Introduction to Radical Cystectomy & Urinary Diversion
Radical cystectomy with urinary diversion is a major urologic surgery most commonly performed for muscle-invasive bladder cancer (MIBC) and some high-risk non-muscle-invasive cancers that have failed conservative treatments. In a radical cystectomy, the surgeon removes the entire urinary bladder, surrounding lymph nodes, and in many cases nearby organs that may harbor microscopic cancer cells. In men this typically includes the prostate and seminal vesicles; in women it may include the uterus, ovaries, fallopian tubes and part of the anterior vaginal wall. The primary goal is oncologic: to remove the cancer completely and reduce the risk of spread or recurrence.
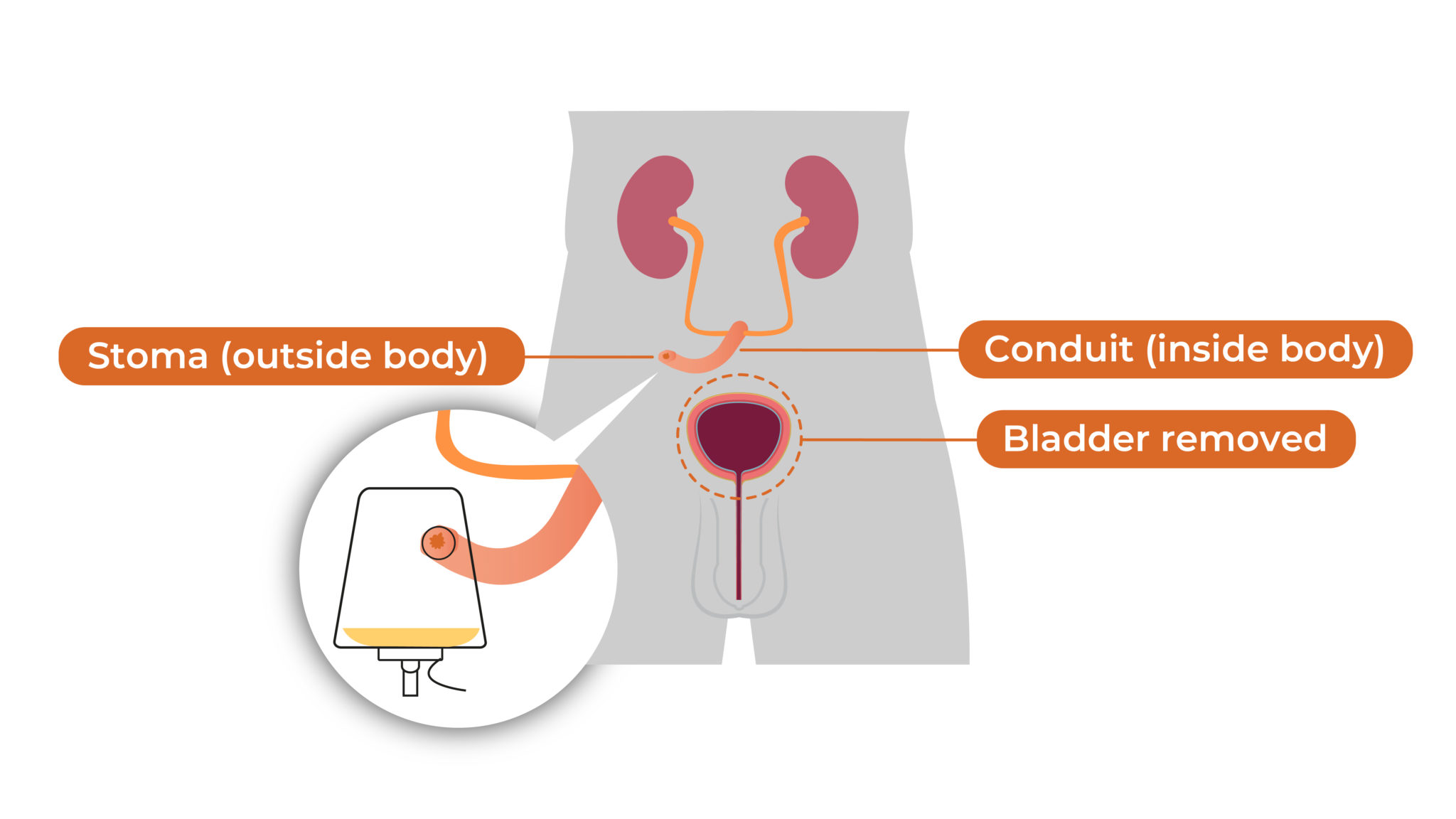
Because the bladder's function is to store urine at low pressure and expel it voluntarily, its removal creates a need for a new pathway for urine to leave the body, known as a urinary diversion. There are two broad categories of urinary diversion: incontinent diversions, such as the ileal conduit (Bricker conduit), where urine flows continuously into an external stoma bag; and continent diversions, which include orthotopic neobladders (internal reservoirs connected to the urethra so the patient voids through the natural route) and continent catheterizable pouches drained periodically by catheter. These reconstructions are usually formed from segments of intestine and are carefully tailored to each patient's anatomy, cancer stage, kidney function and lifestyle.
Today, radical cystectomy and urinary diversion can be performed through an open approach, laparoscopy, or robot-assisted surgery, with similar cancer control when done by experienced teams. However, it remains one of the most complex procedures in urology, associated with substantial short- and long-term morbidity, which is why high-volume centers and standardized Enhanced Recovery After Surgery (ERAS) protocols are strongly recommended to optimize outcomes, shorten hospital stay and reduce complications.
Causes and Risk of Radical Cystectomy & Urinary Diversion
Radical cystectomy is not a disease; it is a treatment for serious bladder or pelvic pathology. The "causes" for needing this surgery are the underlying conditions that damage or threaten the bladder, most commonly bladder cancer. Muscle-invasive bladder cancer (T2-T4a, N0-Nx, M0) is the main indication, as guidelines consistently identify radical cystectomy with pelvic lymph node dissection and urinary diversion as the standard of care for patients fit for major surgery. It is also recommended for selected very high-risk non-muscle-invasive tumors that have failed intravesical therapies such as BCG.
Less commonly, radical cystectomy may be performed for:
-
Refractory interstitial cystitis or bladder pain syndrome causing debilitating symptoms
-
Severe radiation cystitis after pelvic radiotherapy
-
Neurogenic bladder with intractable incontinence and repeated infections
-
Extensive pelvic trauma or congenital abnormalities resulting in a non-functional bladder
The risk profile of radical cystectomy & urinary diversion is influenced by several factors:
-
Patient-related risk factors
-
Advanced age and frailty
-
Comorbidities such as cardiovascular disease, diabetes, chronic kidney disease, COPD and obesity
-
Poor nutritional status, anemia, or low albumin
-
Active smoking and poor pulmonary reserve
These factors increase the risk of wound complications, infections, thromboembolism, and prolonged recovery.
-
-
Disease-related risk factors
-
High tumor stage and nodal disease
-
Prior pelvic surgery or radiotherapy
-
Locally advanced tumors invading adjacent organs
These can complicate surgery, increase blood loss, and raise the risk of positive margins or postoperative fistulae.
-
-
Surgery and diversion-related risk factors
-
Length of surgery and blood loss
-
Choice of diversion (ileal conduit vs orthotopic neobladder vs continent pouch)
-
Use of bowel segments (ileum, colon) and their metabolic consequences
-
Experience and volume of the surgical center
-
High-volume centers and surgeons who perform at least 10-20 cystectomies annually are associated with better peri-operative and long-term outcomes, which is reflected in modern guidelines.
Symptoms and Signs of Radical Cystectomy & Urinary Diversion-Related Conditions
People who eventually undergo radical cystectomy usually present with symptoms of the underlying bladder disease, most often bladder cancer. The classic presentation is visible blood in the urine (gross hematuria), which may be intermittent and painless. Other urinary symptoms include frequency, urgency, burning during urination, or difficulty emptying the bladder. As disease advances, patients may experience pelvic pain, flank pain from obstruction of the ureters, recurrent urinary tract infections, or systemic signs such as weight loss and fatigue.
On examination and investigations before surgery, clinicians may find:
-
Persistent microscopic or gross hematuria on urinalysis
-
Mass or thickening of the bladder wall on cystoscopy and imaging
-
Hydronephrosis (swelling of kidneys due to blockage) on ultrasound or CT
-
Positive urine cytology for malignant cells
After radical cystectomy and urinary diversion, the symptoms and signs shift to those related to surgical recovery and the function of the new urinary system. In the immediate postoperative period, common experiences include:
-
Abdominal pain and tenderness at incision or port sites
-
Temporary bowel paralysis (ileus), bloating and delayed return of normal bowel function
-
Drain tubes and urinary catheters in place
-
Fatigue, weakness and decreased appetite
Warning signs that need urgent attention include fever, increasing abdominal pain, wound redness or discharge, lack of bowel function, chest pain, shortness of breath, leg swelling or sudden changes in urine output. These may signal infection, deep vein thrombosis, pulmonary embolism, anastomotic leaks or bowel obstruction.
In the long-term, symptoms depend on diversion type:
-
Ileal conduit - issues may include changes around the stoma, leakage from the appliance, skin irritation, or changes in urine output.
-
Orthotopic neobladder - patients may report urinary incontinence (especially at night), the need to strain to void, a feeling of incomplete emptying, or recurrent urinary infections.
-
Continent catheterizable reservoirs - difficulty catheterizing, leakage between catheterizations, or recurrent infections.
Patients should receive clear pre-operative counseling so they understand which symptoms are expected and which warrant urgent medical contact.
Diagnosis of Radical Cystectomy & Urinary Diversion-Related Condition
The pathway to radical cystectomy begins with diagnosing the underlying bladder pathology and staging it accurately. This includes:
-
Initial evaluation
-
Detailed history focusing on hematuria, irritative symptoms, smoking, chemical exposures, and family history of urothelial cancer
-
Physical examination including abdominal and pelvic exam, digital rectal exam in men, and pelvic bimanual exam in women
-
-
Laboratory studies
-
Urinalysis and urine culture to rule out infection
-
Urine cytology to detect malignant urothelial cells
-
Baseline renal and liver function tests, blood count and coagulation profile
-
-
Endoscopic assessment (cystoscopy)
Cystoscopy is the gold standard for visualizing the bladder mucosa, identifying tumors and taking biopsies or performing a transurethral resection of bladder tumor (TURBT). TURBT specimens provide histology, grade and depth of invasion, which are critical for staging and treatment selection. -
Imaging for staging
-
CT urography or MRI of the abdomen and pelvis to evaluate tumor extent, lymph nodes and upper urinary tracts
-
Chest imaging (X-ray or CT) to look for metastases
-
In some cases, bone scans or PET/CT if there are suspicious symptoms or lab abnormalities
-
-
Risk stratification and multidisciplinary review
Based on tumor stage (T), nodal status (N), metastasis (M), grade and patient comorbidities, a multidisciplinary team (urologist, oncologist, radiologist, pathologist, nurse specialist) recommends treatment. For fit patients with muscle-invasive or very high-risk disease, radical cystectomy with urinary diversion is usually offered, often with neoadjuvant cisplatin-based chemotherapy to improve survival. -
Pre-operative assessment for cystectomy and diversion
-
Cardiac and pulmonary clearance for major surgery
-
Nutritional assessment and optimization
-
Evaluation of renal function and intestinal health (since bowel segments will be used)
-
Discussion of diversion options: ileal conduit vs neobladder vs continent pouch, considering age, manual dexterity, urethral status, kidney function, previous pelvic radiotherapy, and patient preference
-
Stoma site marking by an experienced stoma therapist for patients likely to have an external stoma
-
This structured work-up ensures patients who proceed to radical cystectomy & urinary diversion are properly selected, medically optimized and informed about the implications of each reconstruction option.
Treatment Options of Radical Cystectomy & Urinary Diversion
Once radical cystectomy is indicated, treatment planning covers both cancer control and urinary reconstruction.
1. Surgical approach to radical cystectomy
-
Open radical cystectomy (ORC) - traditional midline incision, still widely used and considered the reference technique.
-
Laparoscopic radical cystectomy - performed through keyhole incisions; technically demanding but can reduce blood loss and incision size.
-
Robot-assisted radical cystectomy (RARC) - uses robotic platforms to enhance visualization and instrument precision; increasingly common, with similar oncologic outcomes and potential benefits in blood loss and length of stay, especially when combined with ERAS protocols.
The choice depends on surgeon expertise, equipment availability and patient factors; the priority remains complete cancer removal with adequate lymph node dissection.
2. Types of urinary diversion
a. Incontinent diversion - Ileal conduit
The ileal conduit is the most commonly performed diversion worldwide. A short
segment of ileum is isolated and the ureters are implanted into it; the other
end of the segment is brought out through the abdominal wall to create a stoma.
Urine drains continuously into a collecting bag attached to the skin. Advantages
include shorter operative time, simpler technique, and suitability for older or
frail patients. Disadvantages include lifelong stoma care, appliance dependence
and risk of stomal and metabolic complications.
b. Continent orthotopic neobladder
Here, a reservoir is constructed from a longer segment of intestine (usually
ileum) and connected to the urethra, allowing patients to void per urethram,
simulating normal urination. The Studer neobladder is a widely used
configuration. This option can offer excellent body image and quality of life
for selected, motivated patients with good renal function and intact urethral
sphincter. However, it requires more complex surgery, a longer recovery and the
ability to learn new voiding techniques, with possible long-term risks such as
incontinence, retention, metabolic disturbances and upper tract deterioration.
c. Continent cutaneous diversion (catheterizable pouch)
In this option, a reservoir is created from bowel and connected to the skin via
a narrow channel that can be catheterized (e.g., Indiana pouch, Mainz pouch).
Patients drain the reservoir with a catheter every few hours and wear only a
small dressing over the stoma. It is useful when urethral voiding is not
possible but the patient desires continence without an external bag. It demands
manual dexterity, strict adherence to catheterization schedules and lifelong
follow-up.
3. Peri-operative optimization - ERAS protocols
Enhanced Recovery After Surgery (ERAS) pathways have become standard in many centers for radical cystectomy. Key elements include:
-
Pre-operative counseling, smoking cessation, nutrition optimization and exercise ("pre-habilitation")
-
Avoidance of prolonged fasting and routine bowel prep
-
Goal-directed fluid therapy and multimodal analgesia to minimize opioids
-
Early mobilization, early oral intake and careful drain/catheter management
ERAS has been shown to reduce complications, ileus, readmission rates, transfusions, length of stay and time to bowel recovery after radical cystectomy.
4. Systemic therapies
Depending on stage and risk features, surgery may be integrated with:
-
Neoadjuvant chemotherapy (before surgery) to improve survival in eligible patients with muscle-invasive disease
-
Adjuvant chemotherapy or immunotherapy after surgery in patients with adverse features (e.g., pT3/4 or node-positive) who did not receive neoadjuvant treatment or remain high risk. Updated guidelines now include adjuvant nivolumab as an option in selected high-risk cases.
Prevention and Management of Radical Cystectomy & Urinary Diversion
Because cystectomy is major, life-altering surgery, prevention focuses on both reducing the risk of needing it and optimizing outcomes when it is necessary.
1. Preventing or delaying the need for radical cystectomy
-
Smoking cessation: Smoking is the strongest preventable risk factor for bladder cancer. Quitting reduces incidence and recurrence.
-
Occupational safety: Minimizing exposure to aromatic amines and industrial chemicals.
-
Early evaluation of hematuria: Prompt cystoscopic assessment of any visible blood in the urine enables diagnosis and treatment at earlier stages.
-
Adherence to intravesical therapies: For non-muscle-invasive disease, proper BCG or chemotherapy instillations can reduce progression and delay or avoid cystectomy in some patients.
2. Pre-operative management to improve surgical outcomes
-
Comprehensive assessment and control of comorbidities (cardiac, pulmonary, renal, metabolic).
-
Correction of anemia and nutritional deficits; involvement of dietitians when needed.
-
Smoking and alcohol reduction; optimization of glycemic control in diabetics.
-
Prehabilitation: targeted exercise, breathing training, and education about early mobilization.
-
Detailed counseling about diversion options and lifestyle implications; meeting with a stoma nurse and, if possible, patients who have undergone similar surgery.
3. Post-operative and long-term management
After hospital discharge, patients require:
-
Regular follow-up with the urology team to monitor wound healing, diversion function and cancer surveillance.
-
Imaging (CT of thorax/abdomen) for several years to detect recurrence or metastases, as recommended by guidelines.
-
Blood tests to monitor kidney function and electrolytes.
-
Vitamin B12 monitoring and supplementation in patients with ileal segments used, as B12 absorption may be impaired.
-
Education about hydration, infection prevention, stoma or catheter care, and early recognition of complications such as obstruction or metabolic acidosis.
Proactive management-combined with ERAS pathways and good patient education-can significantly improve long-term outcomes and quality of life after radical cystectomy & urinary diversion.
Complications of Radical Cystectomy & Urinary Diversion
Radical cystectomy is associated with high complication rates, with studies reporting early complications in 50-80% of patients and non-trivial 90-day mortality, especially in older, comorbid populations. Complications can be divided into early (within 30-90 days) and late (months to years).
1. Early complications
-
General surgical complications: bleeding requiring transfusion, wound infection, dehiscence, hernia, deep vein thrombosis and pulmonary embolism, pneumonia and sepsis.
-
Bowel-related complications: postoperative ileus, small bowel obstruction, anastomotic leaks, intra-abdominal abscesses and diarrhea.
-
Urinary complications: urine leaks from uretero-enteric anastomoses or reservoir, leading to collections, peritonitis or sepsis.
-
Cardiovascular events: myocardial infarction, arrhythmias, stroke, particularly in high-risk patients.
2. Long-term complications related to urinary diversion
Complication patterns differ between diversion types, but overall long-term complication rates of 30-60% are reported for both ileal conduits and continent diversions.
Ileal conduit (incontinent diversion):
-
Stoma issues: retraction, prolapse, stenosis, parastomal hernia, skin irritation and appliance leakage.
-
Uretero-enteric strictures, leading to hydronephrosis and potential renal impairment.
-
Recurrent urinary tract infections, stones in the conduit or kidneys.
-
Metabolic complications such as hyperchloremic metabolic acidosis and vitamin B12 deficiency due to ileal resection.
Orthotopic neobladder (continent diversion):
-
Daytime and nighttime incontinence (especially nocturnal), or conversely, urinary retention requiring intermittent catheterization.
-
Urethral or ileourethral strictures.
-
Mucus production and stone formation within the neobladder.
-
Recurrent UTIs and pyelonephritis.
-
Metabolic acidosis, electrolyte disturbances and long-term risk of renal function decline.
Continent catheterizable reservoirs:
-
Stomal stenosis or difficulty catheterizing.
-
Pouch leaks or overdistension if catheterization is inadequate.
-
Stones, infections and metabolic issues similar to neobladders.
Long-term quality of life can be good to excellent for many patients, but depends heavily on complication control, realistic expectations, and ongoing follow-up. Recent work continues to investigate how diversion choice and patient age influence health-related quality of life across decades after surgery.
Living with the Condition of Radical Cystectomy & Urinary Diversion
"Living with radical cystectomy & urinary diversion" means adapting to a new way of passing urine, coping with the physical and emotional consequences of a major cancer operation, and committing to lifelong follow-up.
1. Daily life and self-care
-
Ileal conduit: Patients learn how to care for their stoma, change the appliance, protect the surrounding skin and manage the collecting bag discreetly under clothing. Modern appliances are secure and low-profile, enabling normal activities, work, sport and travel. Stoma nurses are key allies, especially in the first months.
-
Neobladder: Patients must retrain their pelvic floor, learn scheduled voiding, and sometimes use intermittent catheterization. Nighttime incontinence is common initially; pelvic floor exercises and behavioral strategies can improve control.
-
Continent pouches: Patients commit to regular catheterization (for example every 4-6 hours), even when they do not feel full, to avoid overdistension and leakage.
Hydration, attention to urine appearance and early management of UTIs are important in all diversion types.
2. Emotional, social and sexual well-being
Radical cystectomy can significantly affect body image, sexuality and self-confidence. Men may experience erectile dysfunction and changes in ejaculation after removal of the prostate and seminal vesicles; women may notice vaginal shortening or dryness after anterior pelvic exenteration. Open communication with partners, use of medications or devices for erectile dysfunction, pelvic floor rehabilitation and, when needed, counseling with a psycho-oncologist can be extremely helpful.
Patients often benefit from:
-
Support groups or online communities of people living with ostomies or neobladders
-
Psychosocial support for dealing with fear of recurrence, fatigue and lifestyle changes
-
Practical advice on clothing, sports, travel, intimacy and work
3. Long-term medical follow-up
Even years after surgery, follow-up remains essential:
-
Regular urologic review with physical exam and imaging to detect cancer recurrence or upper tract changes
-
Laboratory monitoring of kidney function, electrolytes and vitamin B12 (especially with ileal segments)
-
Periodic assessment of diversion function, continence, and need for interventions such as stoma revision, stricture dilation or stone treatment
4. Outlook and quality of life
While radical cystectomy & urinary diversion is life-changing, many patients are able to return to work, engage in physical activity, travel, maintain intimate relationships and enjoy a good quality of life-especially when surgery is done in experienced centers, complications are promptly managed, and patients are well-supported with education and rehabilitation. With modern surgical techniques, ERAS pathways, and better understanding of long-term diversion care, survival and quality-of-life outcomes continue to improve for people undergoing this major cancer operation.
Top 10 Frequently Asked Questions about Radical Cystectomy & Urinary Diversion
1. What is a Radical Cystectomy?
A Radical Cystectomy is a major surgical procedure in which the urinary bladder is completely removed, usually to treat muscle-invasive bladder cancer or high-risk recurrent tumors. In men, the prostate and seminal vesicles are often removed as well, while women may have the uterus, ovaries, fallopian tubes, and a portion of the vaginal wall removed depending on disease extent. The goal is to eliminate cancer and prevent further spread, making it one of the most effective treatments for advanced bladder disease.
2. Why is Urinary Diversion needed after bladder removal?
Because the bladder stores urine, its removal requires surgeons to create a new system for urine to exit the body. Urinary diversion provides an alternate pathway using bowel segments. The most common types include an ileal conduit (stoma bag), a continent cutaneous reservoir (internal pouch emptied with a catheter), or an orthotopic neobladder (new bladder connected to the urethra). The type chosen depends on cancer stage, anatomy, lifestyle, and overall health.
3. What conditions typically require this surgery?
Radical Cystectomy is most often performed for muscle-invasive bladder cancer, but may also be recommended for high-grade recurrent tumors, aggressive carcinoma in situ, or certain benign but severe bladder diseases like refractory interstitial cystitis or radiation damage when all other treatments fail.
4. How is the surgery performed?
The procedure can be done via open surgery, laparoscopic methods, or robot-assisted techniques. After removing the bladder and nearby organs, surgeons use a small section of the intestine to create the urinary diversion. Depending on the method, the operation typically lasts 4-8 hours and requires precision to protect surrounding structures and ensure proper urinary function.
5. What are the risks and complications?
Risks include bleeding, infection, blood clots, bowel obstruction, leakage from urinary reconstructions, and wound complications. Long-term issues may involve electrolyte imbalances, kidney function decline, urinary infections, or stoma problems. Despite potential risks, outcomes are generally favorable when performed by experienced urological surgeons.
6. What is the recovery process like?
Recovery involves a hospital stay of 7-10 days, gradual return to eating, and learning to manage the chosen urinary diversion. Full recovery can take several weeks to months, depending on the patient's overall health. Follow-up visits monitor healing, kidney function, and cancer surveillance.
7. How will life change after urinary diversion?
Most patients adjust well after surgery. Those with an ileal conduit learn stoma care and bag changes, while neobladder patients learn new patterns for urination and pelvic muscle training. With proper support, individuals can return to work, exercise, travel, and sexual activity.
8. Is a neobladder suitable for everyone?
No. A neobladder works best for patients who are healthy, cancer-free at the urethral margin, and motivated for rehabilitation. Patients with poor kidney function, advanced age, or certain cancers may be better candidates for an ileal conduit or continent reservoir.
9. Will sexual function be affected?
Sexual function can change. Men may experience erectile dysfunction depending on nerve preservation during surgery, while women may notice vaginal changes or reduced lubrication. Many treatments and rehabilitation options are available, including medications and pelvic-floor therapy.
10. What long-term follow-up is required?
Patients need regular monitoring for kidney function, metabolic balance, cancer recurrence, and the health of the urinary diversion. Lifelong follow-up ensures early detection of complications and supports long-term quality of life.


