Introduction to Reversal of Sterilization
Sterilization is one of the most widely used permanent contraceptive methods, chosen by many individuals or couples who have completed their family planning goals. The two most common forms of sterilization are tubal ligation (for women) and vasectomy (for men). Both procedures are considered permanent, meaning they are designed to prevent future pregnancies by blocking or severing the pathways used for sperm or egg transport. However, life circumstances can change, and some individuals or couples may later decide that they want to conceive again.
In such cases, the reversal of sterilization provides an option for restoring fertility. Tubal reversal involves reconnecting or repairing the fallopian tubes, while vasectomy reversal involves reconnecting the vas deferens. While these procedures offer hope for those wishing to conceive after sterilization, it's important to understand that the success of sterilization reversal depends on a variety of factors, including the time elapsed since the original sterilization, the patient's age, the quality of the reproductive organs, and whether other fertility issues are present.
This article will delve into the causes and motivations behind seeking a sterilization reversal, explore the associated risks and benefits, examine the various diagnostic methods used to assess eligibility for reversal surgery, and provide insights into the different treatment options available. Understanding all these aspects is crucial for those considering sterilization reversal and for helping them make an informed decision.
Causes and Risk Factors of Reversal of Sterilization
People may choose to undergo sterilization reversal for various reasons. Some of the most common causes include:
Motivations for Seeking Reversal:
-
Regret or Change in Life Circumstances: One of the most significant motivations for sterilization reversal is regret. Individuals or couples may have chosen sterilization at a younger age, only to later find themselves desiring more children. Changes in life circumstances such as the loss of a child, remarriage, or simply a change of heart regarding having more children can prompt individuals to seek reversal.
-
Health or Relationship Changes: Other reasons for reversal include health improvements, changes in fertility, or shifts in a person's relationship status. For instance, a woman might seek a reversal after remarrying and wanting to have children with her new partner. Alternatively, some men might decide they want more children after their initial sterilization if their partner has a health condition or an inability to conceive naturally.
-
Technological Advances: As medical technology improves, there is greater success in surgical reversals of sterilization, particularly in male vasectomy reversals. Advances in microsurgery have made the procedure more accessible and effective, encouraging more individuals to consider this option.
-
Emotional or Psychological Factors: After years of living without the option to have biological children, some individuals or couples may feel emotionally unfulfilled and decide to attempt a reversal in hopes of restoring their fertility. Psychological factors can weigh heavily in these decisions, especially when the desire to grow one's family is deeply rooted in a person's personal identity or life goals.
Risk Factors Affecting Success of Reversal:
The success of sterilization reversal is influenced by several factors, which can increase the complexity of the procedure:
-
Age of the Patient: Age plays a crucial role in the success of sterilization reversal. For women, fertility naturally declines with age, and older women may experience lower success rates after tubal reversal. In men, age also affects sperm quality, with a decline in sperm motility and count as they get older.
-
Time Since Sterilization: The longer it has been since the sterilization procedure, the lower the chances of success. This is particularly relevant in the case of vasectomy reversal, where prolonged blockage of the vas deferens can lead to sperm damage. Women who undergo tubal ligation and then seek reversal many years later may have less favorable results due to the scar tissue that can develop over time.
-
Method of Sterilization: The method used for sterilization will also influence the reversal process. For example, tubal ligation methods involving cutting or cauterizing the fallopian tubes are more difficult to reverse than methods where the tubes were merely tied or clipped. In men, the type of vasectomy (whether a vasovasostomy or vasoepididymostomy is required) depends on how long the obstruction has been in place and the quality of the vas deferens and epididymis.
-
Health and Fertility of the Partner: While sterilization reversal may restore anatomical fertility, the overall success of conception depends on the fertility of both partners. If the female partner has diminished ovarian reserve, if the male partner has low sperm count or poor sperm quality, or if there are other health issues at play, achieving a pregnancy may still be difficult, even after reversal.
-
Surgical and Anatomical Factors: The condition of the reproductive organs also plays a role in the success of reversal. In women, the presence of adhesions, previous tubal damage, or other internal factors such as endometriosis can reduce the success rates of tubal reversal. For men, an epididymal blockage or poor vas deferens quality can complicate the procedure.
Understanding these causes and risk factors allows patients to have realistic expectations regarding the potential success of sterilization reversal and prepares them for what might lie ahead.
Symptoms and Signs of Reversal of Sterilization
While the decision to undergo sterilization reversal is typically based on personal motivations, certain symptoms and signs might indicate the appropriateness or feasibility of a reversal. These may be related to the desire to have children after sterilization or the presence of specific complications that would require medical intervention.
Key Symptoms and Signs:
-
Desire to Conceive Again: The most obvious "symptom" prompting individuals to consider reversal is the desire to have children after previously opting for sterilization. This change in personal circumstances, often due to new relationships, changes in family structure, or loss of a child, can drive the decision to undergo a reversal procedure.
-
Signs of Fertility Issues: A woman who has undergone tubal ligation may not be aware of the condition of her fallopian tubes until she attempts to conceive. If natural conception does not occur after an adequate period of time trying, it may indicate a blockage or scarring in the tubes that necessitates reversal. Similarly, men who undergo vasectomy reversal may notice a failure to restore sperm flow, which could indicate that further surgical intervention is required.
-
Increased Desire to Have Biological Children: In some cases, individuals or couples may have initially chosen sterilization and now regret their decision because of an increased desire for biological children. This emotional and psychological "symptom" may prompt a re-evaluation of their fertility options and lead to considering a reversal procedure.
-
Partner Fertility Issues: If a couple is having difficulty conceiving and the female partner's reproductive organs are in good health, the male partner may consider vasectomy reversal as a possible solution. For women, if tubal ligation has led to infertility or other complications, they may opt for a tubal reversal to restore their ability to conceive naturally.
When to Seek Medical Evaluation:
Individuals should consider consulting a fertility specialist or an experienced surgeon to assess whether sterilization reversal is an option. If there are indications that natural conception is not happening or if the woman is in her late thirties or early forties, surgical intervention may be less likely to succeed. In men, sperm quality and the time since the vasectomy will need to be evaluated to determine the best approach for reversal.
Diagnosis of Reversal of Sterilization
Before considering surgical intervention, patients must undergo a thorough diagnostic evaluation to determine whether reversal is a viable option. This assessment includes both medical and reproductive evaluations to understand the underlying fertility factors and ensure the best chance for success.
Diagnostic Steps:
-
Detailed Medical History: The first step in diagnosis is understanding the reasons behind the request for sterilization reversal. This includes reviewing the initial sterilization method, the patient's health history, and any fertility issues that may have been present before or after the procedure. Understanding both the patient's and the partner's health history is crucial in making an informed decision.
-
Physical Examination: For women, a pelvic exam may be conducted to evaluate the health of the uterus and ovaries. An ultrasound may also be performed to assess the condition of the fallopian tubes. In men, a physical exam will focus on examining the scrotum and testes, looking for signs of any other conditions that might affect fertility.
-
Imaging and Tests:
-
For women: Hysterosalpingography (HSG) is commonly used to assess the condition of the fallopian tubes. This involves injecting a contrast dye into the uterus and fallopian tubes while taking X-rays.
-
For men: A semen analysis will be performed to determine sperm count and motility. This is critical because sperm quality is a determining factor in whether a successful pregnancy can be achieved after vasectomy reversal.
-
-
Partner Fertility Assessment: In many cases, fertility issues may lie with the partner rather than the patient who underwent sterilization. Assessing both partners' fertility is crucial in determining whether surgical reversal alone will suffice or if other fertility treatments, like IVF or ICSI, might be necessary.
-
Decision-Making Discussion: After the evaluations, patients will meet with their surgeon to discuss the findings and decide whether reversal is the most appropriate course of action. They will be informed about the likelihood of success, potential complications, and alternative fertility methods if reversal is not recommended or feasible.
By thoroughly assessing all factors, the physician can help guide the patient toward the best course of action.
Treatment Options of Reversal of Sterilization
Sterilization reversal surgery varies by gender and method of original sterilization. The following sections detail the two primary methods used to reverse sterilization: tubal ligation reversal for women and vasectomy reversal for men.
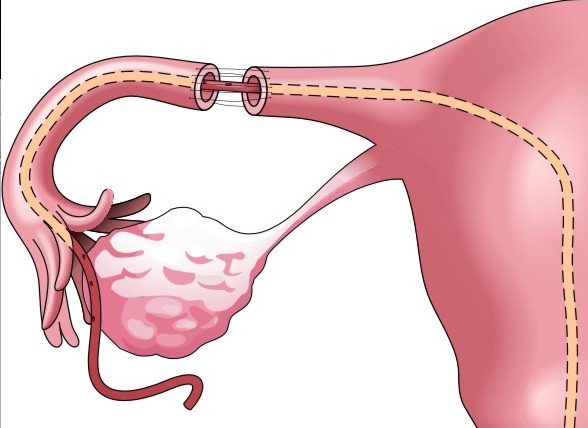
Tubal Ligation Reversal (Female)
The tubal ligation reversal procedure involves reconnecting or repairing the fallopian tubes that were blocked, cut, or cauterized during the original sterilization procedure. The goal is to restore the normal pathway for the egg to travel from the ovaries to the uterus. The procedure involves the following steps:
-
Microsurgical Technique: A skilled microsurgeon will use specialized instruments under magnification to carefully reconnect the remaining parts of the fallopian tubes. This ensures minimal tissue damage and the best possible chance of restoring fertility.
-
Success Factors: The success of the surgery depends on the length of the remaining tube, the condition of the tubes, and the woman's age and overall fertility health. If significant damage has occurred or if only a short segment of the tube remains, the chance of success may be lower.
Vasectomy Reversal (Male)
Vasectomy reversal involves reconnecting the vas deferens, the tube that carries sperm from the testes to the urethra. The procedure can be done in two ways:
-
Vasovasostomy: This procedure reconnects the two ends of the vas deferens directly. It is typically done when the blockage is near the testicle and the vas deferens is intact.
-
Vasoepididymostomy: This is a more complex procedure where the vas deferens is connected to the epididymis (the small tube that stores sperm). This method is necessary when there is a blockage higher up in the vas deferens or epididymis.
Both procedures require microsurgery and a high level of surgical expertise, with success rates varying depending on the length of time since the original vasectomy and the quality of sperm flow.
Prevention and Management of Reversal of Sterilization
Pre-operative Care:
Before undergoing sterilization reversal, patients should optimize their health by managing any pre-existing conditions (e.g., diabetes, hypertension), maintaining a healthy weight, quitting smoking, and ensuring that their reproductive health is in good condition. This includes addressing any hormonal imbalances or menstrual cycle issues for women and ensuring sperm health for men.
Post-operative Management:
After surgery, patients will need time to recover. For women, this may involve several weeks of rest, avoiding strenuous physical activity, and avoiding infection or injury. For men, the post-operative period may involve avoiding sexual activity for a few weeks to allow the vas deferens to heal properly. Regular follow-up visits are required to ensure the recovery is progressing smoothly, monitor fertility potential, and determine the next steps.
Complications of Reversal of Sterilization
Like any surgery, sterilization reversal carries some risks and potential complications. These can vary based on the patient's health, the surgical method used, and the complexity of the procedure. Some potential complications include:
-
Infection: As with any surgery, there is a risk of infection at the incision site.
-
Scarring: Excessive scar tissue may form in the reproductive organs, especially if the original sterilization procedure was more invasive.
-
Ectopic Pregnancy: Women who undergo tubal reversal have an increased risk of ectopic pregnancy, as the repaired fallopian tubes may not allow the egg to travel to the uterus normally.
-
Failure to Restore Fertility: Even after a successful reversal, fertility restoration may not be guaranteed, and couples may still need to pursue alternative fertility treatments.
Living with the Condition of Reversal of Sterilization
Post-operative care is an essential part of living with the outcome of sterilization reversal. Both physical and emotional recovery are important components of this process.
-
Physical Recovery: Most patients can return to normal activities within a few weeks, but it is essential to avoid any strenuous activities and heavy lifting for several weeks to ensure proper healing. Pain management and follow-up care are important to monitor any complications.
-
Fertility Journey: For women, the decision to attempt conception post-reversal can be an emotional journey, particularly if there are concerns about age, the quality of the fallopian tubes, or the length of time since sterilization. For men, the return of sperm post-reversal is a key milestone, though this does not guarantee pregnancy.
-
Support Systems: Emotional and psychological support is key, especially if the reversal does not result in pregnancy. Many individuals or couples may turn to counseling or fertility specialists to help them through this challenging process.
Top 10 Frequently Asked Questions about Reversal of Sterilization
1. What does reversal of sterilization mean?
Reversal of sterilization refers to a surgical procedure aimed at undoing a previous permanent contraceptive method—most commonly in women this means a Tubal Ligation Reversal (re-connecting or reopening the fallopian tubes) and in men a Vasectomy Reversal (re-joining the vas deferens). The goal is to restore fertility so that natural conception becomes possible again. It is important to understand that the procedure does not guarantee pregnancy, but offers a path for people who have changed their mind about having children.
2. Am I a good candidate for sterilization reversal?
Several factors determine whether you are a suitable candidate for reversal of sterilization. These include your age (fertility naturally declines with age), the condition and length of the remaining reproductive tubes (for women), the type of original sterilization method used, presence of other fertility issues (in you or your partner), and your overall health. For example, if a large portion of the fallopian tube has been removed, or if there is significant scarring, the chances of success may be lower. A careful evaluation by a fertility or surgical specialist will help assess the likelihood of success.
3. What does the procedure involve and what types are there?
For women, tubal sterilization reversal surgery involves reopening, re-connecting or reconstructing the fallopian tubes to allow eggs and sperm to meet and natural conception to occur. This may involve microsurgical techniques, laparoscopy or open surgery depending on circumstances. For men, vasectomy reversal involves reconnecting the cut ends of the vas deferens so that sperm can again pass into the ejaculate. Both procedures are more complex than the original sterilization operation and require specialist surgical skill and post-operative care.
4. What is the success rate and what factors influence it?
Success is usually measured in terms of achieving pregnancy rather than simply tube patency or duct re-connection. The success rate depends strongly on several factors: age (younger patients typically have higher rates), the remaining length and health of the tubes (in women), the surgical technique used, fertility status of the partner, and absence of other fertility-limiting conditions. In some centers for women, pregnancy rates after reversal are cited in the range of 50-80% in well-selected cases. However, success is not guaranteed, and outcomes vary.
5. What are the risks and possible complications of the reversal surgery?
As with any surgery, there are risks such as infection, bleeding, damage to nearby organs, reactions to anaesthesia and scar tissue formation. Specific to sterilisation reversal, there is an increased risk of ectopic pregnancy (where the embryo implants outside the uterus, typically in the tube) because the repaired tubes may have areas of narrowed or less-functioning segments. There is also the possibility that the tubes or ducts fail again, and natural conception may still not occur, requiring alternative fertility treatment. Patients and couples should discuss these risks in detail with their surgeon.
6. How long is the recovery period and when can I try to conceive afterwards?
Recovery time for reversal surgery varies depending on the procedure, technique used and the patient's health. Many women undergoing tubal reversal are able to resume normal light activities within 1-2 weeks, but full internal healing, optimal function and monitoring may take several months. Couples are often advised to wait a certain number of menstrual cycles before actively trying to conceive (for example 2-3 months) to allow healing and reduce the risk of complications such as ectopic pregnancy. The surgeon will provide guidance on when it is safe to start trying.
7. Is reversal of sterilisation the only option to try for conception after a sterilisation?
No. While reversal is one option, other fertility pathways exist depending on your context. For women with damaged or missing tubes, or when reversal is unlikely to succeed, in vitro fertilization (IVF) may be recommended. IVF bypasses the fallopian tubes by retrieving eggs, fertilising them in the lab, and transferring embryos to the uterus. Couples should discuss with their fertility specialist whether reversal or IVF (or sometimes both) is the best strategy given time, cost, desire for multiple children, and other fertility factors.
8. Will the reversal only allow one pregnancy, or can I have more children after it?
In many cases, once the sterilisation reversal is successful and fertility is restored, conception becomes possible similarly to a never-sterilised person (subject to age/fertility factors). This means you may have the potential for more than one pregnancy after a successful reversal. However, the surgical success, health of the reproductive organs, and general fertility status will influence how many children you can have and how quickly. Surgeons will often advise about optimal timing and the likelihood of multiple pregnancies based on your individual profile.
9. How much does reversal of sterilization cost and is it covered by insurance?
Cost varies widely depending on location, facility, technique (microsurgery, laparoscopy, etc.), and whether there are additional fertility evaluations or treatments needed. Some insurance plans may cover part of the evaluation or the surgery, but many consider sterilisation reversal elective or fertility-related rather than medically necessary and may not cover it fully. Couples should inquire about total costs (surgery, hospital stay, anaesthesia, follow-up, fertility tests) and compare with other options (such as IVF) in terms of cost-benefit.
10. What questions should I ask my doctor or surgeon before opting for reversal of sterilisation?
Before proceeding, it's wise to ask:
-
What is my specific success rate given my age, health, partner fertility and previous sterilisation method?
-
What surgical technique do you propose and what is your experience (how many reversals have you done, what are outcomes)?
-
What are the risks of ectopic pregnancy or other complications in my case?
-
What is the expected recovery period and when can we try to conceive?
-
Are there alternative fertility options (like IVF) and how do they compare for me?
-
What is the full cost breakdown, and what follow-up care or additional fertility testing will be required?
-
If the reversal does not succeed, what steps do we take next?
Asking informed questions helps set realistic expectations and ensures you are choosing a path aligned with your fertility goals and personal circumstances.


