Introduction to Radical Bilateral Orchidectomy
Radical Bilateral Orchidectomy is a major urological surgical procedure in which both testicles along with the spermatic cords are removed through an incision in the groin area. This technique, known as the radical inguinal approach, is the gold standard whenever a testicular tumour is suspected, because it prevents cancer cells from spreading to the scrotum. While unilateral (single-side) orchidectomy is more common, bilateral orchidectomy becomes necessary when both testicles are affected by disease or when treatment goals require the complete removal of testosterone production. This procedure is often used in cases of bilateral testicular cancer, synchronous or metachronous testicular tumours, severe trauma affecting both testes, or as an irreversible method of androgen deprivation therapy in advanced prostate cancer where hormonal suppression is required.
This type of surgery has major implications for reproductive, endocrine, and emotional health because the testes produce sperm for fertility and testosterone for sexual and metabolic functions. As a result, a radical bilateral orchidectomy permanently eliminates the body’s natural supply of testosterone and sperm, leading to infertility and requiring lifelong hormonal monitoring or replacement depending on the underlying condition. Despite its life-changing nature, the procedure is often essential and potentially life-saving. With improved surgical techniques, early diagnosis methods, and advanced postoperative hormonal management, individuals undergoing this operation can maintain a good quality of life. Understanding the details of why and how this surgery is performed helps patients make informed decisions and prepare physically and emotionally for the recovery process.
Causes and Risk Factors Leading to Radical Bilateral Orchidectomy
Primary Causes
The most important medical reason for recommending radical bilateral orchidectomy is testicular cancer affecting both testicles. This may occur either simultaneously (at the same time) or sequentially over months or years. Although testicular cancer is among the most treatable cancers, bilateral involvement is rare but serious. Once a tumour is identified, radical removal through an inguinal cut is the safest way to prevent further spread.
Another cause is advanced prostate cancer, in which bilateral orchidectomy may be used as a hormonal therapy. Because the testicles produce the majority of natural testosterone, and prostate cancer often grows in the presence of this hormone, removing both testicles drastically reduces hormone levels, slowing cancer progression.
Other rare causes include major trauma that destroys the function of both testes, severe infections that cannot be controlled, complications of previous surgeries, or in unique cases, congenital and developmental abnormalities leading to dysfunctional testicles that may require removal.
Risk Factors
The risk factors are closely related to the underlying diseases that require surgery:
-
Undescended testicle (cryptorchidism)—men born with one or both testes not fully descended have a markedly higher risk of developing testicular cancer later in life.
-
Previous testicular cancer—those who have had cancer in one testicle are at higher risk for cancer in the remaining one.
-
Family history—first-degree relatives (father, brother) with testicular cancer increase risk.
-
Infertility and testicular atrophy—men with small, underdeveloped, or dysfunctional testes may be more susceptible to cancer.
-
Genetic abnormalities—conditions affecting testicular development may predispose individuals to bilateral disease.
-
Long-term hormonal disorders—which may increase risk for testicular abnormalities.
Understanding risks and causes helps improve awareness, promotes early detection, and influences preventive practices.
Symptoms and Signs of Conditions Leading to Radical Bilateral Orchidectomy
Symptoms vary depending on the underlying condition, but the most common warning signs related to testicular cancer include:
-
A painless lump or hard area in one or both testicles
-
Swelling, heaviness, or enlargement of the scrotum
-
Dull ache in the lower abdomen or groin
-
Noticeable difference in size or firmness between the two testicles
-
Sudden build-up of fluid around the testicle (hydrocele)
-
Persistent discomfort or feeling of dragging in the scrotum
If cancer spreads beyond the testicles, symptoms may progress to include back pain (from abdominal lymph nodes), chest symptoms, or fatigue. When both testicles are affected, symptoms may be bilateral, though not always symmetrical.
In cases where bilateral orchidectomy is performed for advanced prostate cancer, symptoms leading to diagnosis include difficulty urinating, frequent urination, pain during urination, pelvic discomfort, bone pain, or unexplained weight loss.
Over time, men may also notice hormonal changes such as reduced libido, erectile difficulties, fatigue, or unusual mood shifts—particularly if both testes are failing before surgery.
Diagnosis of Conditions Requiring Radical Bilateral Orchidectomy
Diagnosis typically begins with a combination of clinical evaluation, imaging, and laboratory tests:
1. Medical History and Physical Examination
A doctor assesses symptoms, risk factors, changes in testicular size or consistency, and any discomfort in the scrotum or groin. Physical examination helps detect masses or irregularities.
2. Scrotal Ultrasound
Ultrasound is the most reliable, non-invasive imaging method to evaluate testicular lumps. It helps distinguish between solid tumours and fluid-filled lesions and determines whether the mass is likely cancerous.
3. Blood Tumour Markers
Specific substances in the blood, such as AFP, β-hCG, and LDH, help identify testicular cancer and assist in staging and monitoring. Elevated levels suggest malignancy.
4. Imaging for Staging
If cancer is suspected, CT scans or MRI scans of the abdomen, pelvis, and chest are used to check for tumour spread.
5. No Needle Biopsy
Unlike many cancers, testicular cancer is not diagnosed through biopsy because puncturing the testicle risks spreading cancer cells. Radical inguinal removal of the testicle is both diagnostic and therapeutic.
6. Pre-surgical Assessments
For patients requiring bilateral surgery, preoperative planning includes:
-
Hormone level evaluation
-
Fertility discussions and sperm banking
-
Psychological preparation
-
Evaluation of suitability for a testicular prosthesis
These steps ensure that the patient understands the full implications and is prepared for the next stages of treatment.
Treatment Options and the Radical Bilateral Orchidectomy Procedure
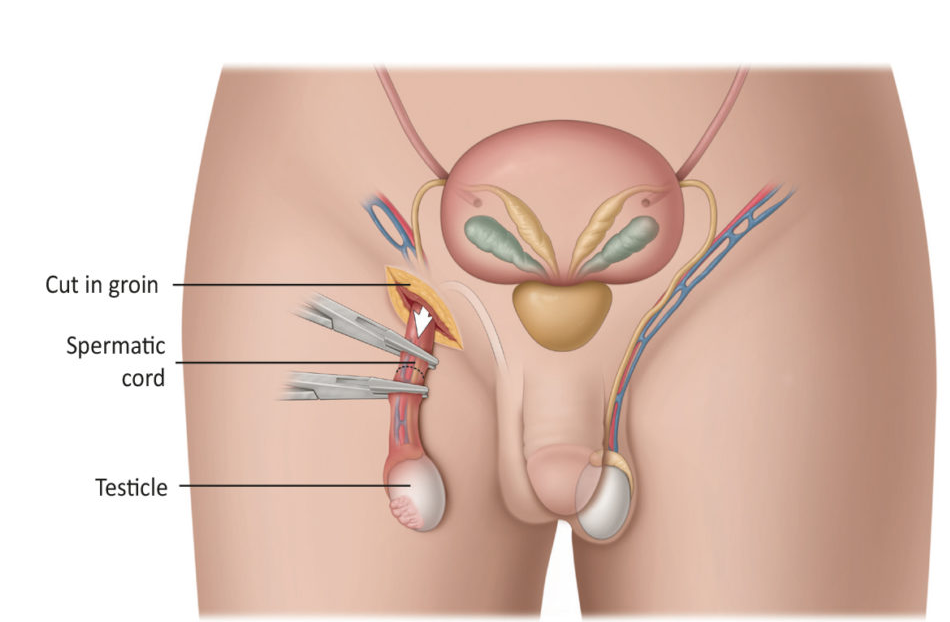
The Surgical Approach
Radical bilateral orchidectomy is performed under general or spinal anaesthesia. The surgeon makes an incision in the groin (never through the scrotum) and removes the testicle and spermatic cord as a complete unit. This process is repeated for the second testicle either during the same operation or during a staged procedure if needed.
Why This Approach?
The inguinal route prevents cancer cells from spreading into the scrotum and ensures a clean removal of tissue. This significantly reduces recurrence risk in cancer cases.
Preoperative Preparation
Patients receive detailed counselling regarding:
-
Permanent infertility after removal of both testes
-
Hormonal consequences and possible testosterone replacement
-
Options for testicular prosthesis
-
Surgical risks and recovery time
-
Possibility of additional cancer treatments such as chemotherapy or radiation
Postoperative Care
Recovery typically includes:
-
Pain control and anti-inflammatory medications
-
Scrotal support garments to reduce swelling
-
Activity restrictions for 2-4 weeks
-
Regular monitoring of hormone levels
-
Oncology follow-up for cancer cases
-
Evaluation for testosterone replacement therapy if needed
Adjunct Treatments
Depending on the underlying condition:
-
Testicular cancer may require chemotherapy or radiotherapy
-
Prostate cancer patients may continue on systemic treatments
-
Hormone replacement therapy may be essential for maintaining long-term physical and emotional health
Prevention and Management Strategies
Preventing Underlying Disease
While testicular cancer cannot always be prevented, early detection remains the most powerful protective measure. Monthly testicular self-examination, prompt evaluation of any swelling or discomfort, and corrective surgery for undescended testes in childhood significantly reduce risk.
Post-Surgical Management
Because bilateral orchidectomy has lifelong consequences, proper management includes:
-
Testosterone Replacement Therapy (TRT) when medically appropriate, which improves energy, libido, bone strength, and emotional stability
-
Fertility preservation strategies such as sperm banking before surgery
-
Lifestyle measures like weight training, healthy diet, and quitting smoking to maintain bone density and muscle mass
-
Regular follow-ups with urologists, endocrinologists, and oncologists
Psychological Support
Counselling is recommended for coping with changes in fertility, physical appearance, sexual function, and emotional well-being. Support groups and mental health services help patients adapt to life after surgery.
Complications of Radical Bilateral Orchidectomy
Immediate Surgical Risks
-
Bleeding or haematoma in the scrotal area
-
Surgical site infection
-
Nerve injury leading to numbness around the inner thigh or groin
-
Wound healing complications
-
Inguinal hernia formation
Long-Term Effects
-
Permanent infertility
-
Loss of testosterone production
-
Erectile dysfunction and loss of libido
-
Fatigue, mood changes, and decreased muscle mass
-
Increased risk of osteoporosis due to low androgen levels
-
Prosthesis-related issues such as displacement or infection
These complications emphasize the importance of follow-up care, hormone monitoring, and lifestyle adjustments.
Living with the Condition After Radical Bilateral Orchidectomy
Life after bilateral orchidectomy involves major adjustments, but with proper support, patients can achieve good long-term health and emotional well-being.
Physical Health
Patients who are not undergoing androgen suppression for prostate cancer will require testosterone replacement through injections, patches, gels, or implants. Regular hormone tests ensure correct dosage. Maintaining physical activity, especially resistance training, helps counteract muscle loss and bone weakening.
Sexual and Reproductive Health
Even though fertility is lost, sexual function can often be restored with hormonal therapy and medications for erectile dysfunction if necessary. Open communication with partners helps maintain emotional intimacy.
Psychological and Emotional Well-Being
Loss of the testicles may affect body image, confidence, or the sense of masculinity. Counselling, peer support groups, and open discussions with healthcare providers significantly help patients adapt.
Daily Life and Long-Term Outlook
Most patients return to normal life, work, and social activities within weeks after surgery. With consistent follow-ups and lifestyle care, long-term health outcomes are generally positive. The key is awareness, consistent medical supervision, and strong emotional support.
Top 10 Frequently Asked Questions about Radical Orchidectomy (Bilateral)
1. What is a Radical Bilateral Orchidectomy?
A Radical Bilateral Orchidectomy is a surgical procedure involving the removal of both testicles (testes). It is often performed as a treatment for testicular cancer, advanced prostate cancer, or certain cases of severe testicular trauma or infection. The term “radical” means that the procedure removes not only the testes but also the surrounding structures such as the spermatic cords to ensure complete removal of any potentially cancerous tissue.
2. Why is a Bilateral Orchidectomy performed?
This surgery is primarily done to:
-
Treat prostate cancer by lowering testosterone levels (which can fuel cancer growth).
-
Remove malignant testicular tumors when cancer is found in both testicles.
-
Manage hormone-related conditions or gender-affirming surgery in certain transgender patients.
-
Address severe injury or infection when both testicles are damaged beyond repair.
3. How is the procedure performed?
A bilateral radical orchidectomy is performed under general or spinal anesthesia.
-
The surgeon makes an incision in the groin area (inguinal approach), not the scrotum, to prevent cancer spread.
-
Each testicle and spermatic cord are gently lifted out and removed.
-
The wound is then sutured closed, and a dressing is applied.
The surgery typically takes about 30 to 60 minutes.
4. What are the risks and possible complications?
While it is generally safe, potential risks include:
-
Bleeding or hematoma formation
-
Infection at the incision site
-
Chronic scrotal or groin pain
-
Psychological effects (loss of masculinity or sexual confidence)
-
Infertility and permanent loss of testosterone production
Your healthcare team will take measures to minimize these risks.
5. What is the recovery time after surgery?
Most patients recover within 2-3 weeks, though complete healing can take up to 6 weeks.
-
Light activities can resume within a few days.
-
Avoid strenuous exercise, heavy lifting, or sexual activity for at least 4-6 weeks.
-
Pain and swelling are managed with prescribed medications and supportive garments.
6. Will the surgery affect sexual function?
Yes, to some extent. Since both testicles produce testosterone:
-
Erectile function may gradually decline without hormone replacement.
-
Sex drive (libido) can decrease due to low testosterone levels.
-
Ejaculation is no longer possible, resulting in permanent infertility.
However, testosterone replacement therapy (TRT) can help maintain sexual function and overall well-being.
7. Can prosthetic testicles be inserted after orchidectomy?
Yes. Many patients choose to have testicular prostheses implanted for cosmetic and psychological reasons. These silicone implants are placed during or after the orchidectomy to restore the natural appearance of the scrotum.
8. What hormonal changes occur after a bilateral orchidectomy?
With both testicles removed, testosterone production ceases, leading to:
-
Hot flashes
-
Fatigue
-
Decreased muscle mass
-
Mood swings or depression
-
Reduced bone density (osteoporosis risk)
Doctors often prescribe hormone replacement therapy (HRT) to balance testosterone levels and prevent these side effects.
9. Is the surgery reversible?
No. A radical bilateral orchidectomy is permanent and
irreversible.
If fertility preservation is a concern, sperm banking should be
discussed before the surgery.
10. What is the long-term outlook after a bilateral orchidectomy?
The prognosis largely depends on the underlying reason for surgery:
-
For cancer patients, it can be curative or life-prolonging.
-
With proper hormone therapy, most men lead normal, healthy lives.
-
Regular follow-ups are essential to monitor hormone levels, bone health, and emotional well-being.


