Introduction to Pterygium Excision & Conjunctival-Limbal Allograft
Pterygium is a common ocular surface disorder characterized by a triangular fibrovascular growth of the conjunctiva that extends onto the cornea, typically from the nasal side. This growth can lead to chronic irritation, redness, tearing, visual disturbances, and cosmetic concerns, particularly when it encroaches upon the central cornea and induces astigmatism. Pterygia are more prevalent in sunny, tropical, and arid regions, highlighting the role of environmental exposure in their development.
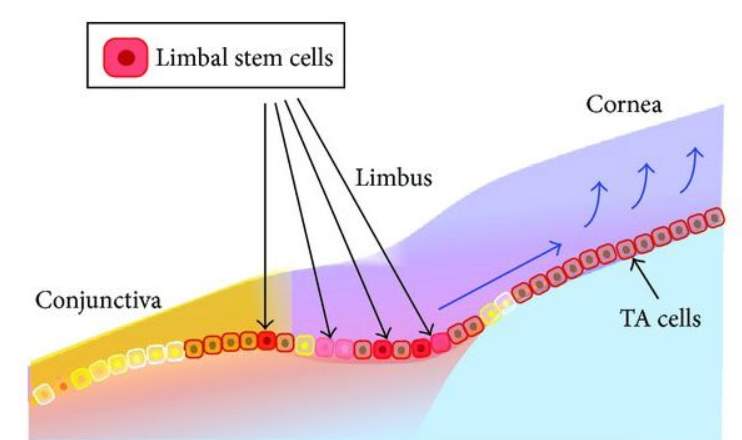
Surgical excision is indicated for pterygia that threaten vision, cause persistent symptoms, or recur after prior interventions. Traditional bare-sclera excision often results in high recurrence rates, leading modern ophthalmic surgeons to adopt conjunctival-limbal autografts or allografts. These grafts restore the limbal barrier, which is critical for maintaining corneal epithelial integrity, preventing fibrovascular proliferation, and reducing recurrence.
The procedure involves carefully excising the pterygium, harvesting healthy conjunctival-limbal tissue (usually from the superior bulbar conjunctiva), and transplanting it onto the scleral defect created by excision. Fixation can be achieved using sutures or fibrin glue, with adjunctive agents like mitomycin-C in selected cases to further lower recurrence rates.
Modern pterygium excision with conjunctival-limbal grafting provides superior visual, cosmetic, and functional outcomes. This guide delves into the causes, risk factors, symptoms, diagnosis, treatment options, prevention, complications, and post-surgical life associated with this procedure.
Causes and Risk of Pterygium Excision & Conjunctival-Limbal Allograft
Pterygium excision with conjunctival-limbal allograft is done to remove a wing-shaped growth on the eye and restore a healthy limbal barrier, but like any surgery it has specific triggers (causes for needing surgery) and risks (complications).
A. Etiology of Pterygium
The development of a pterygium is multifactorial, influenced by environmental, genetic, and ocular surface factors:
-
Ultraviolet (UV) Radiation: Chronic exposure damages limbal stem cells and conjunctival stroma, causing elastotic degeneration and fibrovascular proliferation.
-
Environmental Irritants: Wind, dust, and sand can trigger chronic ocular irritation, leading to fibrovascular growth.
-
Geography and Climate: Individuals living near the equator or in sunny, arid climates have higher incidence rates.
-
Age: Cumulative UV exposure increases risk in older adults.
-
Genetic Predisposition: Certain genetic markers may make individuals more susceptible to pterygium formation.
B. Risk Factors for Needing Surgical Excision
-
Visual Axis Involvement: Pterygia that threaten central vision or induce astigmatism require excision.
-
Recurrent Pterygia: Previously excised pterygia that recur pose a higher risk for complications.
-
Chronic Ocular Surface Disease: Dry eye or limbal stem cell deficiency increases graft failure and recurrence risk.
-
Size and Morphology: Larger, fleshy pterygia have a higher likelihood of recurrence and may require grafting for optimal outcomes.
C. Surgical Risk Factors
-
Incomplete removal of Tenon's tissue can increase recurrence.
-
Improper graft fixation or small graft size can compromise healing.
-
Inflammation or ocular surface disorders may reduce graft success.
Understanding these factors is essential for surgical planning, patient counselling, and long-term follow-up.
Symptoms and Signs of Pterygium
Pterygium often causes few symptoms at first, but as it grows it can lead to noticeable eye changes and, in some cases, vision problems. Recognising typical signs early helps decide when simple eye drops are enough and when surgery should be considered.
A. Patient Symptoms
Patients with pterygium may present with:
-
Redness and Irritation: Persistent conjunctival hyperemia due to fibrovascular proliferation.
-
Foreign Body Sensation: Caused by corneal surface irregularity.
-
Tearing or Photophobia: Chronic ocular surface disruption leads to epiphora and light sensitivity.
-
Blurred Vision: Occurs when the pterygium encroaches on the visual axis or induces astigmatism.
-
Cosmetic Concerns: Visible growth on the cornea can affect self-esteem.
B. Clinical Signs
-
Triangular Fibrovascular Growth: Extending onto the cornea, usually nasal side.
-
Stocker's Line: Iron deposition at the leading edge of the pterygium.
-
Corneal Changes: Flattening or induced astigmatism detectable via corneal topography.
-
Recurrent Lesions: Evidence of previous surgery, scarring, or residual fibrovascular tissue.
Early recognition of these symptoms and signs is critical for timely surgical intervention and preventing visual impairment.
Diagnosis of Pterygium Excision & Conjunctival-Limbal Allograft
Diagnosis here has two parts: confirming that the lesion is a pterygium and then deciding whether it needs excision with a conjunctival-limbal (allo/autograft) based on its effect on the eye. The graft procedure itself is not “diagnosed” but chosen when certain clinical criteria are met.
A. Clinical Examination
-
Slit-Lamp Evaluation: Assess size, thickness, vascularity, and corneal involvement.
-
Documentation: Photographs for surgical planning and postoperative comparison.
B. Ancillary Investigations
-
Corneal Topography: Quantifies astigmatism induced by the pterygium.
-
Anterior Segment Optical Coherence Tomography (OCT): Evaluates depth of invasion and tissue thickness.
-
Tear Film Assessment: Ensures ocular surface health prior to grafting.
C. Preoperative Planning
-
Determine graft size and donor site (usually superior bulbar conjunctiva).
-
Assess ocular surface for dry eye, inflammation, or blepharitis.
-
Plan for adjunctive therapy such as mitomycin-C or amniotic membrane if risk factors for recurrence exist.
-
Educate patients about surgical procedure, recovery, potential risks, and outcomes.
Treatment Options of Pterygium Excision & Conjunctival-Limbal Allograft
Treatment for pterygium ranges from simple eye drops to surgery, with excision plus conjunctival-limbal graft used when the lesion is large, symptomatic, or at high risk of recurrence. The aim is to control irritation, protect vision, and minimise the chance that the pterygium grows back.
A. Surgical Procedure
-
Excision of Pterygium: Complete removal of the head, body, and Tenon's layer.
-
Conjunctival-Limbal Graft Harvesting: Typically from the superior bulbar conjunctiva, including limbal stem cells.
-
Graft Placement: Secured over the scleral defect with sutures or fibrin glue.
-
Adjunctive Therapy: Low-dose mitomycin-C in recurrent or high-risk cases; amniotic membrane for large defects.
B. Variations
-
Autograft: Patient's own conjunctival-limbal tissue (preferred).
-
Allograft: Donor tissue in cases of bilateral disease or insufficient autograft tissue.
-
Fibrin Glue vs Sutures: Glue reduces operative time and discomfort; sutures are traditional but may cause mild irritation.
C. Postoperative Care
-
Topical antibiotics and corticosteroids to reduce infection and inflammation.
-
Lubricating eye drops to maintain ocular surface health.
-
UV protection to prevent recurrence.
-
Follow-up visits to monitor graft integration and early signs of recurrence.
Outcomes: Recurrence rates with conjunctival-limbal autograft are typically <5%, significantly lower than bare-sclera excision.
Prevention and Management of Pterygium Excision & Conjunctival Limbal Allograft
Prevention and management around pterygium excision with conjunctival-limbal graft focus on two things: reducing the chance of needing surgery in the first place, and, if surgery is done, minimising recurrence and complications. Conjunctival-limbal autograft/allograft techniques are among the most effective ways to keep recurrence rates low, especially in high-UV environments.
A. Prevention of Pterygium Formation
-
UV Protection: Sunglasses with side shields, wide-brimmed hats.
-
Avoid Ocular Irritants: Minimize exposure to dust, sand, wind.
-
Manage Ocular Surface Health: Treat dry eye, blepharitis, and inflammation.
-
Regular Eye Examinations: Especially in high-risk populations (outdoor workers, equatorial regions).
B. Preoperative Management
-
Treat any ocular surface inflammation prior to surgery.
-
Counsel patients on postoperative care and recurrence risk.
C. Postoperative Management
-
Strict UV protection.
-
Use of lubricants and anti-inflammatory drops.
-
Avoid eye rubbing or exposure to irritants.
-
Schedule regular follow-up to detect early recurrence.
-
Consider adjunctive therapy in high-risk cases.
Complications of Pterygium Excision & Conjunctival-Limbal Allograft
Pterygium excision with conjunctival-limbal autograft/allograft is generally safe and designed to minimise recurrence, but it can still cause short- and long-term complications. Most are mild and manageable; serious problems are rare when surgery is done carefully and follow-up is good.
A. Common Complications
-
Mild discomfort and redness.
-
Subconjunctival hemorrhage.
-
Temporary tearing or photophobia.
B. Serious Complications
-
Graft dislocation or dehiscence.
-
Recurrence: Higher risk in younger patients, recurrent pterygium, or large lesions.
-
Scleral thinning or melting, especially with mitomycin-C misuse.
-
Dellen formation: Corneal thinning adjacent to graft.
-
Induced astigmatism or persistent corneal irregularity.
C. Management
-
Close postoperative monitoring and revision surgery if graft fails.
-
Treat ocular surface disorders to support graft survival.
-
Educate patients on signs of recurrence or graft complications.
Living with the Condition After Surgery
Living well after surgery means protecting your healing body while gradually rebuilding normal routines, mood, and independence based on your surgeon’s specific advice. Most people can return to a satisfying daily life by following medical instructions closely, pacing activities, and addressing both physical and emotional recovery.
A. Recovery
-
Mild discomfort for several days post-surgery.
-
Vision typically improves as graft integrates.
-
Avoid eye rubbing, dusty environments, or strenuous activity initially.
B. Lifestyle Adjustments
-
Lifelong UV protection.
-
Use lubricating drops as needed.
-
Avoid chronic ocular surface irritants.
-
Attend regular follow-ups for monitoring.
C. Long-Term Outcomes
-
Improved comfort, vision, and cosmetic appearance.
-
Recurrence is rare with proper grafting and postoperative care.
D. Psychosocial Considerations
-
Cosmetic improvement increases confidence.
-
Education reduces anxiety about recurrence and ensures proper care.
Summary: Proper surgical technique, adjunctive therapy, and post-operative care allow patients to live comfortably and maintain vision, with minimal risk of recurrence or long-term complications.
Top 10 Frequently Asked Questions about Pterygium Excision & Conjunctival Limbal Allograft
1. What is a pterygium and why does it need to be removed?
A pterygium is a wedge-shaped growth of fibrovascular tissue that originates on the conjunctiva and extends onto the cornea. It is strongly associated with chronic UV exposure, dry environments, irritants like dust and wind, and long-term inflammation. While it is benign, it can progressively grow across the cornea, causing visual distortion, astigmatism, persistent redness, cosmetic issues, and eventually vision loss. Pterygium excision becomes necessary when symptoms interfere with daily life, vision is affected, or the growth is aggressive or cosmetically disturbing. Early treatment prevents scarring and long-term complications.
2. What is Conjunctival Limbal Allograft (CLA)?
Conjunctival Limbal Allograft is an advanced surgical technique used after pterygium removal. It involves transplanting conjunctival and limbal stem-cell-rich tissue from a donor source—often a cadaver, living relative, or sometimes the patient's other eye. The presence of limbal stem cells is crucial because they serve as a natural barrier against abnormal tissue regrowth. CLA significantly reduces the high recurrence rate seen in older pterygium excision methods and restores the normal ocular surface, offering enhanced long-term stability.
3. How is the pterygium excision with CLA performed?
The surgery begins with local anesthesia. The surgeon removes the pterygium from both the corneal surface and underlying tissues. After complete removal, the donor conjunctival-limbal graft is carefully shaped and placed over the exposed scleral area. It is secured using sutures or fibrin glue. The graft integrates with the patient's eye tissue over time and provides a source of healthy epithelial cells. The entire procedure typically takes 30-60 minutes and is performed as an outpatient surgery.
4. Why choose CLA over traditional bare-sclera excision?
Traditional bare-sclera excision left the underlying tissue exposed, causing recurrence rates of up to 80%. CLA offers significant advantages:
-
Extremely low recurrence rates
-
Restoration of limbal stem cells
-
Faster healing and improved surface stability
-
Better cosmetic appearance
-
Reduced inflammation and scarring
Because pterygium can be aggressive in certain individuals, CLA is considered one of the most effective and reliable modern techniques.
5. Who is an ideal candidate for CLA?
CLA is recommended for:
-
Patients with recurrent or large pterygium
-
Those with chronic inflammation or rapid regrowth
-
Individuals with limbal stem cell deficiency
-
Patients exposed to high UV or dusty environments
-
People requiring optimal cosmetic results
Your ophthalmologist will assess corneal involvement, recurrence history, and overall eye health to determine suitability.
6. What is the recovery process like?
Most patients recover within 2-6 weeks. Mild irritation, tearing, foreign-body sensation, and redness are expected initially. Medications including antibiotics and steroid drops help prevent infection and reduce inflammation. Vision may be slightly blurry but improves as healing progresses. Patients must avoid rubbing the eyes, swimming, dusty environments, and direct sunlight during the early healing period. The graft gradually integrates into the eye and becomes indistinguishable from natural tissue.
7. What risks and complications may occur?
Complications are rare but may include graft displacement, infection, excessive scarring, persistent redness, or delayed healing. Recurrence is still possible but significantly less likely with CLA. In rare cases, mild astigmatism or discomfort may persist. Choosing an experienced surgeon and following postoperative instructions greatly minimizes risks.
8. How long does the graft last?
The graft becomes a permanent part of the eye as it integrates naturally into the conjunctiva and limbal area. Once it has healed completely, it continues to provide lifelong protection by maintaining the integrity of the corneal surface and reducing the risk of future pterygium formation.
9. Will the pterygium return after CLA?
CLA has one of the lowest recurrence rates among current surgical options. While no procedure guarantees 100% prevention, recurrence is significantly minimized due to the presence of limbal stem cells in the graft. Adopting preventive measures—such as wearing UV-protective eyewear, using lubricating drops, and avoiding environmental irritants—further decreases the likelihood of regrowth.
10. What long-term care is recommended after the procedure?
Long-term care includes regular ophthalmic checkups, consistent use of UV-blocking sunglasses, and maintaining good ocular lubrication. Patients working outdoors should take extra precautions to avoid chronic irritation. Your doctor may recommend periodic use of anti-inflammatory drops if you have dry eyes or environmental exposure. Proper follow-up ensures excellent cosmetic and functional results for years.


