Introduction to Radial Optic Neurotomy
Radial Optic Neurotomy (RON) is a specialized retinal surgery that was developed in the late 1990s to treat severe forms of central retinal vein occlusion (CRVO), a sight-threatening condition where the main vein draining blood from the retina becomes blocked. In CRVO, blood and fluid accumulate inside the eye, leading to swelling of the macula (the central area of vision), retinal hemorrhages, and progressive vision loss. RON is performed inside the eye, usually as part of a pars plana vitrectomy. Using a very fine micro-vitreoretinal (MVR) blade, the surgeon makes a small radial cut at the margin of the optic disc to open the tight bony and fibrous canal through which the central retinal vein passes. The theoretical goal is to “decompress” the vein, improve blood outflow, and reduce edema and ischemia in the retina. Early case series reported promising improvements in visual acuity and retinal perfusion in many patients with severe hemorrhagic CRVO.
However, subsequent controlled trials and long-term experience showed mixed results and highlighted important potential complications. At the same time, intravitreal anti-VEGF injections (such as ranibizumab, aflibercept, bevacizumab and faricimab) emerged as the evidence-based standard of care for macular edema due to CRVO. As a result, RON is now considered an adjunct or investigational procedure and is not widely used as first-line treatment. Still, it remains of interest in selected, severe, or refractory cases and is important to understand as part of the full spectrum of CRVO management.
Causes and Risk of Radial Optic Neurotomy
It is important to emphasize that Radial Optic Neurotomy is not a disease; it is a surgical response to an underlying eye condition, most commonly central retinal vein occlusion. Therefore, when we talk about “causes and risks related to RON,” we are mainly referring to:
-
Causes of the underlying condition (CRVO)
-
Reasons why RON might be considered
-
Risks associated with the surgery itself
1. Underlying causes and risk factors for CRVO
CRVO typically occurs in older adults and is strongly associated with systemic
vascular risk factors. The main contributors include:
-
Ageing - risk rises significantly after age 50.
-
Hypertension and arteriosclerosis - stiff, thickened
arteries can compress the adjacent retinal vein at the optic nerve,
predisposing to clot formation.
-
Diabetes mellitus - damages blood vessel walls and
promotes microvascular occlusion.
-
High cholesterol and dyslipidemia - accelerate vascular
damage and thrombosis.
-
Glaucoma or increased intraocular pressure - may
mechanically compress veins at the optic disc.
-
Smoking - increases blood viscosity and vascular disease
risk.
-
Hypercoagulable states (e.g., certain clotting
disorders, oral contraceptive use in high-risk individuals) - increase
the tendency of blood to clot.
These factors create a “bottleneck” at the optic nerve head, where the central
retinal vein passes through a rigid scleral canal and lamina cribrosa. RON is
designed to mechanically enlarge this confined space and relieve the presumed
“compartment syndrome.”
2. Why RON might be considered
RON is generally not the first treatment offered. Anti-VEGF
injections, steroids, and laser therapy are preferred because they have stronger
clinical evidence and fewer severe anatomical risks.
RON may be considered in:
-
Severe, non-ischemic or ischemic CRVO with very poor visual
acuity and extensive hemorrhage not responding to
intravitreal therapy
-
Cases where macular edema remains refractory despite intensive anti-VEGF
or steroid treatment
-
Selected patients enrolled in clinical trials or managed by
subspecialists with experience in complex retinal surgery
3. Surgical risks specific to RON
Like any intraocular surgery, RON carries inherent risks. Documented and
theoretical complications include:
-
Damage to the central retinal artery or vein leading to
sudden, profound vision loss
-
Retinal or optic nerve hemorrhage
-
Retinal detachment or iatrogenic retinal tears
-
Choroidal or chorioretinal neovascularization
originating from the incision site
-
Permanent visual field defects related to damage of
nerve fiber bundles at the optic disc
Because of these potential complications and the success of non-surgical
treatments, most guidelines classify RON as a high-risk,
limited-indication procedure.
Ageing - risk rises significantly after age 50.
Hypertension and arteriosclerosis - stiff, thickened arteries can compress the adjacent retinal vein at the optic nerve, predisposing to clot formation.
Diabetes mellitus - damages blood vessel walls and promotes microvascular occlusion.
High cholesterol and dyslipidemia - accelerate vascular damage and thrombosis.
Glaucoma or increased intraocular pressure - may mechanically compress veins at the optic disc.
Smoking - increases blood viscosity and vascular disease risk.
Hypercoagulable states (e.g., certain clotting disorders, oral contraceptive use in high-risk individuals) - increase the tendency of blood to clot.
RON is generally not the first treatment offered. Anti-VEGF injections, steroids, and laser therapy are preferred because they have stronger clinical evidence and fewer severe anatomical risks. RON may be considered in:
-
Severe, non-ischemic or ischemic CRVO with very poor visual acuity and extensive hemorrhage not responding to intravitreal therapy
-
Cases where macular edema remains refractory despite intensive anti-VEGF or steroid treatment
-
Selected patients enrolled in clinical trials or managed by subspecialists with experience in complex retinal surgery
3. Surgical risks specific to RON
Like any intraocular surgery, RON carries inherent risks. Documented and
theoretical complications include:
-
Damage to the central retinal artery or vein leading to
sudden, profound vision loss
-
Retinal or optic nerve hemorrhage
-
Retinal detachment or iatrogenic retinal tears
-
Choroidal or chorioretinal neovascularization
originating from the incision site
-
Permanent visual field defects related to damage of
nerve fiber bundles at the optic disc
Because of these potential complications and the success of non-surgical
treatments, most guidelines classify RON as a high-risk,
limited-indication procedure.
Damage to the central retinal artery or vein leading to sudden, profound vision loss
Retinal or optic nerve hemorrhage
Retinal detachment or iatrogenic retinal tears
Choroidal or chorioretinal neovascularization originating from the incision site
Permanent visual field defects related to damage of nerve fiber bundles at the optic disc
Symptoms and Signs of Radial Optic Neurotomy-Related Conditions
The symptoms that bring a patient to medical attention are those of central retinal vein occlusion, not of the surgery itself. Many patients only hear about RON later when treatment options are discussed.
Typical symptoms of CRVO (before any surgery)
Patients usually report:
-
Sudden, painless blurring or dimming of vision in one
eye
-
Distortion of central vision (metamorphopsia)
-
Difficulty reading, recognizing faces, or seeing fine detail
-
In some cases, patchy or sectoral visual loss,
especially with hemicentral retinal vein occlusion
-
Rarely, redness or mild eye discomfort, but significant pain is unusual
unless neovascular glaucoma develops
Clinical signs on examination
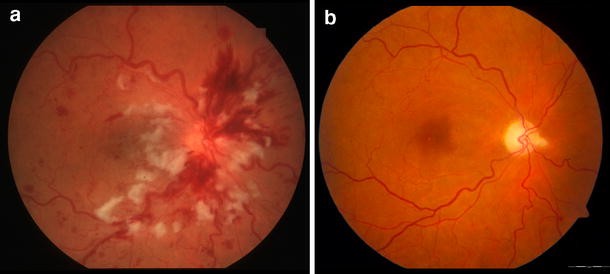
On dilated fundus examination, an ophthalmologist may see:
-
Diffuse retinal hemorrhages (“blood and thunder”
appearance)
-
Dilated, tortuous retinal veins
-
Cotton wool spots indicating retinal ischemia
-
Macular edema causing loss of central retinal reflex
-
Optic disc swelling and hyperemia
These features are well-described in standard ophthalmic references and
reflect impaired venous outflow and capillary leakage.
Symptoms and signs after RON
After RON, the following may be observed:
-
Postoperative blurring or temporary reduction in vision
immediately after surgery (often expected)
-
A visible radial incision at the nasal margin of the optic
disc on fundus exam
-
In some cases, gradual improvement in visual acuity and
reduction of macular edema over months, especially in selected series
where RON was combined with vitrectomy.
-
In case of complications, new visual field defects,
persistent or increased hemorrhage, or signs of retinal or choroidal
neovascularization.
Any sudden worsening of vision, pain, or increased redness after surgery needs
urgent ophthalmic review.
Sudden, painless blurring or dimming of vision in one eye
Distortion of central vision (metamorphopsia)
Difficulty reading, recognizing faces, or seeing fine detail
In some cases, patchy or sectoral visual loss, especially with hemicentral retinal vein occlusion
Rarely, redness or mild eye discomfort, but significant pain is unusual unless neovascular glaucoma develops
On dilated fundus examination, an ophthalmologist may see:
-
Diffuse retinal hemorrhages (“blood and thunder” appearance)
-
Dilated, tortuous retinal veins
-
Cotton wool spots indicating retinal ischemia
-
Macular edema causing loss of central retinal reflex
-
Optic disc swelling and hyperemia
These features are well-described in standard ophthalmic references and reflect impaired venous outflow and capillary leakage.
Symptoms and signs after RON
After RON, the following may be observed:
-
Postoperative blurring or temporary reduction in vision
immediately after surgery (often expected)
-
A visible radial incision at the nasal margin of the optic
disc on fundus exam
-
In some cases, gradual improvement in visual acuity and
reduction of macular edema over months, especially in selected series
where RON was combined with vitrectomy.
-
In case of complications, new visual field defects,
persistent or increased hemorrhage, or signs of retinal or choroidal
neovascularization.
Any sudden worsening of vision, pain, or increased redness after surgery needs
urgent ophthalmic review.
Postoperative blurring or temporary reduction in vision immediately after surgery (often expected)
A visible radial incision at the nasal margin of the optic disc on fundus exam
In some cases, gradual improvement in visual acuity and reduction of macular edema over months, especially in selected series where RON was combined with vitrectomy.
In case of complications, new visual field defects, persistent or increased hemorrhage, or signs of retinal or choroidal neovascularization.
Diagnosis of Radial Optic Neurotomy-Related Condition
Again, RON is a treatment, so diagnosing the “condition” is primarily about correctly identifying CRVO or hemicentral RVO and assessing whether a patient might benefit from RON or alternative therapies.
1. Comprehensive eye examination
The diagnostic process typically includes:
-
Detailed medical and ocular history, including vascular
risk factors, medications, glaucoma, and previous ocular surgery
-
Measurement of visual acuity and refraction
-
Intraocular pressure assessment to rule out glaucoma or
ocular hypertension
-
Slit-lamp exam of the anterior segment and lens
-
Dilated fundus examination to assess the retina, macula,
optic nerve, and peripheral retina
2. Imaging for CRVO
Key tests include:
-
Optical Coherence Tomography (OCT)
-
Measures macular thickness and detects intraretinal or subretinal
fluid
-
Helps monitor response to anti-VEGF injections or surgery
-
Fluorescein Angiography (FA)
-
Visualizes retinal circulation, areas of non-perfusion, and
leakage
-
Helps distinguish ischemic vs non-ischemic CRVO, which influences
prognosis and treatment choices
-
OCT-Angiography (OCT-A) (where available)
-
Non-invasive mapping of macular and peripapillary
microvasculature
-
May document changes after interventions, including RON
3. Systemic evaluation
Because CRVO is strongly linked with systemic disease, many patients undergo:
-
Blood pressure checks and cardiovascular review
-
Laboratory tests for diabetes, lipid profile, and
sometimes hypercoagulability screening (especially in younger patients)
-
Assessment for sleep apnea, smoking status, obesity, and
other vascular risk factors
4. Pre-operative assessment for RON
Before recommending RON, a retinal surgeon will:
-
Confirm the diagnosis, severity, and type of vein occlusion
-
Evaluate whether there is persistent macular edema or
severe ischemia despite optimal intravitreal therapy
-
Explain alternative options and their evidence base
-
Obtain imaging documenting the optic nerve anatomy and the expected
incision site
-
Discuss potential risks, benefits, and the limited role of RON in current
practice
Detailed medical and ocular history, including vascular risk factors, medications, glaucoma, and previous ocular surgery
Measurement of visual acuity and refraction
Intraocular pressure assessment to rule out glaucoma or ocular hypertension
Slit-lamp exam of the anterior segment and lens
Dilated fundus examination to assess the retina, macula, optic nerve, and peripheral retina
Key tests include:
-
Optical Coherence Tomography (OCT)
-
Measures macular thickness and detects intraretinal or subretinal fluid
-
Helps monitor response to anti-VEGF injections or surgery
-
-
Fluorescein Angiography (FA)
-
Visualizes retinal circulation, areas of non-perfusion, and leakage
-
Helps distinguish ischemic vs non-ischemic CRVO, which influences prognosis and treatment choices
-
-
OCT-Angiography (OCT-A) (where available)
-
Non-invasive mapping of macular and peripapillary microvasculature
-
May document changes after interventions, including RON
-
3. Systemic evaluation
Because CRVO is strongly linked with systemic disease, many patients undergo:
-
Blood pressure checks and cardiovascular review
-
Laboratory tests for diabetes, lipid profile, and
sometimes hypercoagulability screening (especially in younger patients)
-
Assessment for sleep apnea, smoking status, obesity, and
other vascular risk factors
4. Pre-operative assessment for RON
Before recommending RON, a retinal surgeon will:
-
Confirm the diagnosis, severity, and type of vein occlusion
-
Evaluate whether there is persistent macular edema or
severe ischemia despite optimal intravitreal therapy
-
Explain alternative options and their evidence base
-
Obtain imaging documenting the optic nerve anatomy and the expected
incision site
-
Discuss potential risks, benefits, and the limited role of RON in current
practice
Blood pressure checks and cardiovascular review
Laboratory tests for diabetes, lipid profile, and sometimes hypercoagulability screening (especially in younger patients)
Assessment for sleep apnea, smoking status, obesity, and other vascular risk factors
Before recommending RON, a retinal surgeon will:
-
Confirm the diagnosis, severity, and type of vein occlusion
-
Evaluate whether there is persistent macular edema or severe ischemia despite optimal intravitreal therapy
-
Explain alternative options and their evidence base
-
Obtain imaging documenting the optic nerve anatomy and the expected incision site
-
Discuss potential risks, benefits, and the limited role of RON in current practice
Treatment Options of Radial Optic Neurotomy
When discussing treatment, we need to place RON within the full treatment landscape for CRVO.
1. Standard treatments for CRVO
Modern management is built around:
-
Intravitreal anti-VEGF injections
-
Medications such as ranibizumab, aflibercept, bevacizumab, and
faricimab block vascular endothelial growth factor (VEGF),
reducing vascular leakage and macular edema.
-
Large randomized trials (e.g., BRAVO, CRUISE, and others) have
shown significant gains in visual acuity and macular thickness
with monthly or treat-and-extend regimens.
-
Current guidelines recommend anti-VEGF as the first-line
treatment for macular edema due to CRVO.
-
Intravitreal corticosteroids
-
Options include dexamethasone implants and
intravitreal triamcinolone.
-
Particularly useful in patients who respond poorly to anti-VEGF
or who cannot attend frequent visits, but they carry a higher
risk of cataract and elevated intraocular pressure.
-
Laser photocoagulation
-
Panretinal photocoagulation is used primarily to manage or
prevent neovascularization of the iris, angle,
or retina, which can lead to neovascular glaucoma.
-
Systemic risk factor control
-
Tight control of blood pressure, sugar, lipids, and stopping
smoking are crucial to reduce further vascular events and
protect the fellow eye.
2. Where Radial Optic Neurotomy fits in
Surgical rationale:
RON aims to relieve the presumed mechanical compression of the central retinal
vein within the rigid scleral canal and lamina cribrosa. During pars plana
vitrectomy, the surgeon places an MVR blade at the nasal edge of the optic disc
and makes one or (rarely) two radial incisions directed away from the fovea,
incising the lamina cribrosa and adjacent sclera.
Evidence profile:
-
Early small case series reported high rates (70-90%) of visual
improvement by at least 2 lines on the Snellen chart and rapid
resolution of hemorrhages and edema.
-
Subsequent studies, including prospective series and meta-analyses,
showed more variable results, with some benefit in
visual acuity and macular thickness but also significant risk of
complications.
-
A 2016 meta-analysis suggested that RON might improve vision and reduce
neovascular glaucoma rates compared with some other treatments, but
heterogeneity and limited sample sizes make firm conclusions difficult,
and results have not surpassed those of anti-VEGF therapy.
Current status:
Most contemporary ophthalmology references and guidelines consider RON to be:
-
Experimental or adjunctive, not routine first-line care
-
Potentially useful in very selected cases of severe CRVO
where intravitreal therapy alone has failed
-
A procedure that should be performed only by experienced vitreoretinal
surgeons, ideally in a clinical study or after exhaustive discussion of
alternatives and risks
Intravitreal anti-VEGF injections
-
Medications such as ranibizumab, aflibercept, bevacizumab, and faricimab block vascular endothelial growth factor (VEGF), reducing vascular leakage and macular edema.
-
Large randomized trials (e.g., BRAVO, CRUISE, and others) have shown significant gains in visual acuity and macular thickness with monthly or treat-and-extend regimens.
-
Current guidelines recommend anti-VEGF as the first-line treatment for macular edema due to CRVO.
Intravitreal corticosteroids
-
Options include dexamethasone implants and intravitreal triamcinolone.
-
Particularly useful in patients who respond poorly to anti-VEGF or who cannot attend frequent visits, but they carry a higher risk of cataract and elevated intraocular pressure.
Laser photocoagulation
-
Panretinal photocoagulation is used primarily to manage or prevent neovascularization of the iris, angle, or retina, which can lead to neovascular glaucoma.
Systemic risk factor control
-
Tight control of blood pressure, sugar, lipids, and stopping smoking are crucial to reduce further vascular events and protect the fellow eye.
Surgical rationale:
RON aims to relieve the presumed mechanical compression of the central retinal
vein within the rigid scleral canal and lamina cribrosa. During pars plana
vitrectomy, the surgeon places an MVR blade at the nasal edge of the optic disc
and makes one or (rarely) two radial incisions directed away from the fovea,
incising the lamina cribrosa and adjacent sclera.
Evidence profile:
-
Early small case series reported high rates (70-90%) of visual improvement by at least 2 lines on the Snellen chart and rapid resolution of hemorrhages and edema.
-
Subsequent studies, including prospective series and meta-analyses, showed more variable results, with some benefit in visual acuity and macular thickness but also significant risk of complications.
-
A 2016 meta-analysis suggested that RON might improve vision and reduce neovascular glaucoma rates compared with some other treatments, but heterogeneity and limited sample sizes make firm conclusions difficult, and results have not surpassed those of anti-VEGF therapy.
Current status:
Most contemporary ophthalmology references and guidelines consider RON to be:
-
Experimental or adjunctive, not routine first-line care
-
Potentially useful in very selected cases of severe CRVO where intravitreal therapy alone has failed
-
A procedure that should be performed only by experienced vitreoretinal surgeons, ideally in a clinical study or after exhaustive discussion of alternatives and risks
Prevention and Management of Radial Optic Neurotomy-Related Condition
Since RON is a treatment, prevention strategies largely focus on preventing CRVO or reducing the chance that it becomes so severe that aggressive surgery is considered.
1. Preventing or reducing the risk of CRVO
Lifestyle and medical measures include:
-
Blood pressure control: Regular screening and treatment
of hypertension.
-
Diabetes management: Good glycemic control and routine
ophthalmic exams for diabetic patients.
-
Lipid management: Diet, exercise, and medication when
needed to manage cholesterol.
-
Smoking cessation: One of the most effective ways to
reduce vascular risk.
-
Managing glaucoma: Regular eye pressure checks and
adherence to glaucoma medications if prescribed.
-
Regular eye exams in at-risk individuals: Older adults
and those with cardiovascular disease should have periodic dilated
retinal examinations.
2. Early management of CRVO
Early recognition and treatment can reduce the chance of irreversible vision loss
and the need for radical surgery:
-
Prompt ophthalmology referral when a patient develops
sudden visual blurring in one eye
-
Early OCT and FA to document macular edema and ischemia
-
Starting anti-VEGF therapy as soon as indicated, ideally
within weeks of diagnosis, is associated with better outcomes in recent
literature.
3. Post-RON management
For patients who do undergo Radial Optic Neurotomy:
-
Frequent follow-up visits in the early postoperative
period to monitor vision, intraocular pressure, and the retina
-
Continued use of adjunctive intravitreal drugs if
macular edema persists or recurs
-
Monitoring for neovascularization, retinal detachment,
or choroidal neovascular membranes at the incision site
-
Ongoing systemic risk factor control in collaboration with a physician or
cardiologist
Blood pressure control: Regular screening and treatment of hypertension.
Diabetes management: Good glycemic control and routine ophthalmic exams for diabetic patients.
Lipid management: Diet, exercise, and medication when needed to manage cholesterol.
Smoking cessation: One of the most effective ways to reduce vascular risk.
Managing glaucoma: Regular eye pressure checks and adherence to glaucoma medications if prescribed.
Regular eye exams in at-risk individuals: Older adults and those with cardiovascular disease should have periodic dilated retinal examinations.
Early recognition and treatment can reduce the chance of irreversible vision loss and the need for radical surgery:
-
Prompt ophthalmology referral when a patient develops sudden visual blurring in one eye
-
Early OCT and FA to document macular edema and ischemia
-
Starting anti-VEGF therapy as soon as indicated, ideally within weeks of diagnosis, is associated with better outcomes in recent literature.
3. Post-RON management
For patients who do undergo Radial Optic Neurotomy:
-
Frequent follow-up visits in the early postoperative
period to monitor vision, intraocular pressure, and the retina
-
Continued use of adjunctive intravitreal drugs if
macular edema persists or recurs
-
Monitoring for neovascularization, retinal detachment,
or choroidal neovascular membranes at the incision site
-
Ongoing systemic risk factor control in collaboration with a physician or
cardiologist
Frequent follow-up visits in the early postoperative period to monitor vision, intraocular pressure, and the retina
Continued use of adjunctive intravitreal drugs if macular edema persists or recurs
Monitoring for neovascularization, retinal detachment, or choroidal neovascular membranes at the incision site
Ongoing systemic risk factor control in collaboration with a physician or cardiologist
Complications of Radial Optic Neurotomy
Complications may arise from the underlying CRVO, from vitrectomy, or specifically from the RON incision.
1. Complications of CRVO itself
Even without surgery, CRVO can lead to:
-
Persistent macular edema and chronic visual impairment
-
Ischemic CRVO, with extensive capillary non-perfusion
-
Neovascularization of the iris, angle, or retina,
potentially causing neovascular glaucoma and painful blindness
-
Vitreous hemorrhage or tractional retinal detachment in advanced cases
2. General vitrectomy-related complications
Any pars plana vitrectomy, with or without RON, can be complicated by:
-
Infection (endophthalmitis)
-
Cataract progression in phakic eyes
-
Iatrogenic retinal tears and rhegmatogenous retinal
detachment
-
Postoperative elevated intraocular pressure
3. RON-specific complications
Studies and expert reviews have described several RON-related risks:
-
Laceration of the central retinal artery or vein,
causing immediate, devastating vision loss
-
Optic nerve fiber damage, leading to permanent localized
visual field defects
-
Chorioretinal or choroidal neovascularization developing
at the neurotomy site, which can bleed or scar the macula
-
Globe perforation or excessive scleral damage if the
incision is misdirected
-
Persistent or increased vitreous and retinal hemorrhage
-
In some series, no significant improvement in vision
despite the risks undertaken
A 2016 meta-analysis suggested that RON might reduce the rate of neovascular
glaucoma compared with some alternative therapies, without significantly
changing rates of retinal detachment or vitreous hemorrhage; however, the
overall safety and benefit profile still compares unfavorably with modern
anti-VEGF regimens.
Because of these concerns, careful patient selection and thorough informed
consent are essential before considering Radial Optic Neurotomy.
Persistent macular edema and chronic visual impairment
Ischemic CRVO, with extensive capillary non-perfusion
Neovascularization of the iris, angle, or retina, potentially causing neovascular glaucoma and painful blindness
Vitreous hemorrhage or tractional retinal detachment in advanced cases
Any pars plana vitrectomy, with or without RON, can be complicated by:
-
Infection (endophthalmitis)
-
Cataract progression in phakic eyes
-
Iatrogenic retinal tears and rhegmatogenous retinal detachment
-
Postoperative elevated intraocular pressure
3. RON-specific complications
Studies and expert reviews have described several RON-related risks:
-
Laceration of the central retinal artery or vein,
causing immediate, devastating vision loss
-
Optic nerve fiber damage, leading to permanent localized
visual field defects
-
Chorioretinal or choroidal neovascularization developing
at the neurotomy site, which can bleed or scar the macula
-
Globe perforation or excessive scleral damage if the
incision is misdirected
-
Persistent or increased vitreous and retinal hemorrhage
-
In some series, no significant improvement in vision
despite the risks undertaken
A 2016 meta-analysis suggested that RON might reduce the rate of neovascular
glaucoma compared with some alternative therapies, without significantly
changing rates of retinal detachment or vitreous hemorrhage; however, the
overall safety and benefit profile still compares unfavorably with modern
anti-VEGF regimens.
Because of these concerns, careful patient selection and thorough informed
consent are essential before considering Radial Optic Neurotomy.
Laceration of the central retinal artery or vein, causing immediate, devastating vision loss
Optic nerve fiber damage, leading to permanent localized visual field defects
Chorioretinal or choroidal neovascularization developing at the neurotomy site, which can bleed or scar the macula
Globe perforation or excessive scleral damage if the incision is misdirected
Persistent or increased vitreous and retinal hemorrhage
In some series, no significant improvement in vision despite the risks undertaken
Living with the Condition of Radial Optic Neurotomy
For most patients, the long-term challenge is living with central retinal vein occlusion and its visual consequences, regardless of whether they undergo RON, anti-VEGF treatment, or other procedures.
1. Visual prognosis and expectations
-
With modern therapy, many patients experience improved or
stabilized vision, especially if treatment is started early
and maintained as needed.
-
Some, particularly those with ischemic CRVO or delayed treatment, may be
left with reduced central vision or blind spots.
-
If RON is performed, the visual result can range from significant
improvement to minimal change or, in rare cases, worse vision if
complications occur.
Setting realistic expectations with the treating ophthalmologist is crucial;
patients should understand that no current therapy can guarantee full
restoration of normal eyesight.
2. Daily life and adaptation
Patients may need to adapt in several ways:
-
Using the better eye more while the affected eye is
healing or remains impaired
-
Adjusting lighting conditions at home and work to reduce
glare and improve contrast
-
Magnifying devices, large-print materials, and
high-contrast screens can aid reading and computer use
-
For those with considerable vision loss, low-vision
rehabilitation services can teach strategies for
orientation, mobility, and independent living.
3. Emotional and psychological support
Sudden or chronic visual loss can have a strong emotional impact, causing
anxiety, frustration, or depression. Helpful steps include:
-
Open discussions with the ophthalmologist about prognosis and timelines
-
Support from family and caregivers
-
Counseling or patient support groups for individuals
coping with visual impairment
-
Involving occupational therapists, low-vision specialists, and
rehabilitation counselors when appropriate
4. Long-term medical follow-up
Even after apparent stabilization, lifelong attention to health is important:
-
Regular visits to an ophthalmologist or retina
specialist to monitor the treated eye and the fellow eye
-
Ongoing control of blood pressure, diabetes,
cholesterol, and other systemic factors under the care of a
physician
-
Avoiding smoking and maintaining a heart-healthy lifestyle to minimize
future vascular events
With modern therapy, many patients experience improved or stabilized vision, especially if treatment is started early and maintained as needed.
Some, particularly those with ischemic CRVO or delayed treatment, may be left with reduced central vision or blind spots.
If RON is performed, the visual result can range from significant improvement to minimal change or, in rare cases, worse vision if complications occur.
Patients may need to adapt in several ways:
-
Using the better eye more while the affected eye is healing or remains impaired
-
Adjusting lighting conditions at home and work to reduce glare and improve contrast
-
Magnifying devices, large-print materials, and high-contrast screens can aid reading and computer use
-
For those with considerable vision loss, low-vision rehabilitation services can teach strategies for orientation, mobility, and independent living.
3. Emotional and psychological support
Sudden or chronic visual loss can have a strong emotional impact, causing
anxiety, frustration, or depression. Helpful steps include:
-
Open discussions with the ophthalmologist about prognosis and timelines
-
Support from family and caregivers
-
Counseling or patient support groups for individuals
coping with visual impairment
-
Involving occupational therapists, low-vision specialists, and
rehabilitation counselors when appropriate
4. Long-term medical follow-up
Even after apparent stabilization, lifelong attention to health is important:
-
Regular visits to an ophthalmologist or retina
specialist to monitor the treated eye and the fellow eye
-
Ongoing control of blood pressure, diabetes,
cholesterol, and other systemic factors under the care of a
physician
-
Avoiding smoking and maintaining a heart-healthy lifestyle to minimize
future vascular events
Open discussions with the ophthalmologist about prognosis and timelines
Support from family and caregivers
Counseling or patient support groups for individuals coping with visual impairment
Involving occupational therapists, low-vision specialists, and rehabilitation counselors when appropriate
Even after apparent stabilization, lifelong attention to health is important:
-
Regular visits to an ophthalmologist or retina specialist to monitor the treated eye and the fellow eye
-
Ongoing control of blood pressure, diabetes, cholesterol, and other systemic factors under the care of a physician
-
Avoiding smoking and maintaining a heart-healthy lifestyle to minimize future vascular events
Top 10 Frequently Asked Questions about Radial Optic Neurotomy (RON)
1. What is Radial Optic Neurotomy?
Radial Optic Neurotomy (RON) is a microsurgical procedure used primarily to treat severe vision loss caused by Central Retinal Vein Occlusion (CRVO). In this condition, the vein responsible for draining blood from the retina becomes blocked, leading to swelling, hemorrhage, and sudden visual decline. RON involves creating a tiny radial incision at the edge of the optic nerve head to decompress the central retinal vein and improve blood flow. By relieving this pressure, surgeons aim to restore healthier retinal circulation and prevent further damage. Although controversial in its early years, RON has evolved with improved techniques and has shown promising outcomes in carefully selected patients.
2. Who is considered an ideal candidate for RON?
Candidates for RON are typically patients suffering from severe or non-ischemic CRVO who continue to experience visual deterioration despite standard treatments such as anti-VEGF injections, steroids, or laser therapy. The procedure is usually recommended for individuals who have persistent macular edema, progressive retinal damage, or poor response to medication over several months. Patients must undergo extensive evaluation, including retina imaging and visual-field testing, to ensure that the surgery is appropriate. Individuals with advanced ischemia or irreversible retinal damage may not benefit significantly, and the specialist will weigh potential risks versus benefits before recommending RON.
3. How does Radial Optic Neurotomy help restore vision?
The central idea behind RON is to ease the compression within the optic nerve head caused by venous blockage. When a small radial incision is made, it may widen the scleral ring (a rigid structure surrounding the optic nerve), allowing trapped venous blood to flow more freely. This reduction in pressure leads to decreased swelling, improved oxygen supply to retinal tissues, and gradual absorption of accumulated fluid. Over time, this enhanced perfusion can translate into improved vision and reduced retinal damage. Results vary depending on patient condition, but many individuals show measurable increases in visual acuity.
4. What risks or complications are associated with RON?
Like any eye surgery, RON carries certain risks. Potential complications include bleeding, retinal detachment, infection, optic nerve damage, or worsening vision. Some patients may develop new retinal tears or temporary increases in swelling immediately after the procedure. However, serious complications are relatively rare when performed by a skilled vitreoretinal surgeon experienced in microsurgical techniques. Pre-operative imaging and precise surgical planning significantly reduce risks. Patients are closely monitored after surgery to ensure proper healing and to address any issues promptly.
5. How is the RON procedure performed?
Radial Optic Neurotomy is typically performed under local or general anesthesia and lasts around 30 to 45 minutes. The surgeon begins by performing a vitrectomy, removing the gel-like vitreous to gain safe access to the optic nerve head. Next, using ultra-fine microsurgical instruments, the surgeon creates a precise radial incision at the nasal side of the optic disc. This incision decompresses the central retinal vein region. The procedure is minimally invasive but requires high surgical expertise, as the optic nerve is a delicate and crucial structure.
6. What is the typical recovery timeline after RON?
Recovery after RON varies, but most patients can resume non-strenuous activities within a few days. Mild discomfort, redness, or blurred vision is expected initially. Improvement in retinal swelling and vision may begin within weeks but often continues for several months as circulation stabilizes. Post-operative visits are essential for monitoring healing, assessing visual progress, and managing any complications early. Eye drops or medications may be prescribed to reduce inflammation and support recovery.
7. How successful is RON in improving vision?
Success rates depend heavily on the severity of the CRVO and the patient’s overall retinal health. Many patients experience stabilization and moderate improvement in vision, while others see significant enhancement. A portion of patients may not experience noticeable improvement, especially if ischemia or extensive retinal damage is present before surgery. However, studies and clinical reports show that RON can provide meaningful outcomes for selected individuals who did not benefit sufficiently from medical therapies.
8. Can both eyes be treated with RON?
CRVO typically affects only one eye, and RON is performed only on the affected side. In extremely rare cases where both eyes are affected at different times, each eye would be evaluated independently. Surgeons carefully assess whether the second eye truly requires surgical intervention or whether medical therapy may be more suitable, as bilateral CRVO often indicates underlying systemic conditions needing medical attention.
9. What alternatives exist besides RON?
Before considering RON, most patients undergo standard treatments such as anti-VEGF injections, intravitreal steroids, and laser photocoagulation. These treatments aim to reduce macular edema and prevent further vision loss. In many cases, they stabilize or improve vision without the need for surgery. Other emerging therapies and clinical trials may also be available. RON is typically reserved for patients who do not achieve satisfactory results with conventional treatments.
10. Are the results of RON permanent?
The benefits of RON can be long-lasting, but outcomes vary depending on patient health and the underlying severity of CRVO. If the procedure successfully restores venous outflow and reduces swelling, improvements may persist for years. However, patients must continue regular eye examinations to monitor retinal health, as ongoing vascular issues or systemic diseases (such as hypertension or diabetes) may influence long-term results.


