Introduction to Radical Prostatectomy
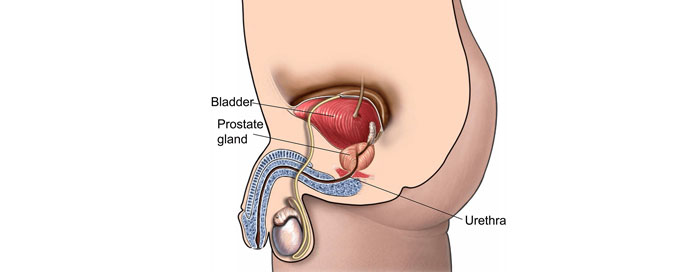
Radical prostatectomy is a major surgical procedure performed to treat prostate cancer. The prostate is a small, walnut-sized gland located beneath the bladder and in front of the rectum, which produces the fluid that helps nourish and transport sperm. When prostate cancer is diagnosed and confined to the prostate, one of the primary treatment options is the complete removal of the prostate gland, along with surrounding tissues such as the seminal vesicles, and in some cases, nearby lymph nodes. This surgery is called a radical prostatectomy. The goal of the procedure is to remove the cancerous tissue, potentially providing a cure and preventing the spread of the disease to other parts of the body.
Radical prostatectomy has evolved significantly over the past several decades. Traditionally, this surgery was performed through an open incision, which required a large cut in the lower abdomen. However, with advancements in surgical technology, minimally invasive techniques such as laparoscopic surgery and robotic-assisted prostatectomy have become more common. These approaches offer several advantages over traditional open surgery, including smaller incisions, less blood loss, reduced pain, shorter hospital stays, and faster recovery times.
The procedure is typically recommended when prostate cancer is diagnosed early, confined to the prostate, and has a low likelihood of spreading. Radical prostatectomy is often considered the most effective treatment option for men with localized prostate cancer, as it provides the best chance for long-term survival. However, it is not suitable for all patients, and the decision to undergo the surgery depends on various factors, such as the stage and grade of cancer, the patient's overall health, and personal preferences.
Causes and Risk Factors for Radical Prostatectomy
Radical prostatectomy is performed primarily to treat prostate cancer, which is the most common cause for the surgery. Prostate cancer begins when cells in the prostate gland start growing uncontrollably, forming a tumor. Over time, this tumor may become large enough to spread outside of the prostate to nearby tissues or distant parts of the body.
There are several key risk factors that increase the likelihood of developing prostate cancer and, consequently, the need for a radical prostatectomy:
1. Age
Age is one of the strongest risk factors for prostate cancer. The risk of developing the disease increases significantly after the age of 50. Approximately 60% of prostate cancer cases occur in men over 65 years old.
2. Family History
Men with a family history of prostate cancer are at a higher risk. If a father or brother had prostate cancer, the risk doubles. The genetic factors contributing to prostate cancer risk are still being studied, but family history remains a key consideration in the risk assessment.
3. Race/Ethnicity
African American men have a higher incidence of prostate cancer and are more likely to develop aggressive forms of the disease. In contrast, Asian men tend to have lower rates of prostate cancer, although these rates have increased in recent years with changing lifestyle factors.
4. Genetic Factors
Certain genetic mutations, including those related to the BRCA1 and BRCA2 genes, can increase the risk of prostate cancer. Men with a history of breast cancer or ovarian cancer in their family may also be at higher risk due to these inherited mutations.
5. Diet and Lifestyle
A diet high in red meat, dairy products, and processed foods, combined with a lack of physical activity, may increase the risk of prostate cancer. Some studies suggest that obesity may be linked to more aggressive forms of prostate cancer.
6. Elevated PSA Levels
Men with high levels of prostate-specific antigen (PSA), a protein produced by the prostate, may be at higher risk for prostate cancer. PSA levels are commonly used as a screening tool to detect potential prostate issues, although elevated PSA levels can sometimes indicate benign prostate conditions.
7. Inflammation or Infection
Chronic inflammation or infections of the prostate, such as prostatitis, may increase the risk of developing prostate cancer. However, the relationship between inflammation and cancer development is complex and still under investigation.
8. Previous Prostate Conditions
Conditions like benign prostatic hyperplasia (BPH), where the prostate enlarges non-cancerously, or a history of high-grade prostatic intraepithelial neoplasia (PIN), a precancerous condition, may increase the risk of developing prostate cancer in the future.
Radical prostatectomy is typically recommended when prostate cancer is localized to the prostate, and the patient is in good overall health with a reasonable life expectancy. If the cancer has spread beyond the prostate, other treatment options such as radiation therapy, hormone therapy, or chemotherapy may be considered.
Symptoms and Signs Leading to Radical Prostatectomy
Prostate cancer is often asymptomatic in its early stages, which is why regular screening is crucial for early detection. When symptoms do occur, they can vary depending on the size of the tumor and whether it has spread to other parts of the body.
Early Symptoms
In many cases, early-stage prostate cancer does not cause noticeable symptoms. This is why screening methods such as the PSA test and digital rectal exam (DRE) are so important. However, in some instances, patients may notice subtle changes such as:
-
Frequent urination, especially at night (nocturia)
-
Weak or interrupted urine flow
-
Difficulty starting or stopping urination
-
Pain or burning sensation during urination
-
Blood in the urine or semen
-
Painful ejaculation
Advanced Symptoms
As the cancer grows or spreads, more severe symptoms may arise, including:
-
Severe pain in the lower back, hips, or thighs (if the cancer has spread to the bones)
-
Blood in the urine or semen becomes more noticeable
-
Unexplained weight loss or a loss of appetite
-
Fatigue, weakness, and generalized discomfort
-
Difficulty getting or maintaining an erection (erectile dysfunction)
Since many of these symptoms can also be caused by non-cancerous prostate conditions like benign prostatic hyperplasia (BPH), it is important to seek medical evaluation to determine the cause. If prostate cancer is suspected, additional diagnostic tests such as a biopsy or imaging studies are necessary to confirm the diagnosis and determine the extent of the disease.
Diagnosis of Prostate Cancer Leading to Radical Prostatectomy
The diagnosis of prostate cancer begins with a medical evaluation and continues with specific tests to confirm the presence of cancer and determine its stage. The key steps include:
1. PSA Testing
The PSA test measures the level of prostate-specific antigen in the blood. Elevated PSA levels can indicate the presence of prostate cancer, though they can also be elevated due to other conditions, such as prostatitis or BPH. A high PSA level often prompts further investigation.
2. Digital Rectal Exam (DRE)
During a DRE, a doctor inserts a gloved finger into the rectum to feel for abnormalities or hard lumps on the prostate. While DRE cannot definitively diagnose cancer, it can help identify suspicious areas that may warrant further testing.
3. Biopsy
If PSA levels are elevated or the DRE reveals abnormalities, a biopsy of the prostate is the next step. A biopsy involves taking small tissue samples from the prostate to examine for cancerous cells. This procedure is typically done under local anesthesia with a needle inserted through the rectum or perineum (the area between the scrotum and anus).
4. Imaging Tests
Imaging tests such as MRI, CT scans, or bone scans are used to assess the spread of cancer beyond the prostate. MRI helps visualize the prostate and surrounding tissues, while CT and bone scans are used to check for metastasis, especially in the lymph nodes or bones.
5. Gleason Score and Cancer Staging
Once cancer is confirmed, it is classified using the Gleason score, which grades the cancer based on how the cells look under a microscope. The score ranges from 2 to 10, with higher scores indicating more aggressive cancer. Staging is also determined based on the extent of the cancer, using the TNM system (Tumor, Node, Metastasis).
Once prostate cancer has been diagnosed and staged, the next step is to discuss treatment options. If the cancer is localized and the patient is deemed a good candidate for surgery, radical prostatectomy is often recommended as a treatment option.
Treatment Options for Radical Prostatectomy
Radical prostatectomy is often the first line of treatment for prostate cancer that is confined to the prostate gland. There are several approaches to this surgery, and the choice of technique depends on the individual patient's circumstances.
1. Open Radical Prostatectomy
In open radical prostatectomy, the surgeon makes a large incision in the lower abdomen to access the prostate gland. This traditional approach is effective but requires a longer recovery period, more blood loss, and a greater risk of complications compared to minimally invasive techniques.
2. Laparoscopic Radical Prostatectomy
Laparoscopic surgery involves making several small incisions through which instruments and a camera are inserted to perform the surgery. This approach offers smaller incisions, less pain, and faster recovery. However, it requires advanced surgical skill and experience.
3. Robotic-Assisted Radical Prostatectomy
Robot-assisted surgery is a minimally invasive approach that uses robotic arms controlled by the surgeon to remove the prostate gland. The robot provides enhanced precision and allows the surgeon to operate with more control, which is particularly beneficial in nerve-sparing procedures. This method reduces recovery time, minimizes blood loss, and often results in less postoperative pain.
4. Nerve-Sparing Prostatectomy
For men who wish to preserve erectile function, nerve-sparing prostatectomy may be performed when the cancer is confined to the prostate and does not involve the nerves that control sexual function. This technique aims to preserve the neurovascular bundles surrounding the prostate, which are responsible for erections.
5. Lymph Node Dissection
In some cases, the surgeon may also remove lymph nodes in the pelvic area during radical prostatectomy to check for cancer spread. If cancer has spread to the lymph nodes, additional treatments such as radiation therapy or hormone therapy may be necessary.
Prevention and Management Post-Surgery
Radical prostatectomy can offer a cure for localized prostate cancer, but prevention and proper management are essential for ensuring long-term health after the surgery.
1. Preventing Prostate Cancer
While there is no guaranteed way to prevent prostate cancer, certain lifestyle changes may reduce the risk. A healthy diet rich in fruits, vegetables, whole grains, and low in red meats can be beneficial. Regular physical activity, maintaining a healthy weight, and avoiding smoking can also contribute to prostate health.
2. Management After Surgery
After radical prostatectomy, patients are closely monitored to ensure the best outcomes. Regular follow-up visits include PSA testing to check for any recurrence of cancer. Most patients also experience some degree of urinary incontinence immediately after surgery, which typically improves with time and pelvic floor exercises. Some men may also experience erectile dysfunction, but various treatments, including medications and devices, can help.
Patients are encouraged to engage in pelvic floor exercises to strengthen the muscles responsible for urinary control and improve recovery. Physical activity and a balanced diet also play a role in speeding up the recovery process.
3. Ongoing Monitoring
Long-term follow-up care includes regular PSA tests to check for any recurrence of cancer. Additionally, men may undergo further imaging or biopsies if their PSA levels rise. It's important for patients to continue their surveillance regimen even after recovery from surgery to detect any potential issues early.
Complications of Radical Prostatectomy
Like any major surgery, radical prostatectomy carries risks. Some potential complications include:
1. Immediate Surgical Complications
-
Bleeding during or after surgery
-
Infection at the surgical site or urinary tract
-
Blood clots (deep vein thrombosis or pulmonary embolism)
-
Damage to surrounding organs such as the bladder or rectum
2. Functional Complications
-
Urinary incontinence, which can vary from mild dribbling to complete loss of control
-
Erectile dysfunction due to nerve damage, particularly if the neurovascular bundles are affected
-
Changes in orgasmic function, including dry orgasms due to the removal of seminal vesicles
3. Long-Term Complications
-
Urethral stricture (narrowing of the urethra), which can cause difficulty urinating
-
Lymphedema (swelling of the legs or pelvic area) if lymph nodes are removed
-
Recurrence of cancer, especially if some cancerous cells were left behind during surgery
Living with Radical Prostatectomy: Quality of Life
Life after radical prostatectomy can be fulfilling, though patients may need to adjust to changes in urinary and sexual function. Many men resume normal activities, including work and exercise, after they have fully recovered. Supportive care, including pelvic floor rehabilitation, erectile dysfunction treatments, and counseling, can help manage these changes.
While most patients regain control of their urinary function within six months to a year, some men may require additional treatment for incontinence. Erectile dysfunction is common, but various therapies, such as medications, pumps, and implants, can help restore sexual function.
Overall, the majority of men live long, healthy lives following radical prostatectomy, especially when the cancer is detected early, and the surgery is successful. Regular monitoring and maintaining a healthy lifestyle are crucial for long-term health and quality of life.
Top 10 Frequently Asked Questions about Radical Prostatectomy
1. What exactly is a radical prostatectomy?
A radical prostatectomy is a surgical procedure where the entire prostate gland, along with surrounding tissues such as the seminal vesicles, parts of the urethra, and occasionally pelvic lymph nodes, are removed. This surgery is primarily performed for patients diagnosed with prostate cancer that is confined to the prostate. The goal is to eliminate the cancer while offering the possibility of a cure. The procedure can be carried out through different methods: open surgery (involves a single large incision), laparoscopic surgery (multiple small incisions using specialized tools), or robot-assisted surgery (a type of laparoscopic surgery using robotic assistance to enhance precision). The choice of surgical method depends on the patient's health, tumor size, and location, as well as the surgeon's expertise.
2. Why and when is radical prostatectomy performed?
Radical prostatectomy is generally recommended when prostate cancer is localized, meaning it has not spread beyond the prostate gland. It is often suggested when the cancer is in its early stages, and the potential for a cure is high. Factors influencing the decision to proceed with surgery include the patient's age, general health, the aggressiveness of the cancer (how advanced it is), and the likelihood of success in preserving important functions like urinary control and sexual performance. The goal is to remove the tumor while maintaining the highest possible quality of life post-surgery. For men who are otherwise healthy and have a long life expectancy, this surgery offers the best chance of long-term cancer-free survival.
3. What types or surgical approaches are available for this procedure?
Radical prostatectomy can be performed using different approaches based on the patient's specific needs. The most common options include open surgery, which involves a single large incision, typically in the lower abdomen or between the scrotum and anus. This method is often used for larger tumors or when a surgeon feels it is necessary for better access to the prostate. Laparoscopic surgery is less invasive, using small incisions through which specialized instruments are inserted, including a camera to guide the procedure. This technique offers quicker recovery times and fewer complications. A more advanced version of laparoscopic surgery is robot-assisted prostatectomy, which uses robotic arms controlled by the surgeon, allowing for greater precision, enhanced visualization, and reduced blood loss. The choice of surgery depends on the tumor's characteristics, the surgeon's expertise, and the patient's health.
4. What are the major risks, side effects, and complications of radical prostatectomy?
Like any major surgery, radical prostatectomy carries risks such as bleeding, infection, and reactions to anesthesia. Specific to this procedure are risks related to the removal of the prostate and its proximity to important structures such as the bladder, nerves, and urethra. One of the most common complications is urinary incontinence, or the inability to fully control urination. This may improve over time, but some patients may experience ongoing issues. Erectile dysfunction is another potential complication, as the nerves responsible for erections are located near the prostate and can be damaged during surgery. Nerve-sparing techniques can help preserve erectile function, but success depends on tumor location and aggressiveness. In rare cases, scarring or narrowing of the urethra or bladder-neck can occur, which may require further surgical intervention.
5. How long is the recovery period, and what can I expect after surgery?
The recovery period for radical prostatectomy varies depending on the surgical approach used. If robotic or laparoscopic surgery is performed, most patients can expect to stay in the hospital for about one to two days and may be able to return to normal activities after a few weeks. However, for open surgery, the recovery period is generally longer, with patients often requiring a hospital stay of several days and needing more time to fully recover, sometimes up to 6 to 8 weeks. During recovery, patients will likely have a urinary catheter in place to help drain urine, which is typically removed within a week. Gradual improvements in mobility, energy levels, and overall well-being are expected, but patients should follow their doctor's recommendations regarding lifting, driving, and physical activity.
6. Will I be able to control urination normally and resume normal sexual activity?
Post-surgery, many men regain urinary control, but it may take some time. Immediately after surgery, urinary incontinence is common, with most patients experiencing mild leakage. Over time, especially with pelvic floor exercises, many regain full control, although some men may experience long-term incontinence issues. As for sexual function, radical prostatectomy can have a significant impact. If the surgery involves nerve-sparing techniques, there may be a better chance of preserving erectile function, but many men will experience some degree of erectile dysfunction post-surgery. Recovery of sexual function can take months, and for some, medications, devices, or other treatments may be necessary. It's important to have realistic expectations and discuss options for rehabilitation and support with your healthcare provider.
7. What happens to my PSA and what follow-up is needed after surgery?
After radical prostatectomy, the PSA (prostate-specific antigen) levels should drop to undetectable levels, as the prostate gland is removed. PSA levels are monitored regularly after surgery as an indicator of cancer recurrence. A rising PSA level after surgery can be an early sign that prostate cancer has returned. Typically, patients will have follow-up visits every 3-6 months during the first few years after surgery to monitor PSA levels, undergo imaging studies, and check for signs of cancer recurrence. If PSA levels remain low and stable, it is generally a good sign that the cancer has been effectively removed.
8. What lifestyle or dietary changes should I adopt after this surgery?
Adopting a healthy lifestyle after prostate surgery is crucial for overall recovery and long-term well-being. Patients are advised to maintain a balanced diet, emphasizing foods rich in fiber, vitamins, and antioxidants to support healing. Limiting red meat and processed foods while increasing intake of fruits, vegetables, and whole grains may help support prostate health. Regular exercise is also recommended to improve overall fitness and prevent weight gain, which can exacerbate certain health issues. Staying hydrated and avoiding smoking are important steps, as smoking can negatively affect recovery and overall prostate health. Patients should consult their doctors about specific dietary restrictions and exercise regimens post-surgery.
9. Will removing the prostate cure my cancer, or might I need other treatments?
Radical prostatectomy can be curative, especially for men whose cancer is detected early and confined to the prostate. However, for some men, the cancer may return even after surgery, particularly if there were certain high-risk features in the pathology, such as positive surgical margins, lymph node involvement, or a high-grade tumor. In these cases, additional treatments such as radiation therapy, hormone therapy, or chemotherapy may be necessary to manage the cancer. After surgery, regular follow-up visits and PSA tests are essential to monitor for any signs of recurrence, and additional treatments may be initiated if needed.
10. How do I choose the right surgeon, and what questions should I ask before surgery?
Choosing the right surgeon for radical prostatectomy is critical to ensuring the best outcomes. It's important to consider the surgeon's experience with prostate surgeries, particularly the technique you are opting for (robotic, laparoscopic, or open). You should inquire about their specific experience in performing radical prostatectomy and the success rates in terms of cancer control, urinary function, and sexual health. Questions to ask include:
-
What approach do you recommend for me and why?
-
What is your experience with nerve-sparing techniques, and what are the chances of preserving sexual and urinary function?
-
What are the risks of complications like erectile dysfunction or incontinence, and how often do these occur in your patients?
-
What does the recovery process look like, and when can I resume normal activities?
Being well-informed and actively participating in decision-making can help ensure the best outcome for your treatment and quality of life.


