Introduction to Radio-Surgical Treatment of Spinal Tumors
Radio-surgical treatment, particularly stereotactic radiosurgery (SRS) and stereotactic body radiotherapy (SBRT), has become a groundbreaking method for treating spinal tumors. Unlike traditional surgery, which involves cutting into the body, radio-surgery uses high doses of precisely targeted radiation to treat tumors with minimal disruption to surrounding tissues. This approach is non-invasive, allowing patients to avoid the risks associated with open surgery, such as infection, blood loss, and long recovery times. Radio-surgery is particularly beneficial for spinal tumors, which often occur near critical structures like the spinal cord and nerves, making traditional surgery risky or impractical.
The procedure works by delivering highly focused beams of radiation to the tumor site from multiple angles. The beams converge precisely at the tumor, delivering a high dose of radiation in a few sessions-usually one to five-depending on the tumor's size and location. Radio-surgical techniques can be employed to treat both primary spinal tumors (tumors that originate in the spine) and metastatic spinal tumors (tumors that spread to the spine from other parts of the body).
The main advantages of radio-surgical treatment include its ability to target the tumor precisely, minimizing the risk of harming surrounding tissues such as the spinal cord. It also offers a quicker recovery time compared to traditional surgery, with many patients returning to their daily activities within a few days. Moreover, it is an option for patients who may not be candidates for surgery due to medical conditions or the location of the tumor. In this guide, we will delve deeper into the causes of spinal tumors, their symptoms, the diagnostic process, treatment options, management strategies, potential complications, and the impact on a patient's quality of life after treatment.
Causes and Risk Factors for Spinal Tumors Treated by Radio-Surgery
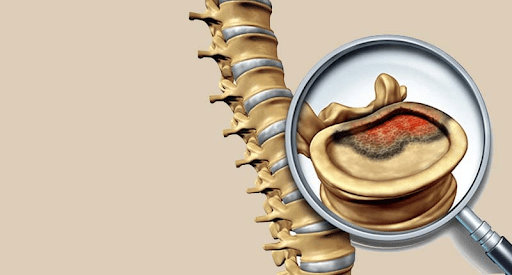
Spinal tumors can be categorized into primary and metastatic tumors, and understanding the causes and risk factors is critical in determining appropriate treatment options, including radio-surgery. The causes of spinal tumors are diverse, with some originating in the spine itself and others spreading from other areas of the body.
Primary Spinal Tumors
Primary spinal tumors originate within the spinal cord or the surrounding structures, such as the bones, nerves, or membranes covering the spine. These tumors are much rarer than metastatic tumors. Some common types of primary spinal tumors include:
-
Meningiomas: Tumors that develop from the meninges, the membranes that cover the brain and spinal cord.
-
Schwannomas: Tumors that arise from Schwann cells, which form the protective sheath around nerves.
-
Neurofibromas: Benign tumors that also form on the nerve sheath but are associated with neurofibromatosis, a genetic disorder.
-
Ependymomas: Tumors that arise from the ependymal cells lining the spinal cord's central canal.
-
Osteosarcomas: Primary bone tumors that can occur in the vertebrae.
While the exact cause of these tumors is often unknown, genetic factors, family history, and certain environmental exposures can increase the risk of developing these tumors. For example, people with neurofibromatosis type 2 have a higher risk of developing spinal schwannomas and meningiomas.
Metastatic Spinal Tumors
Metastatic spinal tumors are far more common than primary spinal tumors and occur when cancer cells from other parts of the body spread to the spine. These tumors typically arise from cancers of the lung, breast, prostate, kidney, and gastrointestinal tract, and often affect the spine due to its proximity to major blood vessels, which facilitate the spread of cancer cells. Some of the most common types of metastatic spinal tumors include:
-
Breast Cancer: One of the most common sources of metastasis to the spine.
-
Prostate Cancer: Prostate cancer often spreads to the bones, particularly the spine, causing significant pain and neurological complications.
-
Lung Cancer: Often spreads to the spine through blood vessels and lymphatics.
-
Renal Cell Carcinoma (Kidney Cancer): Known for its tendency to spread to the spine.
Certain risk factors increase the likelihood of developing metastatic spinal tumors, including:
-
Advanced age: As individuals age, the likelihood of cancer spreading to the spine increases.
-
Previous cancer diagnosis: Patients with a history of cancer, particularly cancers known to metastasize to bone (like breast, prostate, and lung cancers), are at a higher risk.
-
Chronic diseases and weakened immune systems: Conditions that impair immune function, such as HIV/AIDS, increase the risk of metastatic tumors.
Other Risk Factors
-
Family history and genetics: Some genetic conditions, like neurofibromatosis, increase the risk of developing certain spinal tumors.
-
Radiation exposure: Previous radiation treatment to the spine or surrounding areas can increase the risk of developing secondary cancers.
Symptoms and Signs of Spinal Tumors Leading to Radio-Surgical Treatment
Spinal tumors, whether primary or metastatic, can cause a range of symptoms depending on their size, location, and the structures they affect. Symptoms often develop gradually, making it important for individuals to seek medical attention if they experience persistent or worsening neurological symptoms.
Common Symptoms
-
Back pain: The most common symptom of spinal tumors is localized back pain. The pain may be constant or worsen at night and may not respond well to over-the-counter pain medications.
-
Radiculopathy: Pain, tingling, or numbness that radiates along the path of a nerve. This is often due to a tumor pressing on a nerve root.
-
Weakness or loss of coordination: Tumors in or near the spinal cord can cause weakness in the limbs, affecting the ability to walk, balance, or perform daily activities.
-
Bladder or bowel dysfunction: In more advanced cases, when tumors compress the spinal cord or nerves, patients may experience incontinence, retention, or difficulty controlling their bowel or bladder.
-
Sensory changes: Loss of sensation or tingling in the arms, legs, or torso due to pressure on the spinal cord or nerves.
-
Spinal deformities: As tumors grow, they can cause structural damage to the spine, leading to deformities such as scoliosis or kyphosis.
Metastatic Tumor Symptoms
In the case of metastatic spinal tumors, symptoms often manifest after the primary cancer has been diagnosed, although in some cases, spinal involvement may be the first sign. Symptoms in metastatic spinal disease are often more severe and may include:
-
Severe, persistent pain that is often described as aching, stabbing, or burning.
-
Neurological deficits, such as weakness, numbness, or loss of reflexes.
-
Spinal cord compression: A medical emergency characterized by the sudden onset of weakness, numbness, or paralysis. Compression of the spinal cord due to a tumor can lead to permanent neurological damage if not treated promptly.
If you experience any of these symptoms, particularly if you have a history of cancer, it's crucial to seek medical attention promptly. Early diagnosis can help prevent irreversible nerve damage and provide treatment options that preserve function.
Diagnosis of Spinal Tumors and Suitability for Radio-Surgical Treatment
Diagnosing spinal tumors typically involves a combination of clinical evaluation, imaging, and biopsy. Accurate diagnosis is crucial for determining the most effective treatment options, including whether radio-surgical treatment is appropriate.
Clinical Evaluation
The first step in diagnosis is a thorough medical history and physical examination. Doctors will ask about symptoms, pain patterns, family history, and any previous cancer diagnoses. A neurological exam will assess motor function, reflexes, sensation, and coordination to help determine the extent of spinal cord involvement.
Imaging Tests
Imaging is critical for visualizing the tumor, assessing its size, and evaluating its relationship with surrounding structures:
-
MRI (Magnetic Resonance Imaging): The most effective imaging method for detecting spinal tumors, especially for viewing soft tissue and spinal cord involvement. It helps in determining the location and size of the tumor.
-
CT scan (Computed Tomography): CT scans are especially useful in visualizing bony structures and detecting any destruction caused by tumors.
-
Bone Scintigraphy (Bone Scan): Often used to detect metastatic disease spread to the bones, including the spine.
-
PET/CT scans: In cases of metastatic cancer, PET/CT scans are helpful in detecting active cancerous lesions throughout the body.
Biopsy
If the imaging results suggest a tumor, a biopsy is often needed to confirm the diagnosis and determine the tumor's type (benign vs. malignant). A biopsy involves removing a small tissue sample from the tumor for microscopic examination. This procedure can be performed using a needle (for a needle biopsy) or during surgery if necessary.
Suitability for Radio-Surgical Treatment
Not all spinal tumors are suitable for radio-surgery. The decision to use radio-surgery depends on several factors:
-
Tumor size: Radio-surgery is most effective for small to moderate-sized tumors.
-
Location: Tumors close to the spinal cord may require more precise targeting to avoid damaging healthy tissue.
-
Spinal stability: Tumors that cause significant structural damage to the spine may require surgical stabilization in addition to radio-surgery.
-
Health status: Patients who are medically unfit for open surgery or those who have recurrent tumors may be better candidates for radio-surgery.
After the diagnosis is confirmed, the treatment plan is designed based on the tumor's characteristics and the patient's overall health.
Treatment Options for Spinal Tumors: Focus on Radio-Surgical Treatment
Radio-surgery, specifically stereotactic radiosurgery (SRS) or stereotactic body radiotherapy (SBRT), has proven to be an effective treatment for spinal tumors. This treatment uses high doses of radiation delivered with pinpoint accuracy to treat tumors in the spine, sparing surrounding tissues, including the spinal cord, nerves, and blood vessels.
How Radio-Surgery Works
In radio-surgery, multiple beams of radiation are directed at the tumor from various angles. The radiation is carefully calibrated to converge at the tumor site, allowing for a high dose of radiation to be delivered to the tumor while minimizing exposure to healthy tissues. The treatment is usually delivered in one to five sessions, making it a relatively quick treatment option compared to traditional radiation therapy, which may require daily sessions for several weeks.
Benefits of Radio-Surgery:
-
Precision: Radio-surgery delivers high-dose radiation directly to the tumor with minimal exposure to surrounding healthy tissue.
-
Non-invasive: No need for incisions or hospitalization, leading to a faster recovery.
-
Effective: Studies have shown that radio-surgery can achieve excellent tumor control, especially for metastatic spinal tumors.
-
Pain relief: It is highly effective in managing pain associated with spinal tumors, often providing rapid relief.
Combination with Surgery
In some cases, radio-surgery may be used in conjunction with surgical procedures. For example, a patient may undergo surgery to remove a portion of a spinal tumor, followed by radio-surgery to treat any remaining tumor tissue. This combination approach is often used when tumors are large or located near critical structures.
Indications for Radio-Surgery
Radio-surgery is often the preferred treatment for:
-
Small to moderate-sized spinal tumors
-
Metastatic spinal lesions in patients who are not candidates for open surgery
-
Tumors that are not easily accessible through traditional surgery
-
Relapsed tumors after previous surgical or radiotherapy treatment
-
Tumors causing pain or neurological symptoms, especially when surgery poses significant risks
Prevention and Management of Spinal Tumors Treated by Radio-Surgery
Prevention of Spinal Tumors
While preventing spinal tumors, particularly metastatic tumors, is difficult, regular screening for high-risk individuals (such as those with a history of cancer) can help detect tumors early. Lifestyle modifications, such as a healthy diet, regular exercise, and avoiding smoking, can contribute to overall health and reduce the risk of certain cancers.
Management Before, During, and After Treatment
-
Before Treatment: Managing symptoms such as pain, mobility issues, and neurological deficits is crucial. Preparing the patient mentally for radio-surgical treatment is also important, as some patients may experience anxiety about the procedure.
-
During Treatment: Ensuring proper immobilization during radio-surgery to prevent movement and ensure precise radiation delivery is essential. Patients should also be monitored for side effects.
-
After Treatment: Follow-up care includes imaging to assess tumor response, monitoring for complications, managing pain, and addressing any functional impairments. Patients may need physical therapy to recover mobility and strength.
Complications of Radio-Surgical Treatment of Spinal Tumors
Though radio-surgery is generally well-tolerated, there are potential risks and complications associated with this treatment. These include:
-
Radiation-induced myelopathy: Damage to the spinal cord, although rare, can occur if the radiation dose is too high.
-
Vertebral fractures: The radiation may weaken bones, leading to fractures, particularly in patients with metastases.
-
Neurological deterioration: If radiation impacts surrounding nerve tissue, it may cause new neurological symptoms such as numbness or weakness.
Living with Spinal Tumors Treated by Radio-Surgery
After receiving radio-surgical treatment, many patients experience a significant improvement in pain and neurological function. However, living with spinal tumors, even after treatment, requires ongoing monitoring and support:
-
Physical rehabilitation: Essential for restoring mobility, improving strength, and preventing deconditioning.
-
Psychological support: Coping with the emotional impact of cancer and its treatment, including the effects on body image, relationships, and long-term quality of life.
-
Long-term monitoring: Ongoing imaging and clinical evaluations to ensure the tumor does not recur or cause additional complications.
-
Lifestyle adjustments: Avoiding high-impact activities, managing bone health, and maintaining a healthy diet and exercise regimen are important for long-term well-being.
Top 10 Frequently Asked Questions about Radio-Surgical Treatment of Spinal Tumors
1. What is radio-surgical treatment of spinal tumors?
Radio-surgical treatment (often called stereotactic radiosurgery or spine radiosurgery) is a non-invasive therapy in which highly focused, high-dose radiation beams are delivered precisely to a tumour in or around the spine, with the goal of destroying tumour cells or stopping tumour growth while minimising damage to the surrounding spinal cord, nerves and healthy tissue. It differs from conventional radiotherapy in having far greater precision, higher dose per session, fewer treatment sessions, and a steeper drop-off of radiation beyond the target area. In the spine setting, this technology is increasingly used both for primary spinal tumours and metastases.
2. When is spinal radiosurgery used instead of or in addition to surgery?
Spinal radiosurgery may be chosen when a tumour is not safe or feasible to remove surgically (for example because of its location near critical neurological structures), when the patient may not tolerate open surgery due to general health, or when the tumour has recurred after previous surgery or radiation. It may also be used after surgery to treat residual tumour tissue or as part of a combined treatment strategy. The decision is made by a multidisciplinary team (neurosurgeon, radiation oncologist, medical physicist) assessing tumour size, location, previous treatment history, and patient health.
3. What are the benefits of spinal radiosurgery compared to conventional treatments?
The major advantages include:
-
No large incision - it's non-surgical or minimally invasive in nature, which means less risk of surgical bleeding, infection, or long hospital stays.
-
Fewer treatment sessions - some treatments can be done in a single session or just a few sessions rather than many weeks of daily treatment.
-
High precision - radiation is narrowly focused on the tumour with a sharp fall-off to spare healthy spinal cord and tissues, which is critical in spinal applications.
-
Good local tumour control and pain relief outcomes in many cases-studies show high rates of tumour stability or shrinkage and relief of symptoms.
4. What are the potential risks or side-effects of spinal radiosurgery?
While spinal radiosurgery is generally well tolerated, there are risks and possible side‐effects, which may include:
-
Fatigue in the days following treatment.
-
Local swelling or inflammation around the tumour site which may transiently increase pain or neurological symptoms.
-
Skin irritation (if beam passes through skin), or mild transient numbness/tingling in nearby nerves.
-
Rare but more serious risks: radiation injury to the spinal cord or nerves (leading to weakness or sensory loss), or damage to adjacent organs or vertebrae. Because of the critical anatomy of the spine, careful dose planning is essential.
These risks are typically lower than with open surgery, but they still require discussion and monitoring.
5. How long does the treatment and recovery take?
Treatment itself is relatively short - often a single session lasting 1-2 hours, or a small number (2-5) of sessions over one to two weeks. Because the procedure doesn't require large incisions, most patients are treated as outpatients (or with a short stay) and return to many activities quickly. The actual recovery timeline depends on your tumour, your general health, and whether you had other treatments (surgery, chemotherapy) at the same time. Some mild symptoms (fatigue, soreness) may persist for a few days to weeks, but many people resume near-normal activities soon after.
6. What outcomes can patients expect-does it cure the tumour?
Outcomes depend heavily on tumour type (benign vs malignant), size, location, whether it has spread, and whether it has previously been treated. Many studies show excellent local control (i.e., the treated tumour remains stable or shrinks) rates-some in the 80-90 % range in select cases. However, "cure" may not be guaranteed-especially for metastatic disease. The aim may be symptom relief (pain, neurological symptoms), preventing progression, and maintaining quality of life rather than cure in all cases. The treatment is most effective when used as part of a comprehensive, multidisciplinary plan.
7. How is patient eligibility determined for spinal radiosurgery?
Eligibility involves evaluation of multiple factors:
-
Location of tumour (how close to spinal cord, nerves, vertebrae, vital organs)
-
Size and volume of tumour
-
Whether the tumour is primary or metastatic, benign or malignant
-
Whether previous radiotherapy or surgery has been done (which may limit further radiation options)
-
The patient's general health, ability to lie still for treatment, and whether there are other medical issues
-
Whether open surgery is possible or risky
The multidisciplinary team will review imaging (MRI/CT), medical history, and prior treatments to decide whether radiosurgery is appropriate or if another approach is preferable.
8. What should a patient expect during treatment planning and preparation?
Before treatment, you will undergo detailed imaging studies (MRI, CT) to define exactly where the tumour is and how it relates to surrounding structures. You'll meet your care team (radiation oncologist, neurosurgeon, medical physicist) who will explain the procedure, risks, expected outcomes, and after-care. Special measures may be taken to immobilise you during treatment so that the high-dose beams hit precisely the tumour and minimise movement. Sometimes fiducial markers or custom molds may be used. You may be advised to stop certain medications (e.g., blood thinners) or prepare in other specific ways. Overall, preparation ensures that the treatment is as safe and accurate as possible.
9. What follow-up care and monitoring is required after radiosurgery?
After treatment, you'll have scheduled follow-up appointments with your team to monitor how the tumour responds, check for side-effects, and ensure ongoing spinal health. This typically involves periodic imaging (MRI or CT) to assess tumour size and status, and clinical evaluation of symptoms (pain, neurological signs). You may also have follow-up with your neurosurgeon or radiation oncologist. Because radiation effects can evolve over time, long-term monitoring is important-especially if you had prior treatments, or the tumour was malignant. You should report any new or worsening symptoms (such as pain, numbness, weakness) promptly.
10. What lifestyle or activity limitations should I follow after the treatment?
Because spinal radiosurgery is less invasive, in many cases patients can resume normal activities relatively quickly-but there may be some temporary restrictions depending on tumour location and other treatments received. Your doctor may advise avoiding heavy lifting or strenuous spine-stress activities for a period, until the initial healing is complete and your spine is stable. You may be asked to maintain good bone health (calcium intake, vitamin D, physical activity as tolerated), and to avoid smoking or other behaviours that impair healing or bone integrity. Pain management, physical therapy or spine-rehabilitation may be part of recovery. Maintaining overall healthy habits (nutrition, exercise, monitoring underlying conditions) supports the best outcomes.


