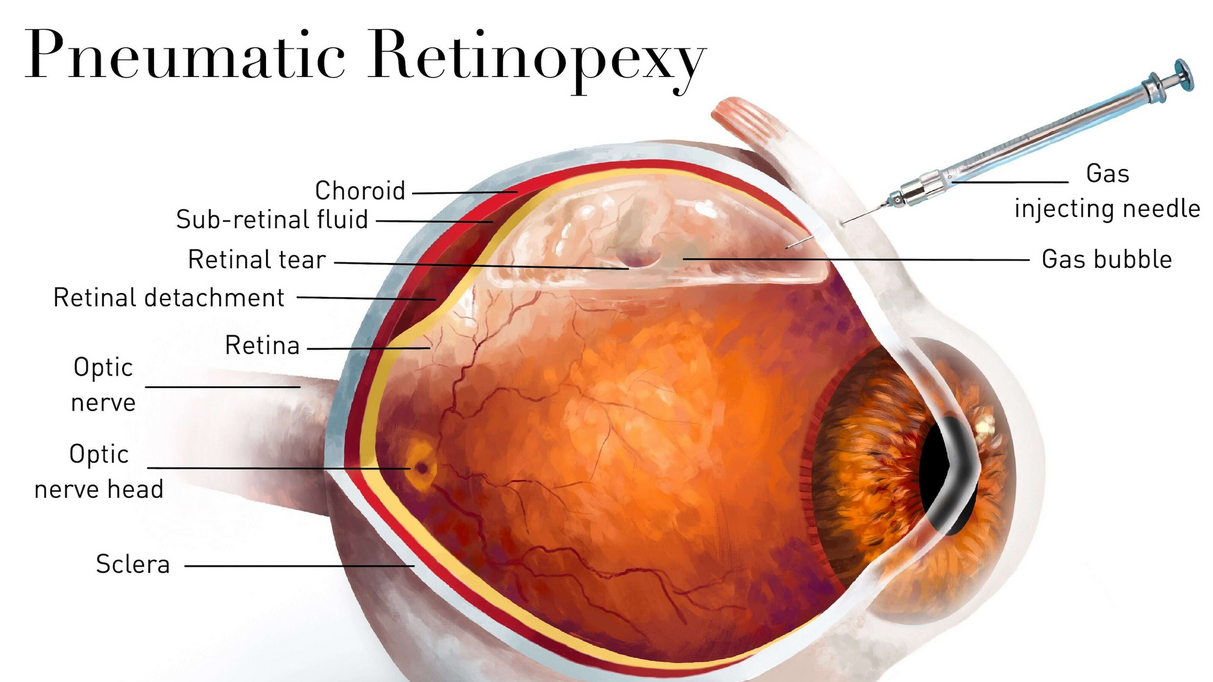
Developed in the 1980s, pneumatic retinopexy offers a less invasive alternative to more extensive surgeries like scleral buckling or vitrectomy. This outpatient procedure involves injecting a gas bubble into the vitreous cavity of the eye. The bubble rises and presses against the retinal tear, helping it seal and allowing the retina to reattach. To permanently secure the retina, cryotherapy or laser photocoagulation is used around the tear.
Pneumatic retinopexy is highly effective for selected patients and is associated with faster recovery, less discomfort, and lower cost than traditional surgical methods. Its success depends heavily on proper patient selection, tear location, adherence to postoperative positioning, and timely intervention.
Causes and Risks Associated with Pneumatic Retinopexy
Pneumatic retinopexy is used to treat specific types of retinal detachments. Understanding why detachments occur helps explain the rationale for this procedure and the need for early detection.
A. Causes of Retinal Detachment Requiring Pneumatic Retinopexy
1. Posterior Vitreous Detachment (PVD)
As people age, the vitreous gel inside the eye shrinks and pulls away from the retina. In some cases, it can create traction on the retina, causing a tear that leads to detachment.
2. Retinal Tears or Breaks
Small tears allow fluid to accumulate underneath the retina. These may result from:
-
Aging-related changes
-
Trauma
-
Severe myopia (nearsightedness)
-
Eye surgeries
-
Genetic predisposition
3. Trauma to the Eye
Blunt or penetrating injuries can lead to sudden retinal tears and subsequent detachment.
4. Lattice Degeneration
A thinning of the peripheral retina that makes it susceptible to tears.
5. Inflammatory or Other Eye Conditions
Long-standing inflammation, infections, or tumors may weaken the retinal structure.
B. Risk Factors for Retinal Detachment
-
High myopia (more than -6.00 diopters)
-
Family history of detachment
-
Previous eye surgeries (cataract extraction)
-
Eye trauma or sports injuries
-
Diabetes with retinopathy
-
Aging (more common in individuals over 50)
-
Previous retinal tears
-
Long-standing vitreous degeneration
Patients with these risk factors should be monitored closely, as early diagnosis improves the success rate of pneumatic retinopexy.
Symptoms and Signs of Retinal Detachment (Indication for PneumaticRetinopexy)
Symptoms of retinal detachment appear suddenly and should never be ignored. Pneumatic retinopexy is typically performed when these symptoms are promptly recognized.
Common Symptoms Include:
1. Sudden Appearance of Floaters
Small black spots, cobweb-like strands, or specks moving across the visual field.
2. Flashes of Light (Photopsia)
Caused by vitreous traction on the retina.
3. Shadow or Curtain Over Vision
Often begins at the peripheral vision and progresses inward.
4. Blurred or Distorted Vision
Vision becomes hazy or unclear as the retina detaches.
5. Reduced Peripheral Vision
Loss of side vision is an early warning sign.
6. Sudden Vision Loss
Occurs if the macula (central retina) detaches.
Emergency Warning Signs
-
Rapid expansion of floaters
-
Curtain-like shadow
-
Pain when associated with trauma
Immediate intervention is crucial. Pneumatic retinopexy is most effective when performed before the macula fully detaches.
Diagnosis of Retinal Detachment for Pneumatic Retinopexy
Accurate diagnosis is essential to determine whether pneumatic retinopexy is appropriate.
Diagnostic Steps Include:
1. Detailed Medical and Ocular History
The ophthalmologist reviews:
-
Symptom onset
-
Trauma history
-
Previous eye surgeries
-
Family history
-
Existing eye disorders
2. Dilated Fundus Examination
A comprehensive exam using specialized instruments to:
-
Locate the retinal tear
-
Assess the extent of detachment
-
Identify whether superior breaks are present
This is the most important step in determining eligibility for the procedure.
3. Indirect Ophthalmoscopy
Provides a wide-field view of the retina and helps assess fluid accumulation.
4. Optical Coherence Tomography (OCT)
Used to evaluate macular involvement and confirm retinal elevation.
5. B-Scan Ultrasonography
Performed when the retina isn’t visible due to media opacities such as:
-
Dense cataracts
-
Vitreous hemorrhage
6. Assessment of Tear Location
Pneumatic retinopexy is most effective when the tear is:
-
Single or limited in number
-
Small or moderate in size
-
Located in the upper two-thirds of the retina
Treatment Options - Pneumatic Retinopexy Procedure
Pneumatic retinopexy offers a minimally invasive approach to retinal detachment repair.
A. Who Is a Suitable Candidate?
Ideal for:
-
Single retinal break
-
Small cluster of breaks within 1 clock hour
-
Superior retinal tears
-
Patients able to maintain strict postoperative positioning
Not suitable for:
-
Large or multiple tears
-
Inferior retinal detachments
-
Severe proliferative vitreoretinopathy (PVR)
-
Long-standing detachments
-
Patients unable to follow postoperative instructions
B. Step-by-Step Procedure
1. Local Anesthesia
Numbing eye drops or injections ensure a painless experience.
2. Cryotherapy or Laser Photocoagulation
The retinal tear is sealed using:
-
Cryopexy (freezing)
-
Argon laser
This prevents further fluid leakage.
3. Gas Bubble Injection
A sterile gas bubble (usually SF6 or C3F8) is injected into the vitreous cavity.
The gas bubble:
-
Rises to the retinal tear
-
Creates pressure against the tear
-
Allows the retina to flatten and reattach
4. Post-Procedure Eye Positioning
The patient must maintain a strict head position for several days to keep the bubble over the tear.
5. Recovery Period
As the retina reattaches, the gas bubble slowly absorbs over 1-8 weeks depending on the gas used.
C. Effectiveness of Pneumatic Retinopexy
Success rate:
-
70-90% initial reattachment
-
Higher success when combined with early treatment and correct selection
If pneumatic retinopexy fails, a secondary procedure like vitrectomy or scleral buckle may be required.
Prevention and Management of Retinal Detachment (Before and After Pneumatic Retinopexy)
While retinal detachment cannot always be prevented, certain practices may reduce risk.
A. Prevention Before Detachment
-
Regular eye exams, especially for high-risk individuals
-
Use of protective eyewear during sports or hazardous work
-
Avoiding physical strain after eye surgeries
-
Managing chronic conditions such as diabetes
-
Prompt attention to symptoms like floaters and flashes
B. Postoperative Management After Pneumatic Retinopexy
1. Adherence to Positioning
Regular eye exams, especially for high-risk individuals
Use of protective eyewear during sports or hazardous work
Avoiding physical strain after eye surgeries
Managing chronic conditions such as diabetes
Prompt attention to symptoms like floaters and flashes
1. Adherence to Positioning
Correct head positioning is the most critical factor for successful healing.
2. Medications
The ophthalmologist may prescribe:
-
Antibiotic drops
-
Anti-inflammatory drops
-
Pain relievers
3. Regular Follow-up Visits
To monitor:
-
Retina reattachment progress
-
Gas bubble size
-
Any new retinal tears
4. Avoidance of Certain Activities
-
Air travel strictly prohibited until the bubble disappears
-
Avoid altitude changes
-
No heavy lifting
-
Avoid sleeping on your back depending on tear location
5. Vision Monitoring
As the bubble dissolves, vision gradually improves.
Complications of Pneumatic Retinopexy
While the procedure is generally safe, certain complications may occur.
A. Common, Temporary Side Effects
-
Mild pain or discomfort
-
Blurred vision
-
Light sensitivity
-
Elevated intraocular pressure
-
Temporary double vision
B. Potential Serious Complications
-
New retinal tears
-
Re-detachment
-
Gas bubble migration
-
Infection (endophthalmitis)
-
Cataract formation
-
Proliferative vitreoretinopathy (PVR)
-
Failure requiring scleral buckling or vitrectomy
C. Risk Mitigation
Choosing an experienced retina specialist and following aftercare instructions significantly reduces risks.
Living with the Condition After Pneumatic Retinopexy
Retinal detachment and its treatment impact everyday life. Patients often require psychological and lifestyle adjustments.
A. Recovery and Vision Rehabilitation
-
Vision improves gradually over weeks
-
Depth perception may be temporarily affected
-
Glasses or updated prescriptions may be required after healing
B. Lifestyle Adjustments
-
Avoid high-impact sports until cleared
-
Maintain regular follow-up with the retina specialist
-
Protect eyes from injury
-
Monitor for new symptoms (flashes, floaters, shadows)
C. Long-Term Outlook
Most patients regain substantial vision if the macula was not detached before treatment. Early intervention significantly improves visual outcomes.
D. Emotional and Psychological Support
Being diagnosed with retinal detachment is stressful. Support through patient education, counselling, and follow-up reassurance helps individuals cope with the anxiety of potential recurrence.
Top 10 Frequently Asked Questions about Pneumatic Retinopexy
1. What is Pneumatic Retinopexy and why is it performed?
Pneumatic retinopexy is a minimally invasive procedure used to repair certain types of retinal detachment, a serious condition where the retina separates from the underlying tissue. The procedure involves injecting a small gas bubble into the eye’s vitreous cavity. This bubble then rises and presses the retina back into position, allowing the tear or hole to be sealed using laser photocoagulation or cryotherapy. It is performed primarily to prevent permanent vision loss, restore the structural integrity of the retina, and avoid more invasive surgeries like scleral buckling or vitrectomy when possible.
2. Who is an ideal candidate for Pneumatic Retinopexy?
Ideal candidates typically include patients with:
-
A single retinal tear or a group of small tears located in the upper part of the retina
-
Fresh retinal detachment with minimal fluid accumulation
-
No significant scarring or proliferative vitreoretinopathy
-
Ability to maintain necessary head positioning after the procedure
It is not suitable for large, complex, or long-standing retinal detachments. A retina specialist determines eligibility after a thorough eye examination.
3. How is Pneumatic Retinopexy performed?
The procedure is usually performed in the doctor's office under local anesthesia. Steps include:
-
Numbing the eye with anesthetic drops.
-
Injecting a sterile gas bubble (typically C3F8 or SF6) into the vitreous cavity.
-
Applying laser or cryotherapy to seal the retinal tear.
-
Instructing the patient to maintain specific head positioning so the bubble floats against the retinal tear to close it.
The entire procedure generally takes 15-30 minutes and is less invasive than traditional retinal surgery.
4. Is Pneumatic Retinopexy painful?
Most patients experience little to no pain because the eye is numbed with anesthetic drops or a local injection. Some may feel mild pressure or discomfort during the gas injection. After the procedure, temporary scratchiness, tearing, or mild soreness may occur, which usually resolves in a day or two with prescribed medications.
5. What is the success rate of Pneumatic Retinopexy?
Pneumatic retinopexy has a success rate of 70-90% for suitable candidates. Success depends on factors such as:
-
Location and number of retinal tears
-
Patient compliance with head positioning
-
Presence of scar tissue
-
Time between detachment and treatment
In cases where the first attempt is unsuccessful, additional procedures like vitrectomy or scleral buckling may be required.
6. What are the risks or complications associated with Pneumatic Retinopexy?
Though generally safe, potential risks include:
-
Recurrence of retinal detachment
-
New retinal tears forming
-
Elevated intraocular pressure
-
Cataract progression
-
Infection (rare)
-
Inflammation or discomfort
-
Gas bubble-related vision obstruction
Most complications are manageable with timely treatment and follow-up.
7. How long does recovery take after Pneumatic Retinopexy?
Recovery varies, but most patients experience improvement within 1-2 weeks, while full healing may take 4-6 weeks. You may notice:
-
Blurred vision while the gas bubble remains in the eye
-
Gradual clearing of vision as the bubble shrinks
Follow-up visits are crucial to ensure the retina remains attached and to monitor eye pressure.
8. What activity restrictions should I follow after Pneumatic Retinopexy?
Patients must follow strict aftercare guidelines, including:
-
Maintaining proper head positioning for several days to allow bubble contact with the tear
-
Avoiding air travel or high-altitude places until the gas bubble is fully absorbed
-
Avoiding strenuous exercise, heavy lifting, or bending over
-
Protecting the eye from trauma
-
Using only prescribed eyedrops
Failure to follow post-procedure instructions may affect the success of the treatment.
9. Will I be able to see normally with the gas bubble in my eye?
Vision will be blurred initially because the bubble blocks part of your field of vision. As the bubble gradually absorbs over days or weeks, your sight will slowly improve. Patients often describe seeing a line or edge where the bubble meets the natural fluid in the eye. Normal vision typically returns once the bubble disappears completely.
10. Can Pneumatic Retinopexy prevent future retinal problems?
While pneumatic retinopexy effectively repairs the current detachment, it does not prevent new retinal tears or detachments from occurring later. Patients with retinal problems should maintain regular eye checkups, manage risk factors (such as high myopia), and seek immediate care if they notice new floaters, flashes of light, or shadow-like vision changes. Early detection is key to preventing future complications.


